Oral and maxillofacial surgeons caring for patients who have sustained a nerve injury to a branch of the peripheral trigeminal nerve must possess a basic understanding of the response of the peripheral nerves to trauma. The series of events that subsequently take place are largely dependent on the injury type and severity. Regeneration of the peripheral nerve is possible in many instances and future manipulation of the regenerative microenvironment will lead to advances in the management of these difficult injuries.
Injury to the peripheral trigeminal nerve results in various extents of nerve fiber injury. The consequences to the patient are almost always detrimental and can influence the patient’s ability to eat comfortably, taste, manage oral secretions, and speak clearly. Many lingual and inferior alveolar nerve injuries require no surgical intervention and the patient’s sensation returns to normal with time. Other injuries show incomplete or no improvement with time. To compare these 2 types of clinical scenarios, the surgeon must first understand the response of the peripheral nerve to injury. The fate of the axons and/or the surrounding architecture of the nerve components is critical for recovery after injury. The healing of nerve injuries is unique within the body because it is a process of cellular repair rather than cell division or mitosis. The nerve cells at the site do not increase in number after an injury, but attempt to restore the axoplasmic volume and continuity of the original neurons.
Anatomy
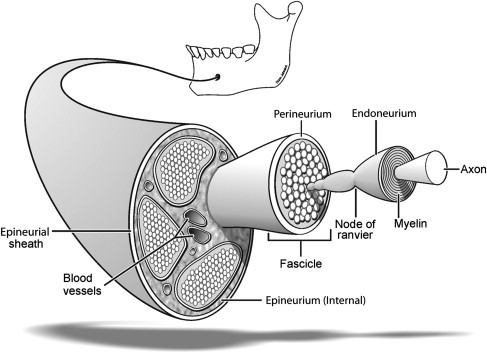
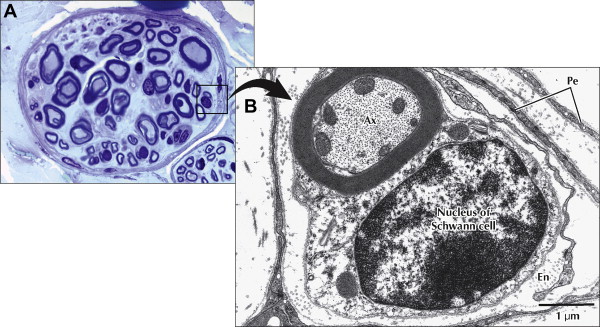
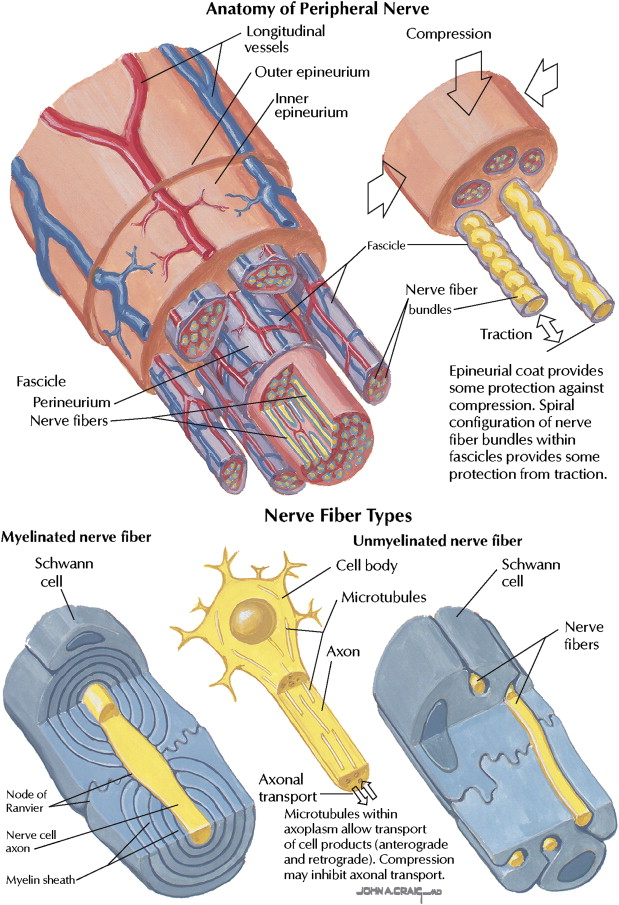
A sophisticated understanding of the anatomy of the peripheral nerve is beneficial to comprehending the series of events that takes place after an injury. A normal polyfascicular trigeminal nerve is shown in Fig. 1 . The components of the peripheral nerve include connective tissue, blood vessels, and the basic unit of the peripheral nerve: an axon and its associated Schwann cells. The nerve trunk represents a composite tissue constructed for the purpose of maintaining continuity, nutrition, and protection of these basic units, which require a continuous energy supply to allow for impulse conductivity and axonal transport.
Connective Tissue
The connective tissue subdivisions provide the framework around and within the nerve. The resulting architecture consists of an external and internal epineurium, and a perineurium surrounding each fascicle, in which are contained multiple axons surrounded by endoneurium. A fourth subdivision includes a mesoneurium that consists of loose areolar tissue continuous with the epineurium and the surrounding tissue bed. The mesoneurium allows the nerve to move a certain distance longitudinally within the surrounding tissue.
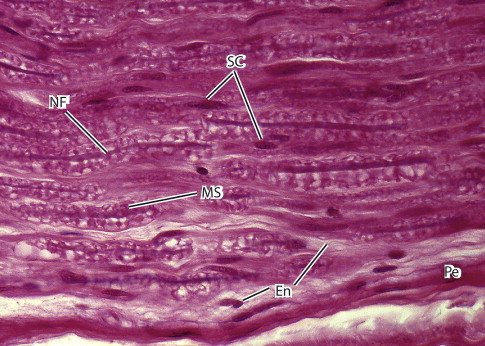
The outer connective tissue layer of the nerve is the external epineurium, which is a supporting and protective connective tissue made up primarily of collagen and elastic fibers ( Fig. 2 ). The internal epineurium is the structure that invests the fascicles, which contain the nerve fibers. Usually, several fascicles are grouped together in bundles, constituting well-defined subunits of the nerve trunk. Fascicles vary in size and quantity depending primarily on whether the region in question is at the proximal or distal site of the nerve. Both the lingual and inferior alveolar nerves are polyfascicular. The lingual nerve contains 15 to 18 fascicles at the region adjacent the mandibular third molar, whereas the inferior alveolar nerve contains 18 to 21 fascicles within the angle of the mandible.
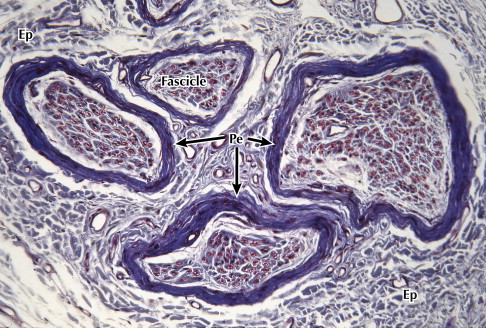
Each fascicle is surrounded by perineurium, a lamellated sheath with considerable tensile mechanical strength and elasticity ( Fig. 3 ). The perineurium is made up of collagen fibers dispersed among perineural cells and acts as a diffusion barrier as a result of its selective permeability, separating the endoneurial space within it from the surrounding tissues. This separation preserves the ionic environment within the fascicle.
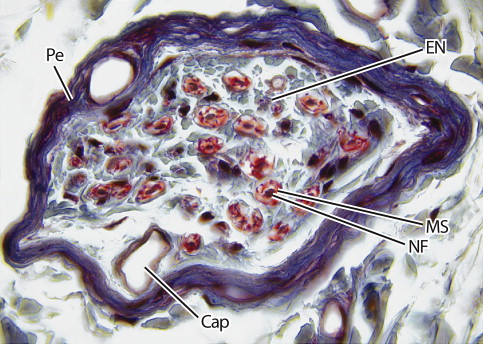
The nerve fibers are closely packed within endoneurial connective tissue (endoneurium) inside each fascicle ( Figs. 4 and 5 ). The endoneurium is composed of a loose gelatinous collagen matrix.
Blood Supply
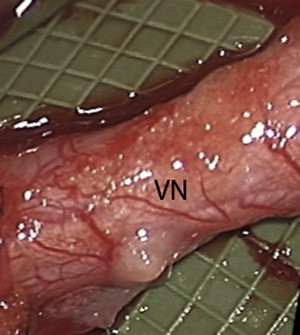
The axon of each neuron requires a continuous energy supply for impulse transmission and axonal transport. This energy is provided by extrinsic and an intrinsic vascular systems, which are interconnected. The extrinsic vessels enter the mesoneurium and communicate with the epineurial space via the vasa nervorum. A plexus develops at this level and runs longitudinally ( Fig. 6 ). Close examination of the fascicles reveals a large number of epineurial vascular branches, supplying each fascicle in a segmental manner, so that each fascicle is vascularly analogous to a complete axon ( Fig. 7 top).
The plexus enters the endoneurium through the perineurium at an oblique angle to anastomose with the intrinsic circulation that surrounds each fascicle. The oblique passage of vessels through the inner perineurial membrane is a site of potential circulatory compromise within the intrafascicular tissue.
Nerve Fibers
A neuron consists of a nerve cell body and its processes. There are several dendrites associated with the cell body and 1 long extension: an axon that travels to an end organ with branches terminating in peripheral synaptic terminals.
Nerve fibers can be either myelinated or unmyelinated (see Fig. 7 bottom). Sensory and motor nerves contain both types of fibers in a ratio of 4 unmyelinated to 1 myelinated.
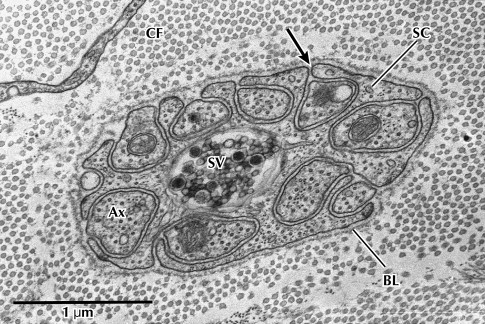
Unmyelinated fibers are made up of several axons enclosed by a single Schwann cell ( Fig. 8 ). Unmyelinated axons are small in diameter, usually averaging 0.15 to 2.0 μm.