Armamentarium
|
History of the Procedure
The pectoralis major myocutaneous (PMMC) flap has always been considered the workhorse flap for oral, head, and neck reconstruction. In 1979, Ariyan was the first to describe the use of the PMMC flap in head and neck reconstruction. Before Ariyan described its use for head and neck defect reconstruction, Pickerel and colleagues used the PMMC flap to reconstruct chest wall defects as a turnover flap to close sternal wounds. Ariyan described the use of the flap for reconstruction in 11 patients with oropharyngeal, cervicofacial, orofacial complex, orbit, and temporal defects. This work led to a lot of head and neck surgeons using this flap for primary reconstruction of head and neck defects. The current advancements with the successful use of vascularized free flaps, the use of the PMMC pedicled flap has decreased significantly. Currently, for head and neck reconstruction, the PMMC flap has been typically used as a salvage flap after failure of a free vascularized flap or in patients who are poor candidates for free flaps; alternatively they are used for reconstruction of large head and neck defects as a chimeric flap with a free vascularized flap. Despite this limited use, the flap remains a versatile and reliable option for head and neck reconstruction.
The main advantages of this flap are that it offers one-stage reconstruction, the patient’s position need not be changed during the procedure, and multiple skin paddles can be harvested to close complex defects.
Disadvantages of the flap are that one can lose muscle function due to weakness in arm adduction/rotation. Poor contour defects can be noted after the flap has been harvested over the chest wall, and a bulge is usually visible over the supraclavicular region due to the arc of the pedicle. This supraclavicular bulge can be prevented by dissecting the pedicle. In cases where the flap has been used to close a defect caused by a cancer ablation, the pectoralis muscle prevents visualization of any recurrences, making follow-up complicated. Serial computed tomography (CT) scans are used to rule out any tumor recurrences in these patients. In women, harvest of the flap can lead to asymmetry of the breast tissue, whereas in males, hair can grow over the skin paddle when placed intraorally. In males, the flap can be harvested without a skin paddle to avoid the problem of hair and bulkiness in the oral cavity.
Anatomy
The pectoralis is a large, fan-shaped muscle that covers the anterior chest wall, lying over the pectoralis minor, subclavius, serratus anterior, and the intercostal muscles on the anterior thoracic wall. Its origins are divided into a cephalic (clavicular) portion that attaches to the medial one third of the clavicle, a central (sternal) portion that arises from the sternum and the first six ribs, and a caudal (abdominal) portion that arises from the aponeurosis of the external oblique muscle portion. The muscle converges to form a tendon that attaches to the greater tubercle of the humerus and forms the axillary fold.
Laterally, the pectoralis major is closely associated with the medial aspect of the deltoid muscle, forming the deltopectoral groove, which consistently contains the cephalic vein. The superior surface of the pectoralis major is surrounded by a layer of deep cervical fascia. The inferior surface is separated from the pectoralis minor by the clavipectoral fascia. The clavipectoral fascia extends cephalad to insert into the inferior aspect of the clavicle, splitting just before its insertion to surround the subclavian muscle.
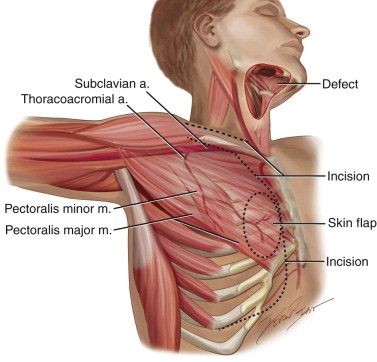
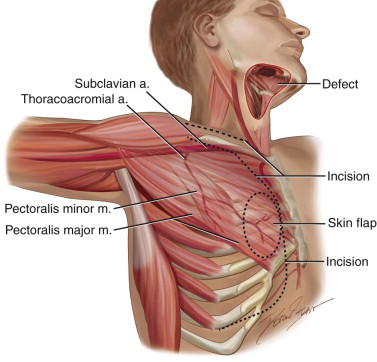
The blood supply to this muscle includes the pectoral branch of the thoracoacromial artery, the lateral thoracic artery, the superior thoracic artery, and the intercostal artery. The pectoralis artery supplies the pectoralis major and arises from the thoracoacromial artery, which in turn originates from the second portion of the axillary artery. The lateral pectoral artery is also contained within the neurovascular bundle, although it is not believed to contribute significantly to the blood supply of the muscle and often is sacrificed to improve the arc of rotation of the muscle. Both arteries are accompanied by their respective venae comitantes ( Figure 111-1 ).
The tendinous insertion of the pectoralis major on the greater tubercle of the humerus is sacrificed completely to improve the arc of rotation and to increase the effective length of the pedicle. The pectoralis major and overlying skin are supplied by the internal mammary perforators, which anastomose with the thoracoacromial artery branches. Thus, the medial aspect of the muscle is the most reliable area on which to design a skin paddle. Inferiorly, the skin overlying the muscle adjacent to the inferior rectus is supplied by the superior epigastric artery and is the least reliable for skin transfer. The total skin territory of the pectoralis major is almost 400 cm 2 , although it is rare to require such a large skin paddle for a head and neck reconstruction.
The medial (C5-C7) and lateral (C8-T1) pectoral nerves supply motor innervation to the muscle. The neurovascular bundles pass through the clavicular pectoral fascia en route to the deep surface of the muscle. The function of the pectoralis major is to adduct and medially rotate the arm. Motor branches from C5 and C6 supply the clavicular head while fibers from C7, C8, and T1 supply the sternocostal head of the pectoralis muscle. Sensory innervation is from the same spinal nerves through C5, C6, C8, and T1.
Indications for the Use of the Procedure
The PMMC flap can be used to reconstruct a variety of defects of the head and neck, defects that affect the oral cavity, as well as oropharyngeal, pharyngoesophageal, and skull base defects. In the oral cavity, the flap can be used to reconstruct the tongue, palate, floor of mouth, buccal mucosa, and segmental defects of the mandible.
For oral, head, and neck reconstruction, this pedicle flap may be used to close an orocutaneous fistula, cover an exposed carotid artery, add bulk to a radical neck dissection site, or restore complex defects with inner and outer epithelial linings. If the muscle flap is used to cover intraoral defects, the muscular surface mucosalizes without the use of a skin paddle. In patients with severe comorbidities, the PMMC can be used as an alternative to free vascularized flaps to close head and neck defects. The upper limit of this flap is usually cephalad to the level of the zygomatic arch.
Many authors have described the use of this flap as a myofascial, myocutaneous, or a myo-osseous flap. Myofascial and myocutaneous uses were described earlier. The use of the PMMC as a myo-osseous flap has also been described in the literature, although its utility is questionable. The flap is usually taken with a rib and used to reconstruct segmental defects of the mandible in addition to providing soft tissue coverage for intraoral or extraoral defects simultaneously. Its advantage is that the curvature of the rib resembles the curvature of the mandible. Combining a rib graft with a PMMC flap, however, does have limitations, including resorption of the graft, pain at the donor site, an increased length of hospital stay, and an increased failure rate. The PMMC flap may also used to close chest/sternal wounds after cardiothoracic surgery.
History of the Procedure
The pectoralis major myocutaneous (PMMC) flap has always been considered the workhorse flap for oral, head, and neck reconstruction. In 1979, Ariyan was the first to describe the use of the PMMC flap in head and neck reconstruction. Before Ariyan described its use for head and neck defect reconstruction, Pickerel and colleagues used the PMMC flap to reconstruct chest wall defects as a turnover flap to close sternal wounds. Ariyan described the use of the flap for reconstruction in 11 patients with oropharyngeal, cervicofacial, orofacial complex, orbit, and temporal defects. This work led to a lot of head and neck surgeons using this flap for primary reconstruction of head and neck defects. The current advancements with the successful use of vascularized free flaps, the use of the PMMC pedicled flap has decreased significantly. Currently, for head and neck reconstruction, the PMMC flap has been typically used as a salvage flap after failure of a free vascularized flap or in patients who are poor candidates for free flaps; alternatively they are used for reconstruction of large head and neck defects as a chimeric flap with a free vascularized flap. Despite this limited use, the flap remains a versatile and reliable option for head and neck reconstruction.
The main advantages of this flap are that it offers one-stage reconstruction, the patient’s position need not be changed during the procedure, and multiple skin paddles can be harvested to close complex defects.
Disadvantages of the flap are that one can lose muscle function due to weakness in arm adduction/rotation. Poor contour defects can be noted after the flap has been harvested over the chest wall, and a bulge is usually visible over the supraclavicular region due to the arc of the pedicle. This supraclavicular bulge can be prevented by dissecting the pedicle. In cases where the flap has been used to close a defect caused by a cancer ablation, the pectoralis muscle prevents visualization of any recurrences, making follow-up complicated. Serial computed tomography (CT) scans are used to rule out any tumor recurrences in these patients. In women, harvest of the flap can lead to asymmetry of the breast tissue, whereas in males, hair can grow over the skin paddle when placed intraorally. In males, the flap can be harvested without a skin paddle to avoid the problem of hair and bulkiness in the oral cavity.
Anatomy
The pectoralis is a large, fan-shaped muscle that covers the anterior chest wall, lying over the pectoralis minor, subclavius, serratus anterior, and the intercostal muscles on the anterior thoracic wall. Its origins are divided into a cephalic (clavicular) portion that attaches to the medial one third of the clavicle, a central (sternal) portion that arises from the sternum and the first six ribs, and a caudal (abdominal) portion that arises from the aponeurosis of the external oblique muscle portion. The muscle converges to form a tendon that attaches to the greater tubercle of the humerus and forms the axillary fold.
Laterally, the pectoralis major is closely associated with the medial aspect of the deltoid muscle, forming the deltopectoral groove, which consistently contains the cephalic vein. The superior surface of the pectoralis major is surrounded by a layer of deep cervical fascia. The inferior surface is separated from the pectoralis minor by the clavipectoral fascia. The clavipectoral fascia extends cephalad to insert into the inferior aspect of the clavicle, splitting just before its insertion to surround the subclavian muscle.
The blood supply to this muscle includes the pectoral branch of the thoracoacromial artery, the lateral thoracic artery, the superior thoracic artery, and the intercostal artery. The pectoralis artery supplies the pectoralis major and arises from the thoracoacromial artery, which in turn originates from the second portion of the axillary artery. The lateral pectoral artery is also contained within the neurovascular bundle, although it is not believed to contribute significantly to the blood supply of the muscle and often is sacrificed to improve the arc of rotation of the muscle. Both arteries are accompanied by their respective venae comitantes ( Figure 111-1 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


