This article reports the successful treatment of a patient with the unusual occurrence of bilateral and multiple dentigerous cysts of the premolars. One impacted mandibular premolar was moved by traction orthodontically. On the opposite side, the impacted premolar was autotransplanted after space was created through mesial movement and hemi-sectioning of the neighboring molars. The impacted maxillary premolar was extracted. Miniscrews were additionally used for anchorage reinforcement to prevent unintended counteractions and solve the problem of space management after autotransplantation. We also reviewed the clinical implications of the diagnosis, planning, and treatment of cyst-associated impacted teeth in young adult patients.
Dentigerous cysts are major pathologic entities found in dentistry, accounting for approximately 24% of all true cysts in the jaws. The cyst involves the odontogenic epithelia of impacted permanent teeth, supernumerary teeth, odontomas, and, rarely, deciduous teeth. The mandibular third molars are the most frequently involved, although there is a marked incidence among mandibular second molars and premolars. Even though the development of cysts can be responsible for structural changes in the bone, root resorption, and abnormal dentition development, there is usually no pain or discomfort associated with a cyst. Therefore, dentigerous cysts are frequently discovered when radiographs are taken to investigate delayed tooth eruption, a missing tooth, or malalignment. Most dentigerous cysts are single lesions. Meanwhile, bilateral and multiple cysts are rare and occur typically in association with syndromes such as cleidocranial dysplasia, Maroteaux-Lamy syndrome, and basal cell nevus syndrome. In the absence of these syndromes, bilateral dentigerous cysts located in the mandible are uncommon, with few reports.
Regarding orthodontic treatment for an impacted tooth with a dentigerous cyst, conventional treatment techniques have some limitations, including the age of the patient, tooth depth, tooth inclination, and eruption space. In some cases, extraction of the impacted tooth might be required, especially in adult patients. The autotransplantation of teeth has been widely used in orthodontics to provide a treatment alternative in many situations, mainly in patients with a severe impaction, early loss of permanent teeth, or congenital aplasia. Recently, the orthodontic miniscrew has provided rigid anchorage, made treatment more efficient, and also made biologically permissible movements possible. As a consequence, miniscrew use could change the treatment paradigm and extend the scope of orthodontic mechanotherapy.
In this article, we report the successful treatment of a patient with the unusual occurrence of nonsyndromic bilateral and multiple dentigerous cysts, in which the mandibular left first molar was severely damaged. Combined treatments, including extraction, marsupialization, orthodontic traction, and tooth autotransplantation, were performed for the impacted premolars. Additionally, miniscrews were used to bring the transplanted premolar to a suitable position in the mandibular arch for favorable occlusion. Our treatment included a consideration of the guidelines for multiple dentigerous cysts associated with mandibular premolars and molars in young adults.
Diagnosis and etiology
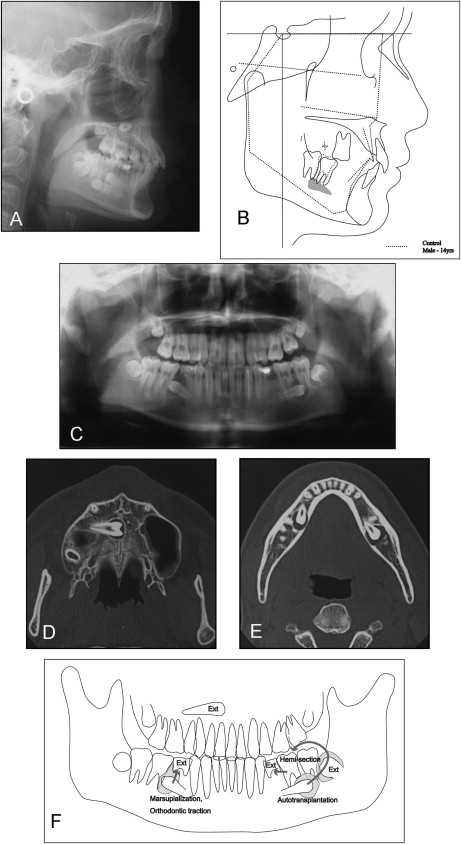
A boy, aged 13 years and 8 months, was examined in the outpatient clinic of Okayama University Hospital in Japan. A general dentist pointed out the impacted premolars and introduced him to us at Okayama University Hospital in Okayama, Japan. He had a symmetrical face, a straight profile, and an obtuse nasolabial angle. The patient’s medical history showed nothing unusual. There were no associated syndromes. Intraoral examination showed the remaining mandibular second deciduous molars, missing second premolars, a diastema, a deep overbite, and a unilateral scissors-bite involving the left second molar ( Figs 1-3 ). The pretreatment panoramic radiograph and computed tomography scan ( Fig 3 , C-E ) showed a well-defined radiolucent area surrounding the crown of the unerupted mandibular second premolars, the mandibular left third molar, and the maxillary right second premolar. The distal root of the mandibular left first molar was rebsorbed due to a dentigerous cyst associated with the mandibular left second premolar ( Fig 3 , C ). The maxillary left second premolar was congenitally absent.
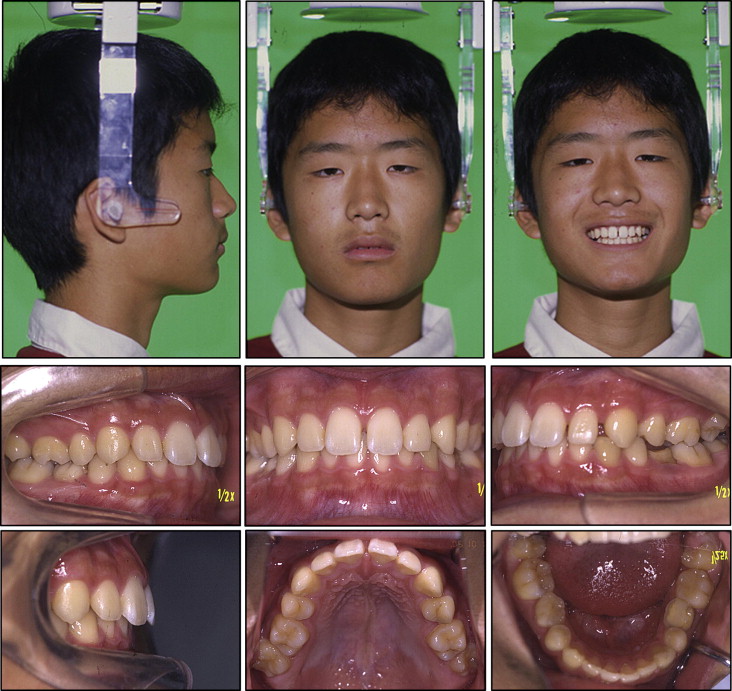
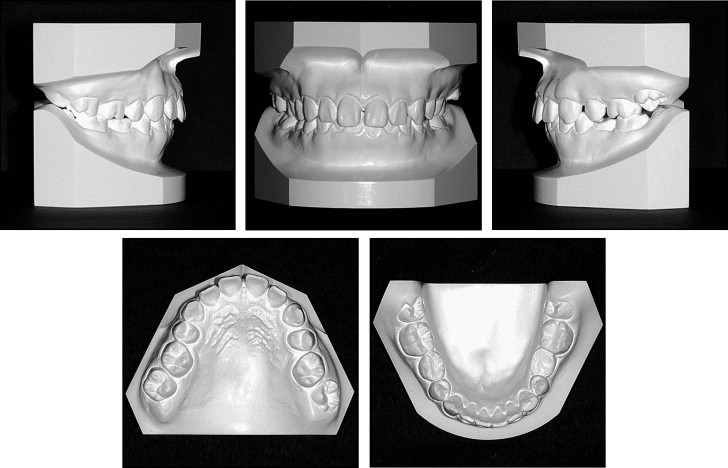
When compared with Japanese norms, the cephalometric analysis showed a tendency toward a skeletal Class III relationship (ANB, 1.2°) with mandibular excess (SNB, 82.0°; Ar-Go, 64.6 mm; Go-Me, 82.2 mm) ( Table I ), a low mandibular plane angle (Mp-FH, 12.7°), and an acute gonial angle (106.9°). The mandibular incisors were proclined relative to the mandibular plane (L1-Mp, 106.0°). The molar relationships were Class II on both sides. The maxillary dental midline was almost coincident with the facial midline, but the mandibular midline was shifted 2.0 mm toward the left. The maxillary anterior teeth were spaced. The patient showed no significant symptoms of a temporomandibular disorder. The incisal path was unstable during opening-and-closing jaw movements with a 6 degrees-of-freedom jaw movement recording system (Gnathohexagraph system, version 1.31; Ono Sokki, Kanagawa, Japan). The interincisal distance on maximal opening without pain was 37 mm. An occlusal force of 776 N and an occlusal contact area of 16.6 mm 2 ( Table II ) were calculated on an occlusal-force recording system (Dental Prescale & Occluzer; Fuji Film, Tokyo, Japan).
| Variable | Mean | Initial | Pre-edgewise | Posttreatment |
|---|---|---|---|---|
| Angular (°) | ||||
| ANB | 3.2 | 1.2 | 1.1 | 0.5 |
| SNA | 81.5 | 83.3 | 83.3 | 83.3 |
| SNB | 78.2 | 82 | 82.2 | 82.8 |
| Mp-FH | 28 | 12.7 | 10.6 | 9.5 |
| Gonial angle | 120.9 | 106.9 | 105.4 | 105.9 |
| U1-FH | 112.4 | 103.1 | 114.7 | 110.8 |
| L1-Mp | 95.2 | 106 | 103.7 | 110.7 |
| IIA | 124.2 | 134 | 131 | 129 |
| Occlusal plane | 15.5 | 10.5 | 7.5 | 10.7 |
| Linear (mm) | ||||
| S-N | 72.2 | 76.3 | 77.7 | 77.7 |
| N-Me | 135.7 | 135.4 | 136 | 137.3 |
| Me/NF | 74.6 | 71 | 71.2 | 72.1 |
| Ar-Go | 53.2 | 64.6 | 67.3 | 70.1 |
| Ar-Me | 115.6 | 123.1 | 126.5 | 129 |
| Go-Me | 76.6 | 82.2 | 84 | 86 |
| Overjet | 3.3 | 4.1 | 4.3 | 2.2 |
| Overbite | 3.3 | 6.7 | 6.1 | 3.8 |
| U1/NF | 32.4 | 34.1 | 31.3 | 32 |
| U6/NF | 26.2 | 26.7 | 26.3 | 27 |
| L1/Mp | 48.9 | 45.4 | 46.4 | 44.5 |
| L6/Mp | 37.5 | 38.1 | 38.9 | 40.2 |
| Occlusal force (N) | Occlusal contact area (mm 2 ) | Maximun opening (mm) | |
|---|---|---|---|
| Initial | 776 | 16.6 | 37 |
| Pre-edgewise treatment | 589 | 13.7 | 49 |
| Posttreatment | 1153 | 24.4 | 48 |
Treatment objectives
The patient was diagnosed with an Angle Class II malocclusion, a skeletal Class III jaw-base relationship, and multiple dentigerous cysts associated with the second premolars and the mandibular left third molar. The principal objectives were to create spaces for the unerupted mandibular second premolars, then bring them into the arch by using appropriate surgical techniques, and achieve acceptable occlusion with ideal overjet and overbite. The outline of the initial treatment plan is shown in Figure 3 , F . The distal root of the mandibular left first molar, which was rebsorbed by the dentigerous cyst, underwent hemi-sectioning. Concerning the mandibular right second premolar, we selected orthodontic traction after marsupialization of the cyst. In contrast, the mandibular left second premolar was brought into the arch by autotransplantation. A miniscrew was implanted to move the hemi-sectioned mandibular left first molar mesially, isolate it from the impacted teeth, and produce adequate space for autotransplantation of the impacted mandibular left second premolar.
Treatment objectives
The patient was diagnosed with an Angle Class II malocclusion, a skeletal Class III jaw-base relationship, and multiple dentigerous cysts associated with the second premolars and the mandibular left third molar. The principal objectives were to create spaces for the unerupted mandibular second premolars, then bring them into the arch by using appropriate surgical techniques, and achieve acceptable occlusion with ideal overjet and overbite. The outline of the initial treatment plan is shown in Figure 3 , F . The distal root of the mandibular left first molar, which was rebsorbed by the dentigerous cyst, underwent hemi-sectioning. Concerning the mandibular right second premolar, we selected orthodontic traction after marsupialization of the cyst. In contrast, the mandibular left second premolar was brought into the arch by autotransplantation. A miniscrew was implanted to move the hemi-sectioned mandibular left first molar mesially, isolate it from the impacted teeth, and produce adequate space for autotransplantation of the impacted mandibular left second premolar.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


