10.1055/b-0034-84408
Diagnostics and Epidemiology: 5 Visual–Tactile Detection and Assessment
The terms detection and assessment with respect to caries lesions have not been widely adopted so far. Instead the term diagnosis is used to describe the result of the clinical and radiographic examination. The current international glossary of key terms states that1:
- Lesion detection implies a process involving the recognition (and/or recording), traditionally by optical or physical means, of changes in enamel and/or dentin, and/or cementum, which are consistent with having been caused by the carious process.
- Lesion assessment is the assessment of the characteristics of a carious lesion, once it has been detected. These characteristics may include optical, physical, chemical, or bio-chemical parameters, such as color, size, or surface integrity and its activity status.
- Caries diagnosis should imply the human professional summation of all the signs and symptoms of disease to arrive at an identification of the past or present occurrence of the disease, caries (see Chapter 9).
Looking up the word diagnosis in the dictionary, one will find that it originates from the two Greek words: “dia” which corresponds to “through,” and “gnosis” which corresponds to “knowledge.” Consequently, it is only through knowledge about diseases that the professional summation or the correct diagnosis can be established.2 Hence Chapters 1–4 have informed about the structure of the teeth, the etiology, and pathogenesis of caries on histological and clinical levels as well as the caries process depicted as a theoretical model.
It follows from the above, then, that diagnosis is a process.3 Here, several signs and symptoms of a disease (as caries) are detected and assessed by means of different qualitative or quantitative methods or tools. Basically, for caries the diagnostic process either leads to the assumption that the lesion is likely to progress or not. In the first case, further loss of mineral is expected, if relevant factors of the disease are not changed4, and either a non-, micro-, or minimal-invasive treatment should then be performed. The therapy that offers the best prognosis to prevent lesion progression without damaging too much sound and diseased hard tissue should be advocated. If the diagnostic process leads to the assumption that the lesion is arrested, no further mineral loss would be expected under the current oral conditions. In consequence, no cariologic treatment is currently necessary (Chapters 9 and 20)4.
NOTE
Detection and assessment of various signs and symptoms of a disease are summarized together with other parameters to reach a diagnosis.
In this chapter we will begin by introducing the visual–tactile method, the main tool for the clinical part of the diagnostic process. The next chapter will deal with radiographs and other caries detection methods. The visual–tactile method comprises the use of the eye and a thin explorer, the latter is said to “lengthen the eye of the examiner.” Hereby a caries lesion can be:
- Detected, which implies a subjective method of determining whether or not a caries lesion is present
- Assessed according to severity status (depth)
- Assessed according to activity status
NOTE
Visual–tactile examination of the teeth is just one of several detection and assessment methods for caries, but still the most important.
In detail, this chapter will cover:
- Requirements for visual–tactile examination of the teeth
- Visual–tactile indices to record or score caries lesions
- Relationships between visual signs of caries and the histological depth
- How to assess activity status of caries lesions
- Differences between caries and other diseases of the tooth hard substance
General Remarks
Caries develops where a cariogenic biofilm accumulates. In consequence, caries most often develops next to gingival margins, cervical to approximal contact areas, and in the grooves and fossae of the occlusal surfaces. Caries is very seldom seen on the incisal edge or at the cusps of teeth. In elderly people root caries can frequently be observed where the gingiva is recessed.
Basically, primary caries, which is caries on unrestored surfaces and caries adjacent to a restoration (old terminology: secondary caries or recurrent caries), can be observed both on crowns and roots. Residual caries means that demineralized tissue, often dentin, was left behind for some reason before a restoration has been placed.
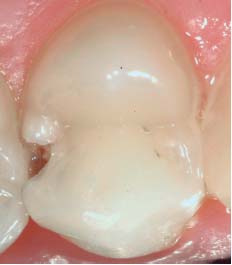
Good light as well as clean and dry teeth are required when examining for caries and other dental hard tissue defects.4–5 These are particularly important to identify early stages of caries3–6 ( Fig. 5.1 ). Professional tooth cleaning can be performed by means of rotating brushes or simply by manual toothbrushing. Approximal surfaces are most easily cleaned by flossing. Cotton rolls are placed in the maxillary sulci to control saliva from the parotid glands. Suction and/or cotton rolls might be used lingually as supplement. Each tooth is then examined, starting for example in the maxilla in the right side of the mouth on the most posterior tooth (tooth 18). Distal, occlusal, oral, buccal, and finally the mesial/distal interproximal surfaces are examined separately under clean and dry conditions. The examination proceeds in the anterior direction, completing first the upper and then the lower arch. A thin probe and a dental mirror are needed. Visually, color changes compared with the appearance of structurally sound teeth are noticed; tactilely, irregularities in the morphology of the tooth surface are sensed.

Thus, changes in color compared with the appearance of structurally sound teeth can be seen, while irregularities in the morphology of the tooth surface can be felt.
ERRORS AND RISKS
Too hard probing in demineralized dental hard tissue can provoke defects7 ( Fig. 5.1c vs. Fig. 5.1d ), which can ease cariogenic biofilm formation and further caries progression.
During recent years it has been increasingly popular for dental professionals to use magnifying glasses. It has been be assumed that magnification increases the accuracy of detection and assessment of caries lesions, in particular of initial ones. However, studies show inconclusive results with respect to improvement in caries examination by using magnification compared to the naked eye.8,9
Histological and Clinical Features of Caries
Coronal Caries Lesions
Caries on the crowns mainly develops in the groove–fossa system (fissure system), on the approximal and the smooth surfaces near the gingival margins. Early stages of caries on approximal surfaces are hidden from visual inspection due to the adjacent tooth. Caries in the groove–fossa system develops most often at the entrance to the fissure parts and in the bottom part of the grooves. However, after cleaning and drying, initial and also more mature stages of occlusal caries lesions can be visually identified.3,10,11
Wherever a cariogenic biofilm is established, signs and subsequently symptoms (tenderness or pain) of caries may become evident. The first changes recognized visually are changes in color from yellowish white to chalky white. If the carious challenge continues, the white area becomes more obvious in time. In the next stage small breakdowns (discontinuations/microcavities) occur in the enamel and/or a dark shadow due to underlying carious dentin is observed. This stage is followed by different sizes of breakdown of enamel and also parts of the dentin. Eventually the surface/tooth is completely destroyed due to the demineralization process ( Fig. 5.2 , Fig. 5.11 ). If progression stops at an early stage, very often the whitish appearance, in particular on the occlusal surfaces, discolors (brownish) and stays like that as a scar ( Fig. 5.2 ).
The change in color from yellowish white to chalky white can be explained by dissolution of mineral. Consequently, the intercrystalline spaces will be bigger and the pore volume increases. Hereby light will be scattered, which is recognized visually as an opaque area that is different from the surrounding translucent sound enamel. This phenomenon can be explained physically by the different refractive indices of various media/structures. Air has a refractive index (RI) of 1.0, water/saliva of 1.33, and enamel of 1.62.12,13 If, in the laboratory, a liquid (e.g., quinoline) with a refractive index of 1.62, being similar to that of the surrounding sound enamel, is applied onto a white spot caries lesion, the lesion will disappear (see Chapter 3). Clinically, we can only dry the lesions and re-wet them with water to identify small lesions with a very low increase in pore volume. After drying, a caries lesion that is normally ‘bathed in saliva’ will be more distinctively visible, since the RI in the most demineralized parts is now changed to 1.0. After applying water the RI in these pores will again (similarly to saliva) increase to 1.33; the lesion is no longer visible, or at least less. If whitish, these initial caries lesions on enamel are called white spots. Stains arising from nutrition or smoking might change these into brown spots over time.
NOTE
If a caries lesion is clinically visible without air-drying, relatively more mineral has been dissolved compared with those caries lesions that require air-drying to become visible.


When acids reach the dentin they will dissolve the mineral in the dentin. Demineralized dentin varies in color from that of sound dentin—it appears more yellowish or brownish ( Fig. 5.3 ). Sometimes the change in color can be seen through the overlying enamel as a shadow ( Fig. 5.4 ). Thus, if a shadow from the underlying dentin can be identified, demineralization of the dentin has taken place. It is important to emphasize that demineralized dentin is not the same as dentin harboring microorganisms, or even biofilms. As long as the caries lesion is not cavitated, occasionally single microorganisms, but not established biofilms, will be present within the lesion. If the lesion is cavitated, larger numbers of microorganisms enter into the enamel and may build up cariogenic biofilms there as well.14,15 Microcavities are cavities in outer parts of the demineralized enamel that covers the demineralized dentin. If all the enamel is gone, this is called a dentin cavitation.16
CLINICAL PEARL
Breakdown of tooth structure due to caries can clinically be verified by gently drawing a probe across the area (feeling).



Caries lesions on approximal surfaces are often obscured by the adjacent tooth surface, which hinders adequate visual examination. Placement of an orthodontic elastic band (0.8 mm) for two days (Fig. 5.5) creates some space, large enough to examine both approximal surfaces visually and tactilely. High interrater-reproducibility when assessing cavitation status has been reported for this technique.17 Few patients seem to experience discomfort when using separators.18 Nevertheless, in dental practice this method does not seem to be adopted on a large scale owing to two patient visits being needed. The use of a thin probe without prior separation or a floss (a floss will crack if it is run over a cavity) might be of help at least to distinguish between cavitated and noncavitated approximal lesions.
Root Caries Lesions
Caries on the roots will only develop when the gingiva is recessed due to either inflammation or trauma (e.g., following incorrect toothbrushing). Even normal brushing will then abrade the cementum covering the root dentin. If a cariogenic biofilm is frequently established in these areas, apatite crystals will be dissolved and the dentin will change in color and texture. Root caries pathogenesis differs slightly from that of enamel, since caries in dentin follows the tubules. Microorganisms will quite easily penetrate into these, already in the very early stages of root caries formation. Preformed sclerotic dentin as well as access to saliva and gingival fluid may slow down the progression rate. Nonetheless, root caries also tends to circle around the neck of the tooth rather than to penetrate very deeply into the tissue. As for enamel, root caries lesions will first be noncavitated ( Fig. 5.6 ).
CLINICAL PEARL
When sound dentin is probed, the texture feels hard. Demineralized dentin is softer than sound dentin, which can be sensed with the probe. Often the dentin feels sticky, which means that the dental professional has to pull back the probe.

Caries Adjacent to Restorations
Caries adjacent to or at the margin of restorations ( Fig. 5.7a, b ) has many designations, for example, secondary caries to distinguish it from primary caries and recurrent caries to reflect the results of lack of plaque control. The preference in this chapter is caries adjacent to restorations (CAR), which relates to the supposition that CAR in principle follows the pathogenesis delineated for primary caries, whether coronal or in root dentin.19–21 From histological examination it has been suggested to describe the CAR enamel lesion in two parts: an outer primary lesion next to the restoration, and a wall lesion between the restoration and the cavity. Initially in enamel and dentin lesions, the wall lesion is narrow, but when the lesion reaches the enamel–dentin junction (EDJ) there may be some lateral spread. The outer primary enamel lesion is a subsurface lesion, which spreads further into the enamel following the directions of the prisms. When the lesion reaches the EDJ, dentin demineralization occurs mainly along the affected dentinal tubules. The initial root CAR lesion also follows the shape of the dentinal tubules.
In addition, a restoration can be imperfect, possibly loose ( Fig. 5.7c ), and then traps plaque, which can lead very quickly to development of caries.
Indices for Clinical Recording of Caries Lesions
Numerous indices for visual/tactile recording of various stages of caries lesions, restorations, and sealants have been described. The reliability in terms of intra- and interrater-reproducibility of the individual indices is often expressed in kappa values. To ease readability of this paragraph the reliability of the individual indices will be graduated according to the three following levels (modified from Landis and Koch22) Thus, if a recording system has the following “scores,” , , this means that both intra- and interrater-reproducibility are almost perfect ( Table 5.1 ).
Historical Perspective
Numerous classification systems to record caries have been developed over the years.23 Each system fulfilled a particular aim, such as to be used in epidemiological investigations, clinical studies, or for daily use in clinical practice.
In the past 50 years a system for epidemiological investigations advocated by the World Health Organization , has been widely adopted.24 Here, only caries at the cavity level—a quite late stage of the disease ( Fig. 5.8 )—is reported. This is understandable, as the system was primarily developed to record caries under field conditions, without cleaning and drying of the teeth, and using nonprofessional light sources. As caries is recorded at the cavity level, there are no good reasons to have codes for either active or arrested caries lesions, as all cavitated lesions in this system are regarded as being active. Another system (RadikeX,)25 also only scores caries at the cavity level or for those caries lesions where the probe is caught.
The modern approach is to prevent caries before it requires restorations, and therefore it is necessary to record initial, noncavitated stages as well as cavitated stages.X,X, 27,,28,,29,. Such indices may also be used in clinical trials where small changes within short periods from baseline to final examination need to be recorded. Table 5.2 shows the scoring system used by Kuzmina et al.28 where primary caries is divided into four scores: 1 = initial, noncavitated caries; 2 = caries with microcavitation; 3 = caries with dentin cavitation; and 4 = deep dentin caries.
Figure 5.9 shows a formula used for recording primary caries and CAR, root treatments, and extractions due to caries on children in the Public Child Dental Health Service in Denmark.30–31 This system, , , has been used since the 1970s on a daily basis by both dentists and dental hygienists. This recording system was amongst the first where scores for a whole child population could be transferred to a computer, where mean dmfs/t-DMFS/T and percentages of children with dmft-DMFT = 0 could be expressed at the individual level, and at the municipality, county, and national levels.
There are several other recording systems worth mentioning, also covering root caries; however, they are linked to the depth of the lesions evaluated histologically and/or the activity state of the lesions. These will be discussed in the following paragraphs.

NOTE
Traditional caries indices have focused on lesions at the cavitation (into dentin) level. More recent ones include the recording of noncavitated caries lesions. The majority of indices have not been adequately evaluated scientifically, although reproducibility seems to be quite good for most of them.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses








