The purpose of this article is to review and discuss the advances in the management of children born with cleft lip and palate (CLP) as it has evolved over the past 100 years. This overview is based on articles published in the American Journal of Orthodontics , which frequently changed its name, over the past century. Additionally, other journals will be cited as craniofacial anomalies became recognized during the 20th century and the biologic basis became refined, with the new discipline of genetics replacing the term hereditary and its connotations of eugenics. The Human Genome Project, completed in 2003, has now provided an understanding of syndromic and nonsyndromic CLP that has led to advances in the diagnosis and treatment of CLP in the 21st century. These evolving concepts will be discussed in an overview of the types of procedures published from 1915 to 2015 and the major transition in the mid-20th century from multiple uncoordinated interventions from various specialists to a coordinated team approach in which the orthodontist has a specific role in the timing and sequencing of interdisciplinary treatment goals. Major technologic advancements in treatment modalities and the contemporary approach to the health-related quality of life of the patient and the caregiver have resulted in their participation in treatment options and decisions. The requirement of informed consent reflects the legal doctrine that now emphasizes the ethical imperative of greater respect for patient autonomy in the decision-making process. The orthodontist no longer makes decisions alone, but rather with the team and the patient or the caregiver.
Highlights
- •
Management of children born with cleft lip and palate (CLP) has evolved over 100 years.
- •
The biologic basis for studying craniofacial anomalies has been refined.
- •
The Human Genome Project provides understanding of syndromic and nonsyndromic CLP.
- •
Patients and caregivers have greater participation in treatment decisions.
- •
Orthodontists work with team members and the patient or caregiver.


Becoming familiar with a century of orthodontic publications relating to orofacial clefts and other craniofacial anomalies has been a rewarding and educational pursuit. Issues relating to the diagnosis, treatment, and probable causes of orofacial clefting have shown remarkable progress in the second half of the 20th century, with advances in anesthesia and control of infection with the advent of antibiotics. The term heredity has been replaced by the evolving concepts of genetics and genomics with the unraveling of the human genome early in the 21st century. The role of the orthodontist in the clinical management of orofacial clefts differs from a typical 2-year comprehensive orthodontic treatment by extending treatment from the neonatal period with treatment of displaced alveolar segments, to management of the skeletal and dental components of the developing dentition starting with the deciduous dentition, through treatment of the mixed dentition and into adolescence and adulthood. This continuum of treatment not only exhausted the patient and caregiver, but also, with a lack of communication between all involved specialists, affected the timing and sequencing of treatment. An interdisciplinary approach fostered collaboration with other specialties including surgeons and speech pathologists. While the orthodontist’s role is central to the overall management of children born with orofacial clefts, a close collaboration with surgeons, speech and language pathologists, geneticists and dysmorphologists, and paramedical specialists is imperative for team care. The team concept was not formalized until the 1940s, but the literature starting in 1915 reflects the influence of interdisciplinary management with orthodontists and their colleagues and collaborators. This interactive theme is reflected in the name of the journal that started as the International Journal of Orthodontia in 1915 but was followed by the International Journal of Orthodontia and Oral Surgery (1919-1921), with the articles having a strong surgical influence in the correction of cleft lip and palate (CLP). The publications frequently reported a collaborative approach with the orthodontist, approximating the cleft segments for ease of surgical repair followed by expansion to establish the occlusion. Closing the palatal cleft was a challenge, and the prosthodontist or orthodontist constructed obturators with various materials before the advent of acrylic. A publication by Calvin Case in 1921 addressed prosthetic correction of speech in patients with CLP with a velum obturator constructed from black vulcanite that would approximate the anterior pharyngeal wall opposite the atlas vertebra. This appliance facilitated producing the phonetic components of speech, as “speaking correctly” was a high priority.
The influence of emerging radiology techniques with the dawning of an era of cephalometrics changed the journal’s name to be more inclusive to International Journal of Orthodontia, Oral Surgery and Radiology (1922-1932). In 1932, surgeons Kiskadden and Tholen from Los Angeles published an article on primary and secondary repair of the lip in which they condemned the removal of the premaxilla in “double harelip” to allow closure of the soft tissues. Davis, in 1932, reported that 80% of palatoplasty results in failure with poor speech, and the facial appearance of these patients leads to ridicule. The enlightened school system in California had speech training available for all children in 1932, and speech therapy was considered possible whatever the deformity, if the child was “disciplined and put in the appropriate effort.” Lip repair at this time was advocated to be done 24 hours after birth, and Brophy supported the need for contact of the cleft alveolar segments before surgical closure with his compression appliance and primary bone grafting.
As other specialties in dentistry became recognized, so the orthodontist collaborated with the pedodontist or pediatric dentist, and the journal changed its name to the International Journal of Orthodontia and Dentistry for Children (1933-1935). The journal returned again to include oral surgery as the International Journal of Orthodontia and Oral Surgery (1936-1937) before relinquishing the international title to become the American Journal of Orthodontics and Oral Surgery (1938-1947).
The treatment of cleft palate was limited to obturators until anesthesia became available in the 19th century, at which time surgical repair became a reality. In 1937, Ivy reviewed the recent literature on CLP surgery in the American Journal of Orthodontics and Oral Surgery and provided insights into eugenics and heredity (genetics had not yet been established as a replacement for heredity ). He quoted Häntzschel, who concluded from his research “that sterilization of all individuals with these clefts should be promoted, in order to cut off from the complicated recessive heredity pathway an invisible uncontrollable propagation of the disease stock.” These words and this doctrine are inconceivable in the 21st century but are part of the history of the treatment and management of CLP and the recognition that there was a genetic inheritance. The discovery of anesthetics had promoted advancements in surgical techniques, but there was still a problem with infection until antibiotics in mid-20th century controlled infection and resulted in increased success of surgical procedures.
Facial growth and development of children born with orofacial clefts had the stigma of facial deformity that was to be later studied with serial cephalograms from birth to adulthood. The outcome of early surgical and orthodontic interventions could be measured and compared with serial lateral skull cephalograms during the child’s development. The controversy that has continued over the last century about the optimal timing of orthodontic and surgical interventions has focused on growth of the nasomaxillary complex. Facial esthetics have already been compromised by the midface deficiency and the facial scars from nasolabial surgical repair. When Ross and Johnson reported their cephalometric study in 1968 to evaluate the effect of early orthodontic treatment (before the eruption of the permanent dentition) on facial growth, they concluded that it had no significant effect. For most children with unilateral CLP, orthodontic treatment before the eruption of the permanent dentition had no appreciable effect on the facial growth pattern.
Although interest in the treatment of patients with CLP continued with articles published in orthodontic journals, the specialty of oral surgery had advanced rapidly after the end of the World War II in 1945. Elective orthognathic surgery with correction of dentofacial deformities was a recognized specialty of oral and maxillofacial surgery that required its own journal. The journal changed its name again but this time to exclusively embrace the first specialty in dentistry and became the American Journal of Orthodontics (1948-June 1986). Major advances were being made in science and technology, and a new concept, prevalent in Europe, was to modify and redirect growth by dentofacial orthopedics with functional appliances. As these became popular in the United States, a further modification to the title of the journal was made; it became the current American Journal of Orthodontics and Dentofacial Orthopedics ( AJO-DO ) (July 1986-present).
The first 50 years, 1915-1965
Interestingly, the same issues that have engaged those involved in providing treatment for children with CLP recur in the 21st century. These controversies relate to the timing and sequencing of treatment and the influence of the treatment intervention on the growth and development of the child’s nasomaxillary complex. Orthodontists were concerned that early surgical repair of the palate would affect maxillary growth and development, but delaying palatal closure was opposed by speech and language pathologists. The premise was that early closure of the hard and soft palates would restore the velopharyngeal mechanism to promote intelligible speech with normal development of the phonetic components of language. Additionally, ear infections and recurrent otitis media affected the child’s hearing and consequently the development of speech. From the patient’s and caregiver’s perspectives, the stigma of facial scars and unintelligible speech are central to the person’s health-related quality of life, especially as adolescence approaches. Those born with orofacial clefts usually have normal mental intelligence and capacities that make the teasing and bullying they experience even more painful and distressing. In 1938, Herbert Cooper founded the first clinic in the United States for the sole purpose of treating CLP patients, whom he termed “facial cripples” to attract government and private funding. At this time, repair of bilateral clefts was commonly achieved by removal of the premaxilla, but this was found to have severe consequences in the later growth and development of the nasomaxillary complex and included loss of the incisors. With the team approach established in the 1940s, the integration of a coordinated treatment plan gave clinicians an organized timing and sequencing of interventions by the multiple specialists involved in the interdisciplinary treatment plan. By 1943, the American Cleft Palate Association (ACPA) was established to provide a national and an international forum for disseminating information to emerging teams and as an advocate for parents, caregivers, and patients. The Cleft Palate Journal , launched in January 1964, is the official publication of the ACPA and is currently published as the Cleft Palate-Craniofacial Journal .
The Northwestern University CLP Institute introduced the concept of coordinated and integrated treatment plans in a team approach around a conference table. At the 1953 meeting of the American Association of Orthodontists in Dallas, the theme of “an integrated service for unfortunate dentofacial cripples” focused on a team working together just 10 years after the accepted team concept was supported by the newly established ACPA in 1943. Although the concept of team management was a natural progression in the care of children with orofacial clefts, there was a proliferation of treatment modalities and a lack of reliable and valid outcome measures that resulted in acrimonious debates on which intervention was the most effective and efficient.
Surgeons were challenged by trying to bring the maxillary cleft segments into proximity so that palatal closure could be achieved by continuity of the soft tissues without fistulas. Uranoplasty compressed the cleft maxillary segments and collapsed them into contact for surgical closure. This was accepted treatment in Europe in the late 19th century. By the 1920s, Brophy’s “gradual compression by wiring” technique was abandoned in the United States. In 1914, Drachter, using caliper measurements of normal palatal and cleft palate widths, showed the “fallacy” of closing the cleft palate by forced compression of the maxillary segments. Dentists and orthodontists recognized that collapsing the arches caused “dental disasters,” and the Brophy technique and the “maxillary squeezers” used in forced contraction of the maxilla would be abandoned. Bone grafting into the cleft area to achieve bone continuity of the palate in the cleft site was being proposed, but it was not accepted as a standard of clinical practice until the availability of antibiotics; before this time, infection after surgery was difficult to control, with resulting morbidity and mortality. An early orthodontic contribution by Graber described the cleft palate deformity and provided insights into management and treatment.
Primary bone grafting to establish continuity in the cleft alveolus by the early 1950s was enthusiastically adopted in several centers. However, the results of this procedure were questioned in 1964, and Pruzansky called attention to the lack of a rationale to support the intervention. This resulted in most CLP centers discarding primary bone grafting techniques. Pruzansky noted that “the procedure apparently has not achieved the improved results anticipated and does not justify the hazard involved. Furthermore, it has been demonstrated that bone grafting in the primary stage of repair of cleft palate may actually be disadvantageous to the child’s maxillary growth pattern.” In 1972, a longitudinal study confirmed the effects of early bone grafting. Rosenstein and Rosenstein et al introduced a new concept in the early treatment of CLP and promoted primary bone grafting, although in reality few centers adopted the procedure. Most of these orthodontic controversies were published in the newly established Cleft Palate Journal starting in 1964, but summaries were reported in the American Journal of Orthodontics in the review sections.
Neonatal maxillary orthopedic procedures were used to realign the maxillary segments before surgery in patients with complete clefts of the lip and palate. There were some longitudinal studies indicating that presurgical segmental realignment before the age of 2.5 years remains relatively stable and that such treatment reduces the probability of a crossbite in the early mixed dentition. Further long-term studies of the effects of presurgical orthopedics were reported in the 1950s, and the approach of Burston and McNeil in Britain provided the beginning of a 60-year debate. This culminated in the nasoalveolar maxillary molding technique in the 21st century; although it is still controversial, it has advocates throughout the world.
In 1958, the American Journal of Orthodontics published an article entitled “Orthodontic treatment for the cleft palate patient” by Malcolm Johnston. Orthodontists were now serving on teams throughout the United States and becoming more involved in providing care for this special group of patients.
The next 50 years, 1965-2015
Technical advances and case presentations at professional meetings and published in peer-reviewed journals promoted the dissemination of new knowledge and techniques with lively discussions but little supporting evidence for the unsubstantiated claims of success. In 1973, the National Institute of Dental and Craniofacial Research reported a state-of-the-art assessment of treatment interventions and their outcomes that still resonates in 2015: (1) enthusiastic claims were made for a new type of therapy; (2) the procedure was widely adopted; (3) a flow of favorable clinical reports resulted; (4) little or no positive evidence developed to support the desirability of the procedure; and (5) there was a sharp drop in the number of clinical reports, again without evidence to support the change.
The conclusion from the National Institute of Dental Research report was that the best age at which to begin orthodontic treatment for children with CLP is still an open issue.
Textbooks covering the etiology and treatment of CLP were being written by Ross and Johnson in 1972 and reviewed by Saltzmann in the American Journal of Orthodontics . The textbook by Cooper et al (1979) was reviewed in the American Journal of Orthodontics in 1980, with the historical perspective of citing the first cleft palate clinic established in 1938 by Herbert Cooper.
The next 50 years, 1965-2015
Technical advances and case presentations at professional meetings and published in peer-reviewed journals promoted the dissemination of new knowledge and techniques with lively discussions but little supporting evidence for the unsubstantiated claims of success. In 1973, the National Institute of Dental and Craniofacial Research reported a state-of-the-art assessment of treatment interventions and their outcomes that still resonates in 2015: (1) enthusiastic claims were made for a new type of therapy; (2) the procedure was widely adopted; (3) a flow of favorable clinical reports resulted; (4) little or no positive evidence developed to support the desirability of the procedure; and (5) there was a sharp drop in the number of clinical reports, again without evidence to support the change.
The conclusion from the National Institute of Dental Research report was that the best age at which to begin orthodontic treatment for children with CLP is still an open issue.
Textbooks covering the etiology and treatment of CLP were being written by Ross and Johnson in 1972 and reviewed by Saltzmann in the American Journal of Orthodontics . The textbook by Cooper et al (1979) was reviewed in the American Journal of Orthodontics in 1980, with the historical perspective of citing the first cleft palate clinic established in 1938 by Herbert Cooper.
Contemporary role of the orthodontist in the management of orofacial clefts
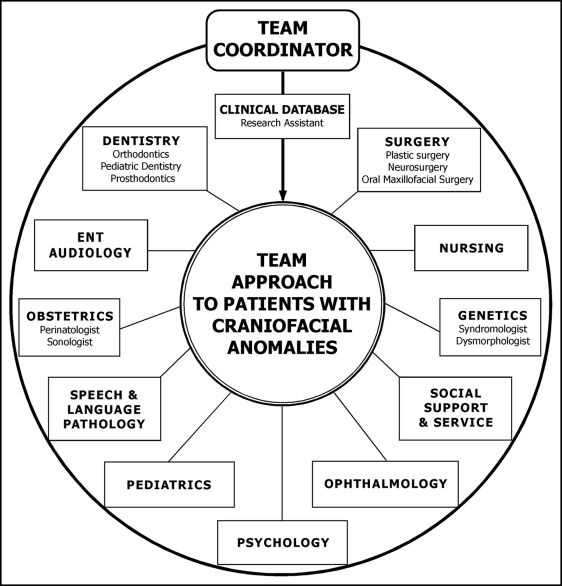
The original cleft palate teams in the 1950s represented 3 main disciplines: surgery, speech pathology, and orthodontics. By the 21st century, the team embraced multiple specialties as represented in Figure 1 , and most centers have adopted the principle of using defined times for treatment interventions in the context of a team approach. These conveniently fall into 4 stages with specific goals defined by periods of active orthodontic intervention followed by observation and rest periods. Numerous articles on CLP continue to be published in the AJO-DO , but they basically are defined by the time frame of growth and development. Whereas textbooks summarize the contemporary approach of the orthodontist in the management of CLP, the AJO-DO updates its readers on innovative developments in genetics and technical advances.
Prenatal period: importance of early diagnosis
Diagnosis of orofacial clefts with ultrasonography has become more common because technical refinements produce images by which congenital and developmental anomalies are more clearly detected. The ability to make the diagnosis in utero allows the parents to be prepared for the birth of their infant with a facial difference. Without prenatal diagnosis of a craniofacial anomaly, parents may experience an overwhelming sense of disappointment and guilt when the obstetrician informs them of their baby’s birth defect. Once a prenatal diagnosis of a craniofacial anomaly is made, counseling is provided to parents before delivery by the members of the cleft palate-craniofacial team. The team’s pediatric dentist or orthodontist may discuss with parents the dentoskeletal manifestations associated with clefts and offer an overview of the dental care required at the appropriate developmental stage. The plastic surgeon can discuss with the parents a customized plan for the management of the baby’s cleft based on the severity of the deformity.
Neonatal period: 2 weeks to 6 months
The goal of neonatal maxillary orthodontics was to eliminate the need for orthodontic treatment after the dentition erupted and did not include primary bone grafting. It was predicated on active and passive ideal alignment of the cleft segments in both unilateral and bilateral clefts of the lip and palate so that the teeth would erupt normally in their respective aligned segments. By treating at such an early age, the results would have to wait until the deciduous and permanent teeth erupted to convince the profession that early alignment of the segments with acrylic appliances did not eliminate orthodontic treatment. Modifications of appliances and primary bone grafting continued, but by the 1990s nasoalveolar molding (NAM) was gaining traction with the profession and was being reported in the Cleft Palate Journal . The intervention was typically performed by the orthodontist serving on the cleft palate and craniofacial team. With the use of an intraoral molding appliance and extraoral taping, the alveolar ridges are approximated within 1 to 2 mm of each other. The addition of nasal stents achieves lengthening of the columella in bilateral cleft patients. Ultimately, NAM prepares the infant for a 1-stage primary lip-nose repair between 3 and 5 months of age combined with gingivoperiosteoplasty to close the alveolar defect. The hard and soft tissue complications resulting from NAM are described by Levy-Bercowski et al, including recommendations on proper preventive and palliative measures. This technique is not without controversy, primarily in regard to the evidence supporting the benefits. In 2014, the AJO-DO captured this controversy in the Point/Counterpoint articles by Grayson and Garfinkle (Point) and Hathaway and Long (Counterpoint).
Deciduous dentition: 2 to 7 years
Although treatment in the deciduous dentition was popular in the 1930s and 1940s, most interventions were duplicated in the mixed dentition when the permanent teeth erupted. It therefore became prudent to delay most orthodontic interventions such as expansion and alignment of the incisors until the mixed dentition. With the development of the phonetic component of speech and language, articulation in the toddler is challenged by structural impairment. Lack of velopharyngeal competency and palatal mobility of the repaired cleft palate may result in adaptations by the child to reduce the hypernasality of speech and the development of glottal stops. To reduce the nasal air escape, a surgical pharyngeal flap may be suggested in which the soft palate is connected permanently to the superior anterior pharyngeal wall. Lip or nose revision surgeries are occasionally recommended for children before they start grade school.
Mixed dentition: 7 to 12 years
One major advantage for an orthodontist is having a successful alveolar bone graft in the cleft site into which the permanent canine erupts and brings additional alveolar bone. This requires close collaboration by the surgeon and orthodontist. Presurgical maxillary expansion is typically indicated; after the alveolar bone graft, the teeth adjacent to the cleft may be repositioned and moved into the sites without compromising their periodontal health. The controversies surrounding primary alveolar bone grafting resulted in some skepticism when secondary alveolar bone grafting was introduced in the oral surgery literature by Boyne and Sands and adopted by cleft palate teams. It took 15 years before a landmark publication from the team in Oslo, Norway, provided strong evidence for the benefits of autologous secondary bone grafting using cancellous bone from the iliac crest; this remains the gold standard in the 21st century. As the permanent teeth erupt, an association between cleft type and dental abnormalities of size, shape, and number becomes apparent, with the maxillary lateral incisor being the most vulnerable. The prevalence of “hypodontia” has been reported to increase with the severity of the cleft in both the deciduous and permanent dentitions. The circummaxillary sutures respond during the mixed dentition by modification and redirection of the nasomaxillary complex with protraction headgear. This became popular with orthodontists in the 1970s to correct the midface deficiency after its introduction by Delaire et al, who applied the protraction force to prevent relapse after surgical maxillary advancement. Children with unilateral CLP typically have a midface deficiency, and their response to the protraction facemask has been studied for skeletal and dental outcomes after treatment. More recently, the introduction of bone-borne anchorage with miniplates and miniscrews provides an orthopedic force that can be applied to the maxilla.
Permanent dentition: 12 years to adulthood
As growth stabilizes and the skeletal discrepancy is no longer a moving target, surgical corrections of the skeletal and nasolabial soft tissue revisions are planned. Adolescence is a difficult time for all young adults but especially if they have orofacial clefts. This special group of patients has already experienced multiple surgical procedures and nose and lip revisions. Speech may have deteriorated with velopharyngeal incompetency and the quality of life and social interactions impacted. Outcome measures of oral health–related quality of life of people with orofacial clefts have demonstrated significant psychological and social burdens. The adjustment of children to their facial deformity and scars is compounded by compromised speech and hearing disabilities. Functional and social-emotional well-being are reported to decrease their oral health–related quality of life, and the decrease is significantly greater in the 15- to 18-year-old subjects than in younger children with orofacial clefts. After definitive jaw surgeries and growth stabilizes, dental implants are an option for restoration of missing maxillary incisors at the cleft site with high success rates if sufficient bone is provided by autogenous grafts and with implant lengths of at least 13 mm in the grafted alveolar sites. More prospective clinical studies of dental implants in cleft sites are needed to improve the quality of evidence on their success rates. Mesializing the maxillary canine into the lateral incisor space (canine substitution) is a common alternative to implants, yielding similar esthetic results.
Technical advances in the 21st century
Cone-beam computed tomography
Cone-beam computed tomography (CBCT) technology is now available in orthodontic educational and private practice settings. Since 2005, the AJO-DO has published numerous articles on the applications of CBCT technology in orthodontic diagnosis and treatment planning. This 3-dimensional imaging of anatomic structures is especially valuable in evaluating cleft palate and other craniofacial skeletal anomalies. Hamada et al reported on the use of CBCT for the clinical assessment of alveolar bone grafting, demonstrating vertical and buccopalatal width measurements of the bone bridge. Wörtche et al used CBCT to evaluate axial and coronal sections through the cleft defect before alveolar bone grafting. Using volume-rendering software to analyze CBCT images, Oberoi et al objectively measured the amount of bone at the cleft site before and after alveolar bone grafting. The AJO-DO has since published several articles including applications of CBCT technology in the field of craniofacial orthodontics ( Table I ). As with any new technological advancement, the orthodontist is faced with the dilemma of the appropriateness of using CBCT in all patients or only in patients with clefts or craniofacial anomalies. In a special AJO-DO article by Abdelkarim, he advised that the prescription of radiographic imaging should be customized for each orthodontic patient, and thus not all patients (especially children) will require CBCT for diagnosis and treatment planning purposes. Specific to patients with clefts and craniofacial anomalies, Kuijpers-Jagtman et al overviewed the evidence for CBCT imaging in orthodontics and reported on 2 systematic reviews that support the use of CBCT in patients with orofacial clefts. There is a need to justify exposing all patients with orofacial clefts to CBCT, on any occasion, by performing a judicious clinical risk-benefit assessment.
| Authors, year | CBCT application |
|---|---|
| Pereira et al, 2011 | Diagnosis and localization of teeth in hyperdontia cases |
| Ohtani et al, 2012 | Evaluation of skeletal and soft tissue asymmetry in patients with hemifacial microsomia |
| Yoshihara et al, 2012 | Assessment of pharyngeal airway morphology and volumes in growing patients with clefts |
| Celikoglu et al, 2013 | Evaluation of mandibular asymmetry in patients with clefts |
| Shibazaki-Yorozuya et al, 2014 | Assessment of longitudinal craniofacial growth in patients with hemifacial microsomia |
| Celikoglu et al, 2014 | Evaluation of pharyngeal airway volumes in patients with unilateral clefts |
| Figueiredo et al, 2014 | Evaluation of maxillary dentoskeletal effects of expansion in patients with clefts |
| Celikoglu et al, 2014 | Measurement of facial soft-tissue thickness in patients with bilateral clefts |
| Yatabe et al, 2015 | Detection of bone dehiscences in maxillary canines moved into grafted alveolar clefts |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


