Introduction
The aim of this study was to use a microsensor to investigate the association among overjet reduction, treatment duration, and wear time of the van Beek activator.
Methods
The study sample comprised patients (n = 28) with a mean age of 11.60 (±1.25) years at start of treatment treated with the van Beek activator. The prescribed wear time was 12 hours per day. The evaluation period was limited to the first 3 appointments. The wear times during the 3 intervals were assessed. Treatment periods with good compliance were characterized by a wear time of 8 hours or more per day.
Results
The medians of overjet were 9.00 mm at the start of treatment and 5.75 mm at the third appointment. The mean total wear time throughout the evaluation period was 7.75 (±3.66) hours per day. Significant correlations were found at the 3 intervals. Patients with a mean wear time of 8 hours or more per day achieved significantly greater overjet reductions. Patients with good compliance of at least 5 months showed significantly greater overjet reductions.
Conclusions
Significant overjet reduction was achieved with a minimum daily wear time of 8 hours for at least 5 months. The level of compliance had a strong tendency to be maintained throughout the treatment period. No patient achieved the prescribed wear time of 12 hour per day.
Highlights
- •
We investigated the association between overjet reduction and wear time.
- •
Significant overjet reduction was achieved with a daily wear time of 8 hours.
- •
Significant overjet reduction was achieved in a treatment period of at least 5 months.
- •
A daily wear time of less than 8 hours showed no significant overjet reduction.
- •
No patient achieved the prescribed wear time of 12 hour per day.
Class II Division 1 malocclusions in children are commonly treated with various removable or fixed functional appliances. The general opinion about the treatment effect of these orthopedic appliances is that they produce a reduction of maxillary prognathism. These appliances also can enhance mandibular growth as well as retrude the maxillary incisors. An experiment on primates showed that the increase in mandibular growth by using activators occurred in the first 5 months of treatment. Other clinical studies on humans showed that the period of mandibular enhancement was comparatively short: 5 to 7 months.
The van Beek activator is a removable orthopedic functional appliance combined with high-pull headgear. This modified appliance is a monobloc activator with 2 external bows for occipital extraoral traction ( Fig 1 ). The monobloc has no contact with the lingual surface of the mandibular incisors, but it covers the labial surfaces and incisal edges. The upper part of the monobloc covers the palatal part of the occlusal side of the maxillary premolars, and the incisors are enclosed in the acrylic up to the cervical margin. The total treatment period with a van Beek activator consists of active and retention phases. A normal overjet without forward force bite should be achieved in the active treatment phase and stabilized in the retention phase. Previous studies with van Beek activators have shown decreases in overjet and overbite, improvements of the jaw base and molar relationship, restraint of maxillary forward growth, limited retrusion of the maxillary incisors, distal displacement of the maxillary molars, and some proclination of the mandibular incisors. Despite the skeletal effects, overjet reduction during van Beek activator treatment is mainly due to dentoalveolar changes.

The cooperation of children and adolescents plays a major role in achieving the desired results with removable activators. In previous studies, it has been shown that the average wear times for removable orthodontic appliances were 7 up to 9 hours per day. Nevertheless, opinions differ on how many hours per day the van Beek activator and other activators should be worn to reach an effective overjet reduction.
In many studies, methods for assessing patient compliance have been suggested. For instance, compliance can be assessed by measuring the amount of orthodontic tooth movement, by asking patients and parents direct and detailed questions about appliance wear times, and by using electronic timing devices.
Electronic microsensors, such as the TheraMon sensor (Handelsagentur Gschladt, Hargelsberg, Austria), are useful to measure the wearing times. The TheraMon sensor is easy to use and has proved to be reliable and accurate in assessing the wear time of removable orthodontic appliances. Moreover, microelectronic measuring and documentation of wear times and wear behaviors offer the possibility to make more efficient treatment planning decisions with removable appliances.
Our aim in this study was to use the TheraMon sensor to investigate the association between objective wear times, overjet changes, and duration of treatment with van Beek activators.
Material and methods
The study sample was drawn from 38 adolescent Class II Division 1 patients seeking orthodontic treatment at the orthodontic clinic of the Academic Centre of Dentistry of Amsterdam in The Netherlands ( Fig 2 ). The treatment period was between June 2011 and October 2014. Inclusion criteria were healthy patients without syndromes, clefts, systemic diseases, or previous orthodontic treatment; with a Class II Division 1 malocclusion; and with an overjet of at least 6 mm. The sample in this study consisted of 28 patients (20 boys, 8 girls) treated with a van Beek activator by residents of the Department of Orthodontics. These activators had TheraMon sensors to record the wear time during the evaluation period ( Fig 1 ). Patients and parents were informed about the microsensor in the activator, and there were no objections to participating in the study. At the beginning of treatment (T0), the mean age was 11.60 years (SD, 1.25), and the median was 11.66 years. This research project was approved by the Medical Ethical Committee of the Vr ije Universiteit University Medical Centre (FWA00017598).

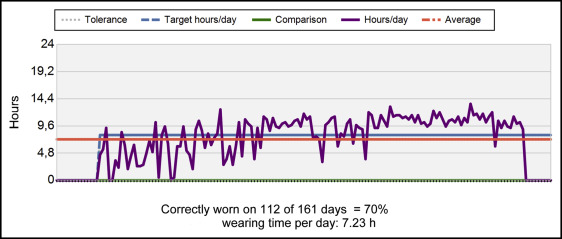
TheraMon sensors were fitted into each appliance by the technician and activated according to the manufacturer’s instructions. The TheraMon sensor used is a relatively small (12.83 × 8.73 × 4.2 mm) device covered by polyurethane. It uses an application-specific integrated circuit with a 16-kilobyte internal electronically erasable programmable read-only memory. The sensor registers temperatures every 15 minutes for up to 18 months. The recorded time that the temperature was more than 35°C corresponds to the time that the activator was worn. The TheraMon readout station reads the data. A diagram with the relevant information is generated ( Fig 3 ).
After the activators were fitted with 2 external bows for occipital extraoral traction and the headgear cap, patients were instructed to insert the appliance first in the mandibular arch and then to bite forward into the appliance. They were taught to close the lips firmly when swallowing, suck on the appliance, and clench the teeth on the appliance during swallowing. They were instructed to wear the activator with the high-pull headgear for at least 12 hours per day. The force exerted by the high-pull headgear was between 230 and 260 g.
The patients were told that some discomfort and minor mobility of teeth might be experienced. They were instructed on how to clean the appliance with a toothbrush and cold water.
Overjet was assessed between the maxillary and mandibular right central incisors by using an orthodontic ruler. The reliability and validity of the overjet measurements were investigated in an untreated control group (n = 16). Two independent and blinded observers (A.S.A.K., R.B.K.) measured the overjets in the control group at 2 time points with intervals of 1 week. The overjet of every subject in the test sample was measured at each visit by the same residents and noted in the patient’s sheet. Wear time between 2 intervals was quantified by using the TheraMon software, as shown in Figure 3 . The wear time in the memory of the chip before the start of the treatment was 0 hours per day. The wear time measurements of the first 3 intervals were used for the statistical analysis.
The total evaluation period encompassed only the first 3 appointments of the active treatment phase and covered a period between 3.6 months (108 days) and 9.3 months with 3 successive wear-time records and overjet measurements. In all patients, the treatment continued after the third appointment. The threshold of good compliance in the software program of the TheraMon sensor was 8 hours per day. Treatment periods with a daily wear time of 8 hours or more throughout the evaluation period (good compliance) were recorded. These days were calculated by using the software of TheraMon sensor ( Fig 3 ). Previous clinical studies showed that with orthopedic activators a normal overjet could be achieved in 5 to 7 months. Consequently in this study, a cutoff point of 5 months was chosen to investigate the effect of the duration of good compliance on the overjet changes.
Statistical analysis
Statistical analysis of the collected data was performed using SPSS for Windows software (version 21; IBM, Armonk, NY). The amount of overjet reduction between the intervals was expressed as a percentage of the previous overjet. Overjet reduction percentages between the intervals and overall were calculated by using the following formula
Percentage overjet reduction = overjet reduction in mm at T 1 , 2 , and 3 overjet in mm at T0, 1 , and 2 × 100
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


