Subapical mandibular surgeries have been used to correct vertical malocclusion and interdental problems associated with mandibular deformity. Subapical surgery to the anterior part of the mandible is applicable in many patients with anterior open bite and deepbite. Surgery of the posterior part of the mandible is needed less frequently than surgery of the anterior part. This case report describes the surgical-orthodontic treatment of a 21-year-old woman who underwent posterior subapical mandibular surgery. Her chief complaint was facial asymmetry, and she had a collapsed mandibular arch with a scissors-bite of the right premolars and molars. After subapical osteotomy, surgically assisted correction of the collapsed right mandibular arch was performed with a lingual arch appliance. Comprehensive orthodontic treatment was initiated in both arches after this correction. Le Fort I osteotomy and sagittal split ramus osteotomy were used to correct the facial asymmetry. Her facial appearance and temporomandibular problems were markedly improved, and she achieved a functional and stable occlusion after these treatments. This case report demonstrates the efficiency of posterior subapical mandibular surgery for a patient with a collapsed mandibular arch and a scissors-bite.
Anterior subapical mandibular surgery was first described by Köle and was mainly applied to patients with anterior open bite and deepbite. This surgery is frequently used to correct vertical problems, but it can also advance or retrude a dentoalveolar segment. Total subapical mandibular surgery was first described by MacIntosh. This involves moving the total mandibular dentoalveolus in an anterior, posterior, or superior direction. Compared with these 2 subapical surgeries, posterior subapical mandibular surgery has been less frequently used. This is mainly due to the risk of injuring the inferior alveolar neurovascular bundles.
This case report describes the surgical-orthodontic treatment of a 21-year-old woman with a unilateral collapsed mandibular arch and a scissors-bite. Posterior subapical mandibular surgery was applied, and surgically assisted correction of the mandibular arch was performed. This report demonstrates the efficiency of posterior subapical mandibular surgery to treat a severely collapsed or narrowed arch.
Diagnosis and etiology
A Japanese girl was born to healthy parents without a facial deformity. She had been having difficulty with occlusion from her youth but did not seek treatment. She visited our dental hospital at 21 years 0 months of age with a chief complaint of facial asymmetry ( Figs 1-3 ).

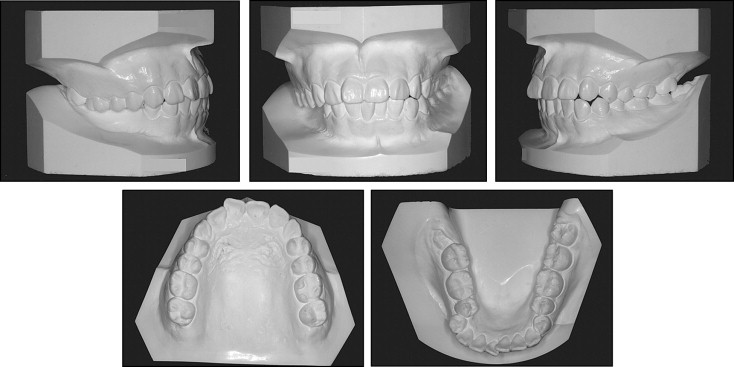
Her facial photographs showed an asymmetric mandible and chin. Her philtrum and lip were inclined in the frontal facial view. The mandibular right second premolar and 3 molars had collapsed lingually, and a scissors-bite was noted. There was premature contact because of this collapsed mandibular arch, and a functional shift was noted toward the left. She occasionally had pain in both temporomandibular joints and frequently had clicking sounds on the right side. Her overbite and overjet were both 2 mm, and the midline of the mandibular central incisors was 4 mm to the left.
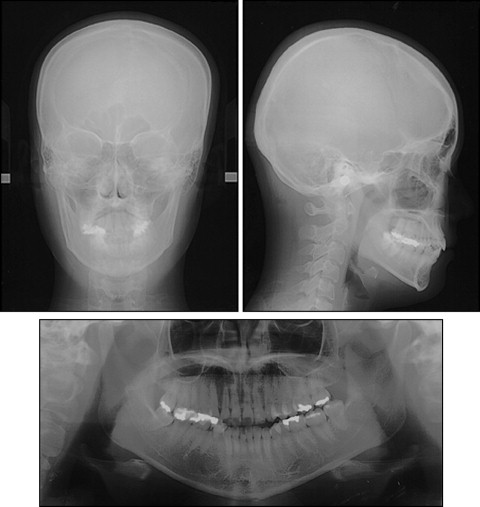
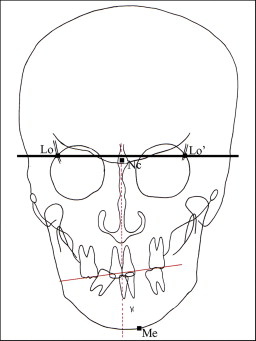
A panoramic radiograph showed that the mandibular third molars were present on both sides. A posteroanterior cephalogram showed an inclined maxilla and mandible in the frontal dimension ( Fig 3 ). The cephalometric tracing showed that the maxillary occlusal plane inclined by 7.5°, and menton was located 11.0 mm to the left ( Fig 4 ; Table I ). The SNA, SNB, and mandibular plane angles were comparable with Japanese norms ( Table II ), and the skeletal disharmony was not apparent in the sagittal or vertical dimension.
| Pretreatment (21 y 0 mo) | Immediately before Le Fort I osteotomy and SSRO (23 y 6 mo) | Immediately after active orthodontic treatment (24 y 8 mo) | One year after active orthodontic treatment (25 y 8 mo) | |
|---|---|---|---|---|
| Inclination of maxillary occlusal plane (°) | 7.5 | 7.5 | 1.0 | 1.0 |
| Deviation of menton (mm) | 11.0 | 8.0 | 2.5 | 2.5 |
| Angle (°) | Japanese norm ± SD | Pretreatment (21 y 0 mo) | Immediately before Le Fort I osteotomy and SSRO (23 y 6 mo) | Immediately after active orthodontic treatment (24 y 8mo) | One year after active orthodontic treatment (25 y 8 mo) |
|---|---|---|---|---|---|
| SNA | 82.3 ± 3.5 | 79.4 | 79.4 | 80.0 | 79.6 |
| SNB | 78.9 ± 3.5 | 78.3 | 77.0 | 77.7 | 77.2 |
| ANB | 3.4 ± 1.8 | 1.1 | 2.4 | 2.3 | 2.2 |
| U-1 to FH plane | 111.1 ± 5.5 | 114.5 | 116.2 | 116.8 | 117.0 |
| L-1 to mandibular plane | 96.3 ± 5.8 | 97.5 | 101.7 | 97.5 | 97.2 |
| Mandibular plane | 28.8 ± 5.2 | 27.4 | 29.2 | 30.0 | 30.2 |
| Gonial | 122.2 ± 4.4 | 126.4 | 126.4 | 126.5 | 125.2 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


