The prevalence of impacted second molars is low, varying from 0% to 2.3%. The etiology of an impaction can involve systemic, local, and periodontal factors, as well as a developmental disruption of the tooth germ. A number of surgical and orthodontic treatment options have been suggested in the literature, including leaving the tooth in situ, removing the impacted second molar, orthodontic uprighting, and autotransplantation. Removal of third molars has been suggested as an adjunct for space creation. This article presents the treatment of a girl with bilateral severely impacted mandibular second molars as well as an ectopic maxillary left canine and severe crowding affecting both the maxillary and mandibular arches. Her treatment was successfully completed with fixed preadjusted edgewise appliances (0.022 × 0.028-in slot size) and MBT prescription (APC precoated Gemini Brackets; 3M Unitek, St. Paul, Minn), along with the removal of 4 first premolars. The maxillary left canine and the mandibular second molars were surgically exposed. The treatment mechanics show that even severely impacted second molars can be uprighted by routine straight-wire techniques, which are easy to apply. The center of rotation of the second molar lies in the bifurcation of the roots of this tooth, and this biomechanical property was used to its full advantage. The techniques applied comprised bracket repositioning, bypass of brackets, conversion of molar tubes to brackets, thermoelastic copper-nickel-titanium archwires, and a push-coil spring. Other orthodontic treatment mechanics, which require complex sectional or segmental techniques, auxiliaries, or artistic wire bending, that have been suggested in the literature were not used here. The third molars were not removed.
Impaction of permanent teeth is a relatively common occurrence that can involve any tooth in the dental arch. The frequency of impaction is highest for mandibular and maxillary third molars, followed by maxillary canines and mandibular second molars. The eruption of the permanent molars differs from that of other permanent teeth, since there are no preceding deciduous teeth. For permanent molars, the tooth germ develops from the backward extension of the dental lamina. Unilateral impaction of the mandibular second molar is more common than bilateral impaction. It occurs more frequently in the mandible, among male patients, and on the right side of the jaw. Impacted second molars are most often mesially inclined. The 3 main causes of second molar disturbances are an ectopic position of the follicle, obstacles in the path of eruption, and failure of the eruption mechanism. It is important to diagnose this condition early so that treatment can begin at the optimal time. It is thought to be ideal to treat this condition during early adolescence, when second molar root formation is still incomplete and before complete development of the mandibular third molars. Treatment at this time has been found to improve the outcome.
The indications for treatment of impacted second molars include prevention of pericoronitis, increased risk of caries and periodontal disease, risk of resorption of adjacent teeth by the follicle, and cystic development of the follicle. Treatment modalities for impacted mandibular second permanent molars include orthodontic (with or without removal of third molars) and surgical repositioning (autotransplantation). Removal of the second molars to allow eruption of the third molars and autotransplantation of the third molars after extraction of the second molars have also been described in the literature.
Surgical repositioning of mesially impacted teeth, however, can be associated with unwanted side effects, such as ankylosis, replacement resorption, and loss of tooth vitality. In a recent study, autotransplantation of third molars was successful in 11% of the patients. Orthodontically assisted guided eruption is thought to be the treatment of choice for impacted second molars, with a success rate of 70%. This procedure might be difficult if the tooth is caudal to the occlusion or horizontally positioned.
Several orthodontic treatment modalities have been suggested to guide the eruption of impacted second molars, including diverse spring designs often encompassing sectional or segmental mechanics. Other treatment mechanics such as the use of temporary cortical anchorage devices (mini-implants) in the retromolar region have also been suggested. Surgical treatment is often required as an adjunct; this can involve exposure of the second molars or removal of the third molars. Alignment of the impacted molar can sometimes be obtained without surgical assistance because the orthodontic uprighting involves a distal tipping movement, which creates space for the impacted molar. However, interference with the third molar cannot be excluded.
Diagnosis and etiology
A 9-year-old female patient was referred to the orthodontic department of Guy’s and St Thomas’ NHS Dental Hospital Trust, London, United Kingdom, because of delayed eruption of the maxillary left central incisor. She was diagnosed with a Class I incisor relationship in the early mixed dentition with crowding affecting both the maxillary and the mandibular arches. Both maxillary deciduous canines were removed to relieve the crowding in the labial segment ( Fig 1 ). On review 6 months later, the maxillary left central incisor had erupted, and both maxillary permanent canines were palpable high in the buccal vestibule. The crowding in both arches was confirmed, but orthodontic intervention was thought unnecessary at this stage.

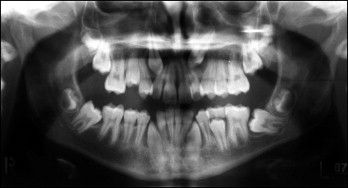
Further review appointments confirmed the above diagnosis and did not lead to further intervention. Reevaluation at age 11 confirmed severe crowding in both arches, and a radiograph showed the ectopic position of the maxillary left canine and the mesial impaction of both mandibular second molars, with the left one horizontally impacted ( Fig 2 ). All 4 first premolars were subsequently extracted to create space to allow for spontaneous alignment of the anterior teeth and improvement of the eruption path of the impacted maxillary left canine.
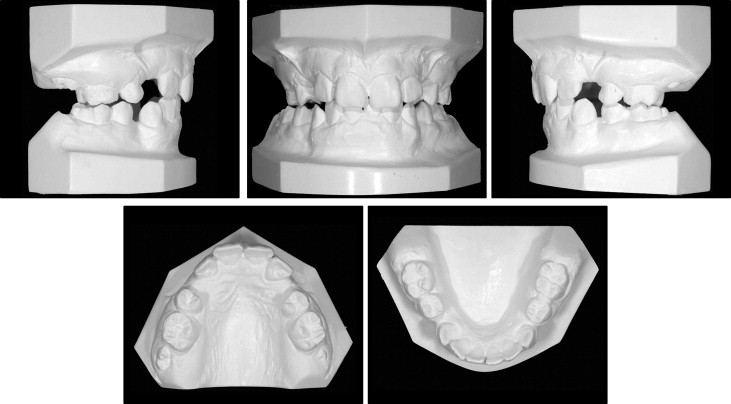
Six months later, the patient complained of “gaps in the front” of her teeth ( Figs 3 and 4 ). A detailed clinical examination confirmed a Class I incisor relationship (British Standards Institute classification) on a mild Class II skeletal base with average vertical facial proportions. The position of the ectopic maxillary left canine had not improved, and the position of both mandibular second molars was also unchanged. There was spacing in the maxillary and mandibular arches with potential crowding in the maxillary arch; the maxillary right canine was short of space but in a favorable position for spontaneous eruption. The left canine was still ectopic. Overbite was increased, and the mandibular centerline was deviated to the left by 1 mm. The incisors appeared slightly retroclined on clinical examination. There was a buccal crossbite of the maxillary right first molar, and the first molar relationship was nearly Class II on the left and complete Class II on the right. The maxillary left canine was subsequently surgically exposed, and a gold chain was attached. The canine was buccal, and a surgically repositioned flap design was chosen for the best possible outcome of the gingival margin.

The cephalometric analysis ( Table ) confirmed the clinical findings of a mild Class II skeletal base relationship with an increased ANB angle (5°). The Wits appraisal, however, suggested a moderate Class II skeletal pattern (+3.5 mm). The maxillary-mandibular plane angle of 27° and the lower facial height proportions (55%) were within normal limits; this confirmed the clinical findings. The maxillary incisors were retroclined (100°). The mandibular incisor inclination (87°) was at the lower limit of the normal range. Although the incisors were technically Class I according to the British Standard Institute’s classification, they showed some features of a Class II Division 2 incisor relationship. The panoramic radiograph ( Fig 5 ) showed a complete permanent dentition, except for the 4 previously extracted first premolars.
| Variable | Pretreatment | Normal | Posttreatment | Change |
|---|---|---|---|---|
| SNA | 85° | 82° ± 3° | 84° | +1° |
| SNB | 80° | 79° ± 3° | 80° | 0° |
| ANB | 5° | 3° ± 1° | 4° | +1° |
| SN to maxillary plane | 7° | 8° ± 3° | 7° | 0° |
| Wits appraisal | 3.5 mm | 0 mm | 5 mm | +1.5 mm |
| Maxillary incisor to maxillary plane angle | 100° | 108° ± 5° | 112° | +12° |
| Mandibular incisor to mandibular plane angle | 87° | 92° ± 5° | 90° | +3° |
| Interincisal angle | 148° | 133° ± 10° | 134.5° | −13.5° |
| Maxillary-mandibular angle | 27° | 27° ± 5° | 27° | 0° |
| Upper anterior face height | 55 mm | 56 mm | +1 mm | |
| Lower anterior face height | 66 mm | 70 mm | +4 mm | |
| Face height ratio | 55% | 55% | 56% | +1% |
| Mandibular incisor to APo line | −1 mm | 0-2 mm | 1 mm | +2 mm |
| Lower lip to Ricketts’ E-plane | 0 mm | −2 mm | −2 mm | −2 mm |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


