Diagnosis and etiology
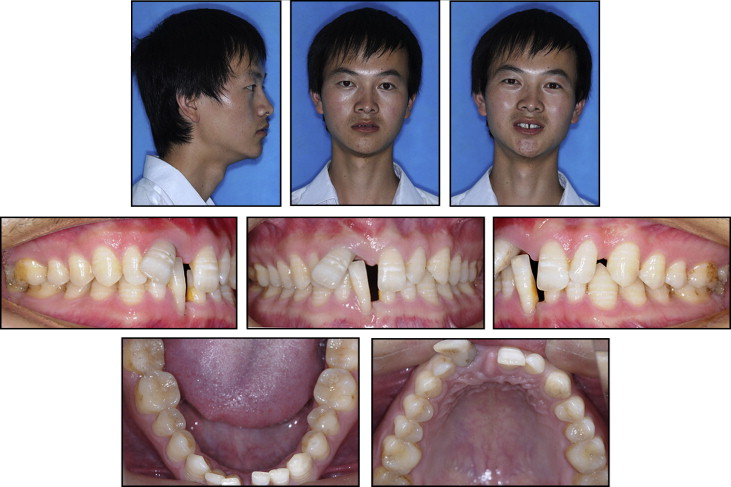
A man (age, 22 years 6 months) came to the orthodontic office of our hospital in Chendu, China. His chief complaints were displaced maxillary and mandibular anterior teeth and large gaps between the incisors. He was eager to improve both his appearance and self-confidence by orthodontic treatment. He was self-conscious about the appearance of his teeth. He had no history of smoking. He had a symmetrical face with a straight profile. Angle Class I canine and molar relationships on both sides were observed, with an acceptable occlusion in the posterior segment. The main problem was in the anterior region. He had a severe deep overbite, and a deep gap was visible when he smiled. His mandibular right central incisor just impinged on the mesial cervix of the maxillary right central incisor, with rotation of the maxillary right central incisor and extrusion of both maxillary and mandibular right central incisors. Severe gingival recession was observed in the incisors. A 3-mm-deep periodontal pocket could be explored in the mesial aspect of the maxillary right central incisor, with a 4-mm-deep pocket in the mesial aspect of the mandibular right central incisor. Penpyema (pyorrhea of periodontium observable on periodontal probing) could be seen in the pocket of the maxillary central incisor. Both the maxillary and mandibular right incisors were extruded. The exposed root length of the mandibular right incisor was almost half of the whole. There were mild arch-length discrepancies in both arches: the maxillary available space was 6.0 mm, and the mandibular space was 2.0 mm. The anterior Bolton index was 74.39%, and the overall Bolton index was 88.6%. The curve of Spee was about 3.5 mm ( Figs 1-4 ).
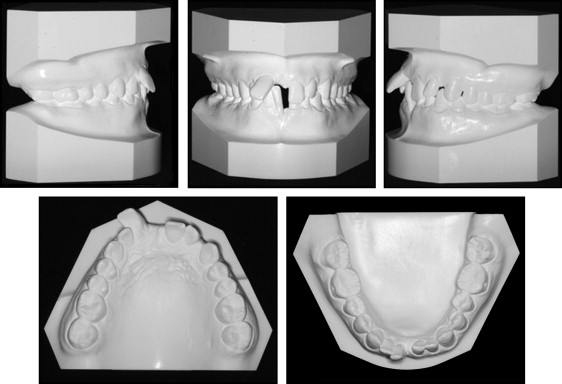

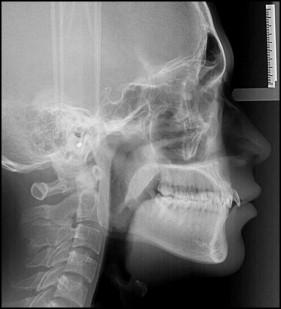
The panoramic radiograph showed that all teeth were present except the 4 third molars. Pathologic migration of the maxillary and mandibular right central incisors was also observed on the panoramic radiograph ( Fig 3 ). Extensive resorption of alveolar bone could be seen on the film, mainly in the premolar and anterior regions. In some sites of the anterior teeth, the resorption area was as large as half to two thirds of the root surface; eg, the maxillary and mandibular right central incisors. An infracrestal pocket was faintly visible in the mesial aspect of the maxillary right central incisor (subsequent follow-up periapical films during treatment also confirmed this). Cephalometric analysis showed a Class I skeletal pattern (with a slight Class III tendency) with the pathologically displaced maxillary right central incisor protruded ( Fig 4 , Table I ) and the mandibular plane angle within the normal range (28.7° ± 5.3°). Based on these findings, the patient was diagnosed with a skeletal Class I malocclusion with severe periodontitis and pathologic tooth migration.
| Measurements | Mean | Pretreatment | Posttreatment |
|---|---|---|---|
| SNA (°) | 81.69 ± 2.54 | 82.07 | 81.60 |
| SNB (°) | 78.94 ± 2.19 | 80.62 | 80.09 |
| ANB (°) | 2.75 ± 1.16 | 1.45 | 1.51 |
| MP-SN (°) | 32.85 ± 4.21 | 28.43 | 28.14 |
| Y-axis (°) | 63.54 ± 3.23 | 60.85 | 60.96 |
| S-Go/N-Me (mm) | 65.85 ± 3.83 | 69.64 | 71.46 |
| U1-SN (°) | 74.94 ± 6.22 | 63.79 | 75.01 |
| FMIA (°) | 57.0 ± 6.79 | 67.77 | 71.86 |
Treatment objectives
The orthodontic treatment objectives for this patient were to achieve a stable occlusion; restore esthetics, function, and periodontal health in the anterior region; and maintain the existing occlusion in the posterior region. These objectives were aimed at preventing mutual aggravation of occlusal trauma and periodontitis, leading to better facial esthetics and enhancing self-confidence. The orthodontic treatment objectives were built on a complete treatment plan for this periodontal patient.
The complete treatment plan for this patient consisted of 4 main phases: systemic, hygienic, corrective, and maintenance (supportive periodontal therapy). In the hygienic phase, the periodontists gave the patient oral hygiene instructions and motivated him to maintain his oral hygiene. Scaling and root planing of all teeth were carried out at the same time. Before the corrective phase, the following criteria had to be satisfied: proper infection control, full-mouth plaque index within 25%, the full-mouth percentage of positive bleeding on probing sites less than 30%, and no residual pockets deeper than 5 mm. Once orthodontic treatment was finished, the maintenance phase began. The patient was required to be reviewed every 3 to 6 months to prevent reinfection and recurrence.
A multidisciplinary approach was chosen for this patient because the final result must be guaranteed by a qualified dental team: orthodontists, periodontists, and prosthodontists. It was necessary for the orthodontists to cooperate with the periodontists throughout the treatment and also cooperate with the prosthodontists when the orthodontic treatment was finished. Appropriate intrusion and uprighting of anterior teeth were involved in the progress of the treatment; these were combined with thorough scaling and planing of the root surfaces of particular anterior teeth. For the poor periodontal status, light forces to move teeth and minimize occlusal trauma were used. At the beginning of the alignment, Australian archwires shaped to the original alignment of the dentition were chosen to extenuate the aligning force exerted on each tooth. An occlusal splint was used to prevent occlusal trauma to the anterior teeth during the early stage of alignment. Slightly grinding the crown of the extruded mandibular right central incisor to reduce the ratio of crown to root length could also contribute to reducing the occlusal trauma. According to our model analysis, the Bolton index was slightly deviated from normal, so restorative treatment might be required for the maxillary lateral incisors after orthodontic treatment. Since there was discoloration of the maxillary right central incisor, necrosis of the pulp was suspected. We requested an endodontic consultation for this tooth, and restorative treatment might be necessary after orthodontic treatment.
Treatment objectives
The orthodontic treatment objectives for this patient were to achieve a stable occlusion; restore esthetics, function, and periodontal health in the anterior region; and maintain the existing occlusion in the posterior region. These objectives were aimed at preventing mutual aggravation of occlusal trauma and periodontitis, leading to better facial esthetics and enhancing self-confidence. The orthodontic treatment objectives were built on a complete treatment plan for this periodontal patient.
The complete treatment plan for this patient consisted of 4 main phases: systemic, hygienic, corrective, and maintenance (supportive periodontal therapy). In the hygienic phase, the periodontists gave the patient oral hygiene instructions and motivated him to maintain his oral hygiene. Scaling and root planing of all teeth were carried out at the same time. Before the corrective phase, the following criteria had to be satisfied: proper infection control, full-mouth plaque index within 25%, the full-mouth percentage of positive bleeding on probing sites less than 30%, and no residual pockets deeper than 5 mm. Once orthodontic treatment was finished, the maintenance phase began. The patient was required to be reviewed every 3 to 6 months to prevent reinfection and recurrence.
A multidisciplinary approach was chosen for this patient because the final result must be guaranteed by a qualified dental team: orthodontists, periodontists, and prosthodontists. It was necessary for the orthodontists to cooperate with the periodontists throughout the treatment and also cooperate with the prosthodontists when the orthodontic treatment was finished. Appropriate intrusion and uprighting of anterior teeth were involved in the progress of the treatment; these were combined with thorough scaling and planing of the root surfaces of particular anterior teeth. For the poor periodontal status, light forces to move teeth and minimize occlusal trauma were used. At the beginning of the alignment, Australian archwires shaped to the original alignment of the dentition were chosen to extenuate the aligning force exerted on each tooth. An occlusal splint was used to prevent occlusal trauma to the anterior teeth during the early stage of alignment. Slightly grinding the crown of the extruded mandibular right central incisor to reduce the ratio of crown to root length could also contribute to reducing the occlusal trauma. According to our model analysis, the Bolton index was slightly deviated from normal, so restorative treatment might be required for the maxillary lateral incisors after orthodontic treatment. Since there was discoloration of the maxillary right central incisor, necrosis of the pulp was suspected. We requested an endodontic consultation for this tooth, and restorative treatment might be necessary after orthodontic treatment.
Treatment alternatives
Treatment modalities for such a patient include orthodontic treatment and after extraction of severely displaced teeth. In view of the patient’s age and because the occlusal trauma and periodontitis aggravated each other, prosthodontic treatment was not thought to be a good alternative. Prosthodontic treatment cannot resolve a deep overbite, an esthetic problem of the anterior region caused by a periodontal defect. Also, prosthodontic treatment might result in health hazards of other teeth. With orthodontic treatment, we could reestablish a stable occlusion, restore esthetics and function, and prevent mutual aggravation of occlusal trauma and periodontitis. Orthodontic treatment assisted by regular periodontal treatment was considered the best choice for this young patient. The decision was made to use relatively simple orthodontic treatment mechanics: the direction and strength of the orthodontic forces were well controlled step by step, with whole monitoring of the periodontal status.
Treatment progress
First, we consulted with physicians, determining whether further examination was required to exclude other systemic diseases. Second, the patient was required to see a periodontist periodically. The periodontist gave him oral hygiene instructions and motivated him to maintain oral hygiene, and scaling and root planing of all teeth were carried out at the same time. Three months later, the orthodontists and periodontists held a consultation. We made sure that the periodontal status satisfied the criteria: proper infection control, full-mouth plaque index within 25%, the full-mouth percentage of positive bleeding on probing sites less than 30%, and no residual pockets deeper than 5 mm; this meant that the periodontitis had moved to a chronic phase.
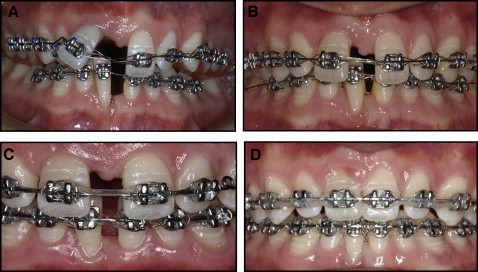
Then the patient was referred to our orthodontic office again. Before the appliance was bonded, the extruded mandibular right central incisor was ground to reduce the ratio of crown to root length. A 0.022-in preadjusted edgewise appliance was placed in the mandibular arch (from first premolar to first premolar), and a prepared occlusal splint was placed on the maxilla to relieve the occlusal interference and trauma between the maxillary and mandibular incisors ( Fig 5 , A ). A 0.014-in Australian archwire with a step between the 2 mandibular central incisors (shaped to the original step between the teeth) was used to align the mandibular arch segmentally and gradually. Four months later, the extruded and rotated mandibular right central incisor had been corrected slightly, and a 0.022-in preadjusted edgewise appliance was placed in the maxillary arch (from second premolar to second premolar). A 0.014-in Australian archwire shaped to the original alignment of the maxillary arch was installed ( Fig 5 , A ).