Introduction
This report describes the clinical orthodontic management of a patient with spastic quadriplegia and cerebral palsy. Guidelines to overcome difficulties encountered during the treatment period are suggested.
Methods
A 13-year-old boy with cerebral palsy and spastic quadriplegia complained of an undesirable oral appearance because of his malocclusion. He had a Class II molar relationship, with severe maxillary and moderate mandibular anterior crowding. Enamel hypoplasia was apparent on all teeth. He had losses of body function and upper extremity function of 70% and 39%, respectively. His physical limitations necessitated a treatment approach that did not rely on patient-dependent appliances. The treatment plan called for maxillary first premolar extractions, mandibular incisor protrusion, and air rotor stripping.
Results
The patient’s oral function and esthetic appearance were significantly improved. Aligned dental arches with good occlusion were obtained. The patient’s self-confidence improved during the treatment period.
Conclusions
Physical appearance can influence personality and social acceptability. Corrective orthodontic treatment for patients with physical handicaps can improve not only oral function, but also self-confidence and self-esteem.
Highlights
- •
Orthodontic treatment for a boy with quadriplegia and cerebral palsy is reported.
- •
Oral function and esthetic appearance were significantly improved.
- •
Treatment emphasized appliances that minimize reliance on patient compliance.
Cerebral palsy (CP) is a general term for a group of developmental disorders affecting movement and posture. CP is frequently accompanied by mental retardation and altered sensation, perception, and communication abilities. The exact prevalence of CP is unknown; however, the reported rate is 2 to 3 per 1000 live births; this increases to 40 to 100 per 1000 births among preterm or low-birth-weight children. CP can be attributed to nonprogressive neurologic disturbances that affect the fetal or infant brain and result in varying disabilities.
Movement impairments in people with CP can be classified as spastic, ataxic, athetoid, or mixed. The most common form is spastic CP, which is predominantly characterized by elevated muscular tonus resulting from deficits in the motor cortex or corticospinal tract. In ataxic CP, the cerebellum is affected, resulting in losses of coordination and balance. Patients with athetoid CP exhibit mixed muscle tone and involuntary movements caused by basal ganglia dysfunction. Mixed CP involves more than one form of CP.
In CP, motor dysfunction and alterations in muscle tone and function frequently lead to deviations in facial growth and dental occlusal development. Patients with CP with spastic quadriplegia mostly have a Class II growth pattern with malocclusion. The most common orofacial abnormalities associated with CP are increased overjet, lip incompetence (often accompanied by drooling), missing teeth, greater prevalence of periodontal disease, and enamel defects. In terms of overbite relationship, conflicting studies show both increases and decreases in overbite. Most orofacial abnormalities are more prevalent in persons with CP who also have severe mental retardation. Although the orthodontic literature contains some articles regarding the clinical management of children with handicaps, reports specific to children with CP are few. We describe the orthodontic treatment of a CP patient with spastic quadriplegia, emphasizing the guidelines to overcome difficulties encountered during the treatment period.
Etiology and diagnosis
A 13-year-old boy with CP and spastic quadriplegia was referred to our clinic because of his undesirable oral appearance caused by malocclusion ( Fig 1 ). The cause of CP was diagnosed as a maternal urinary tract infection. His loss of total body function was 70%, and his loss of upper extremity function was 39%. He needed assistance to walk and eat. In addition to motor dysfunctions, mild mental retardation was also present (IQ, 56). Prominent neck flexion was apparent due to increased muscular tonus. Enamel hypoplasia affected all teeth, a common finding in patients with CP.
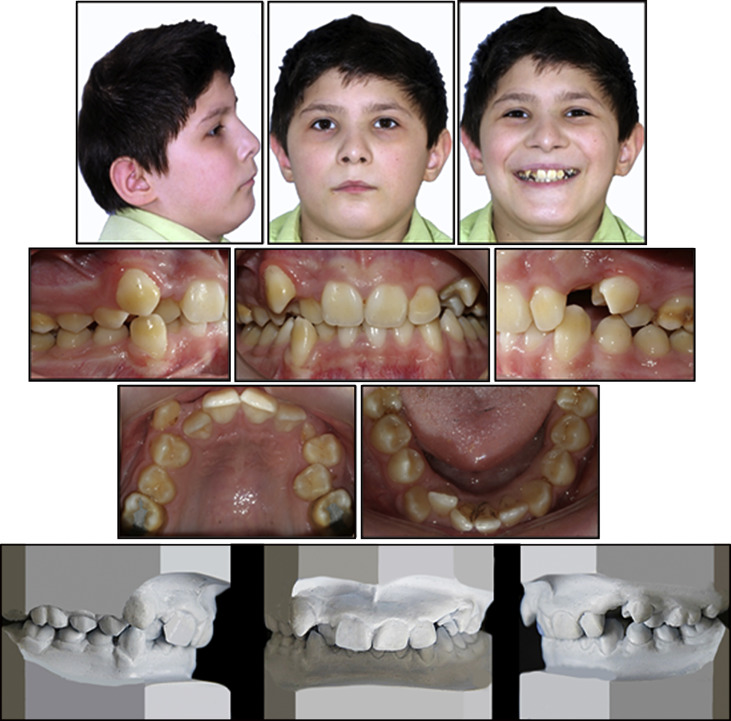
The cephalometric evaluation showed a convex profile, a protrusive maxilla, and a relatively normal mandible with a high-angle growth pattern ( Table ). In terms of vertical growth, his articular, gonial, and mandibular plane angles were all increased. In the transversal direction, no crossbites were observed. He was skeletally Class I with an ANB angle of 4°, a Class II dental relationship with severe maxillary (11 mm) and moderate mandibular (4 mm) crowding. Because of a severe lack of maxillary space, his maxillary left canine was unerupted, and the right canine was infrapositioned in the vestibule. Despite his high-angle growth pattern, he had an increased overbite (75%) with retroclined maxillary incisors. His overjet was 2 mm.
| Measurement | Pretreatment | Posttreatment | 1 year posttreatment |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 85 | 87 | 87 |
| SNB (°) | 81 | 84 | 84 |
| ANB (°) | 4 | 3 | 3 |
| Wits (mm) | −1 | 1.2 | 1.6 |
| S-N (mm) | 64.5 | 68,1 | 68,3 |
| Go-Me (mm) | 55.3 | 59.8 | 61,4 |
| A-N Pog (mm) | 4.4 | 0.5 | 0.7 |
| N/A/Pog (°) | 10 | 1 | 1 |
| S/Ar/Go (°) | 154 | 149 | 149 |
| Ar/Go/Me (°) | 138 | 135 | 135 |
| S-N/Go-Gn (°) | 39 | 31 | 32 |
| Dental | |||
| U1-NA (mm) | 0 | 4.3 | 4.7 |
| U1/NA (°) | 10 | 29 | 31 |
| L1-NB (mm) | 3 | 6 | 6 |
| L1/NB (°) | 20 | 25 | 27 |
| U1/L1 (°) | 145 | 124 | 119 |
| IMPA (°) | 78 | 87 | 90 |
| Soft tissue | |||
| Upper lip protrusion UL-NMePog (mm) |
1.3 | 0 | −0.4 |
| Lower lip protrusion LL-NMePog (mm) |
−0.5 | 1.7 | 1 |
| G ′ /Sn/Pog ′ | 20 | 17 | 17 |
In terms of soft tissue measurements, he showed a convex profile with upper lip protrusion and lower lip retrusion. The panoramic radiograph ( Fig 2 ) showed no signs of root resorption or pathologies. The third molars were present but unerupted in all dental segments. The mandibular second molars were congenitally missing. According to his hand-wrist radiograph ( Fig 2 ), his skeletal age was 12 years 6 months with a growth percentage of 85.3%, coherent with his age. His oral hygiene was moderate because of his motor dysfunction and his parents’ lack of knowledge about oral hygiene procedures. There were no symptoms of temporomandibular disorders. He was willing to undergo orthodontic treatment, and his parents were fully cooperative.

Treatment objectives and plan
Considering the abilities and the needs of the patient, our overall treatment objective was to achieve a functional and esthetically favorable result without complicated or invasive treatment procedures. Our aims were to align the dentition, correct the anterior deepbite, increase the maxillary incisor angles, and obtain a harmonious profile. Our objectives for the final occlusion were to maintain the Class II relationship of the molars and establish a Class I relationship for the canines. Accordingly, because of the severe maxillary arch deficiency, maxillary first premolar extractions for space creation were scheduled. To gain space for the mandibular arch deficiency, incisor protrusion and air rotor stripping procedures were preferred to improve the lower lip position.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


