There is no doubt that dental casts, whether plaster or digital, are one of many important tools routinely used in orthodontics for assessing dentitions or malocclusions. Unfortunately, to this day, a convincing case has still not been made for the routine mounting of all casts on articulators. Drs Martin and Cocconi, however, would like you to believe otherwise. The issue of articulator mountings in orthodontics must be considered within the broad framework of orthodontic gnathology. Under the premise of pursuing “what is best for the patient,” Drs Martin and Cocconi have conveniently left out the term “gnathology” in their “Point” article; however, the principles of gnathology (right or wrong) form the basis of their argument for using articulators. We have written and expressed the evidence-based view on gnathology and articulator mounting in orthodontics several times and advise the reader to review relevant literature for a more thorough understanding on this topic.
Drs Martin and Cocconi make many unsupported claims in their article. Statements such as the articulator “is just another tool . . .” an orthodontist can do good orthodontics without using an articulator, but an articulator can help him or her to provide better treatment in many clinical situations,” and “whether research is always good for clinical practice” fly in the face of evidence-based practice and the basic tenets of science. With comments like these, are they really putting forward an intellectual and scientific discussion on the use of articulators in orthodontics?
Clearly, several issues need to be discussed: articulators in relation to centric relation and records, centric slides, occlusion and temporomandibular disorders, and occlusion and periodontal disease.
Articulators can play a role in prosthodontics, restorative dentistry, and orthognathic surgery to maintain a certain vertical dimension for laboratory purposes. For some orthodontists, mounted dental casts help elucidate various 3-dimensional and static jaw and occlusal relationships and deviations. Nonetheless, using articulators as a routine diagnostic aid in orthodontics appears to be a perfunctory exercise. The premise for the use of articulators dates back to well over a half century ago, when occlusion and condyle position were believed to be the primary cause of temporomandibular disorders. However, the modern view is that specific occlusion, condylar position, and jaw alignment factors are no longer considered the primary causes of temporomandibular disorders. The diagnosis and treatment for temporomandibular disorders has changed from a dental-based model to a biopsychosocial model that integrates biologic, behavioral, and social factors to the onset, maintenance, and mitigation of temporomandibular disorders. A medical orthopedic approach that focuses on the biomedical sciences and musculoskeletal treatments similar to those for chronic pain are the current approaches for temporomandibular disorders. Biopsychosocial treatment approaches such as cognitive-behavioral therapies and biofeedback are contemporary treatment modalities for temporomandibular disorders. The exciting future research topics for temporomandibular disorders are genetics (vulnerabilities related to pain), central-brain processing, imaging of the pain-involved brain, endocrinology, behavioral risk-conferring factors, sexual dimorphism, and psychosocial traits and states. Conservative and reversible forms of temporomandibular disorder treatments are preferred (at least initially) over aggressive and irreversible forms. In the evidence-based view, orthodontics is considered temporomandibular disorders neutral— ie, orthodontics does not cause and will not necessarily correct or improve a patient’s temporomandibular disorder condition now or in the future. Because orthodontics has not been demonstrated to cause temporomandibular disorders, this further supports the notion that occlusion and condyle position do not cause temporomandibular disorders: ie, the premise that orthodontics could cause temporomandibular disorders is grounded in the dental-based model.
The premise for the use of articulators dates back to well over a half century ago, when occlusion and condyle position were believed to be the primary cause of temporomandibular disorders.
Of note, the evidence-based view does not argue that occlusion and condyle position have no relationship to temporomandibular disorders and that orthodontists should ignore them. The gross evaluation of the patient’s occlusion still are useful: “assessment of occlusion is necessary as part of the initial oral examination to identify and eliminate gross occlusal discrepancies.” The amelioration of gross occlusal interferences that cause tooth mobility, fremitus, and deviation or deflection on mandibular closure and movement are within the scope of the evidence-based paradigm.
Because there has been a paradigm shift regarding the etiology, diagnosis, and treatment of temporomandibular disorders away from occlusion and condyle position, occlusionists and gnathologists should reconsider and abandon age-old views and techniques that are not supported by science and evidence. Certainly, the evidence-based view on the role of occlusion in relation to temporomandibular disorders should have had a negative impact on the routine use of articulators in orthodontics. Greene wrote: “I would encourage orthodontists to be somewhat flexible in applying the standards of ideal jaw relationships as well as ideal occlusion relationships to their finishing of patients . . . we should not have conversations about tenths of millimeters when discussing where the condyle should be. . . . The failure to produce some expert’s version of a so-called good/ideal occlusion or CR position is not a risk for developing TMD.” Does it make sense to focus and study occlusion and condyle position the same way that we did more than 50 years ago?
The belief that centric occlusion or (or maximum intercuspation or intercuspal position) should be coincident with an arbitrary centric relation position is not evidence-based. The preponderance of evidence suggests that for the population at large there is a range of acceptable positions and not 1 centric relation position that is optimal for every patient. That is, a particular 3-dimensional position of the temporomandibular joint condyles in the glenoid fossa has not been found to predict temporomandibular disorders. Johnston wrote: “I know of no convincing evidence that condyles of patients with intact dentitions should be placed in CR or that once placed or that once having been placed there, the resulting improvement on nature will be stable.” Interestingly, centric slides greater than 4 mm that have been found to be associated with temporomandibular joint arthropathies are most likely the result of the temporomandibular disorders rather than the cause, contrary to the beliefs of Drs Martin and Cocconi.
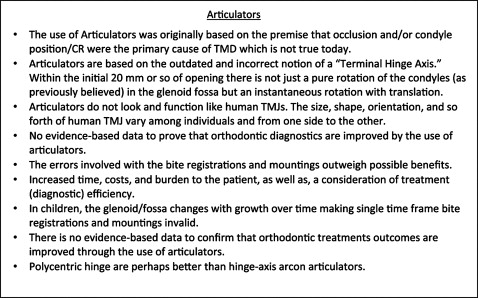
Many of the problems we have with articulators as diagnostic aids in orthodontics start before the articulator is actually used ( Fig 1 ). Centric relation records can be demonstrated to be reliable, but there is no evidence to support their validity. Nonetheless, proper attention to an orthodontic patient’s centric records is an important consideration in orthodontics and all of dentistry. We do know that doctor-generated patient centric records are more reliable than patient-generated records, but they are also less valid (physiologic). In addition, the same bite registrations used to make dental casts should be consistently used throughout all the patient records—dental models, photographs, cephalometric radiographs, and so on. And, to merely ask orthodontic patients to bite on their back teeth will not always provide an accurate centric bite registration, and one might miss diagnosing a “Sunday bite.”
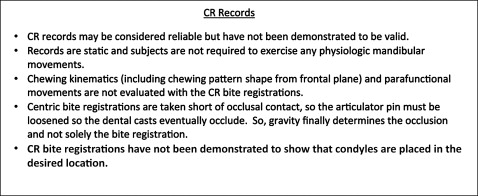
Gnathologic centric records are static and not functional ( Fig 1 ). Patients are not asked to exercise any relevant physiologic mandibular movements to generate centric relation records. Chewing kinematics are not evaluated, such as chewing pattern dynamics, which might determine whether a patient is more or less a vertical or horizontal chewer. Furthermore, the harshest occlusal forces are those generated via parafunctional mandibular movements, such as bruxing and clenching. These movements and forces are not evaluated by centric relation records and articulator mountings.
Based on information from the study of Alexander et al, clinicians, in general, cannot predict where condyles are positioned and recorded based on their particular type of centric bite registration. This makes it imperative that orthodontic gnathologists provide magnetic resonance imaging research data of the temporomandibular joints that substantiate that the subjects’ condyles are actually placed and recorded in positions determined by such registrations. In addition, the difference between gnathologic and nongnathologic diagnostics is on average as little as 1 mm or less, and this is mostly in the vertical dimension. Are such minor differences really a health concern? Also, in growing children, the temporomandibular joint condyle-glenoid fossa complex changes location with growth; the fossae on average are displaced posteriorly and inferiorly. One would therefore need to perform new mountings regularly throughout treatment to diagnose and maintain their so-called ideal centric relation position. This however does not occur.
The shortcomings of articulators in orthodontics were discussed in detail in our article and are listed in Figure 2 . Diseases of the temporomandibular joint such as disc displacement and osteoarthrosis are best diagnosed with magnetic resonance imaging of the temporomandibular joints and a clinical examination, and not with articulators. The major premise for the use of articulators is based on the incorrect concept of a “terminal hinge axis” of Posselt dating back more than a half century. Posselt conjectured that, in the initial 20 mm or so of opening and closing, the mandible (condyles) only rotates similar to a door hinge (and does not simultaneously translate). However, Posselt’s theory was made in the era when centric relation was considered a retruded, posterior position of the condyles in the glenoid fossa. During this time period, retruded centric relation was recorded with distal guided pressure applied to the chin, a probable reason for Posselt’s finding of a “terminal hinge axis.” In 1995, Lindauer et al demonstrated that, during opening and closing, the condyles not only rotate, but also simultaneously translate (move downward and forward). They demonstrated that the terminal hinge axis does not exist, and their findings support an “instantaneous center of rotation” that varies in every patient and cannot be simulated via an articulator ( Fig 2 ).