The presence of healthy soft tissue at the tooth and implant interface correlates to long-term success and stability in function and esthetics. Grafting procedures utilizing various techniques can be performed during any stage of the implant or restorative therapy. Materials of autogenous, allogeneic, and xenogeneic sources are available for oral soft tissue grafting. This article describes the classifications of soft tissue defects, treatment modalities, and materials used to enhance soft tissue quality and quantity and to achieve optimal esthetics and function around teeth and implants.
Key points
- •
The goal of soft tissue grafting is to improve prognosis, esthetics, and function of teeth and implants.
- •
New classification systems for soft tissue diagnosis have been developed.
- •
Allogenic, xenogenic, and biologic materials are increasingly used to compliment or substitute autogenous soft tissue grafts.
- •
The number of techniques and materials for oral soft tissue grafting is expanding.
Treatment of mucogingival deficiencies has become an integral part in oral and dental rehabilitation. Inadequate keratinized tissue (KT) surrounding teeth and implants can lead to recession. , Recession refers to the apical displacement of the soft tissue margin including mucosa or gingiva, whichever is present at the site. The presence of healthy tissue at the tooth and implant soft tissue interface correlates to long-term success and stability in function and esthetics. Although KT is not necessary to prevent recession in presence of good plaque control, , it does decrease recession over time. Implant success is also not absolutely dependent on the presence of gingiva ; however, adequate KT is associated with patient comfort and less inflammation around implants. Plaque is the primary etiologic factor in periodontal and peri-implant inflammation, and thicker gingiva facilitates its removal and strongly correlates with optimal tissue health around implants. Implants without KT demonstrate increased susceptibility to recession and plaque-induced tissue destruction. Esthetic demands including soft tissue surrounding for natural, restored, or implant-supported dentition have increased. Harmony is expected among teeth, implants, restorations, and adjacent soft tissue ( Fig. 1 ).

Cause of recession
Recession around teeth is a result of several predisposing factors including: anatomy; tooth position; orthodontic tooth movement; mechanical and chemical trauma; tooth brushing technique; the quantity, quality, and biotype of surrounding attached gingiva; poorly designed or maintained prosthetic devices; suboptimal restorative margins; high muscle attachment and frenal pull; and calculus and plaque control. ,
Etiologies of soft tissue defects around implants include: poor spatial positioning, excessive abutment contour and implant diameter, horizontal biologic width formation, and periodontal phenotype. Recession around implants may be partially associated with the remodeling of the peri-implant soft tissue barrier following implant placement and restoration.
Papilla
Maintenance of papillae height is predictable in healthy periodontium because of tissue rebound based on the height of interproximal bone. Complete papilla fill between teeth is possible with less than or equal to 5 mm distance from the contact point to the bone. Papilla height next to an implant depends on the adjacent tooth’s bone height (see Fig. 1 C). Adjacent implants only average 3.4 mm of soft tissue height over the interimplant bone crest (see Fig. 1 A, B, D). Surgical techniques aiming to increase the volume of papillae use platelet-rich fibrin (PRF), injection of hyaluronic acid–based gel, and connective tissue grafts (CTG) with coronally positioned flaps (CAF). To prevent loss of interproximal bone and papilla, implants should be placed 1.5 mm from adjacent teeth, and 3 mm from another implant, because vertical bone loss increases with closer proximity.
Classification of recession
An early classification of recession was introduced by Sullivan comprising four categories: (I) deep/wide, (II) shallow/wide, (III) deep/narrow, and (IV) shallow/narrow.
Miller Classification System of Marginal Tissue Recession
Miller’s classification was introduced in 1985 and it sets realistic expectations for root coverage outcomes. Class I and II groups can achieve almost complete root coverage, class III only partial, and class IV none:
-
Class I: Recession not passed mucogingival junction, no interdental bone loss
-
Class II: Recession to/passed mucogingival junction, no interdental bone loss
-
Class III: Recession to/passed mucogingival junction, some interdental bone loss
-
Class IV: Recession to/passed mucogingival junction, severe interdental bone loss
Mucogingival Deformities and Conditions Around Teeth
In 1999, the International Workshop by the American Academy of Periodontology proposed a new classification system that comprehensively diagnosed mucogingival deformities and conditions around teeth and on edentulous ridges as two subcategories under developmental or acquired deformities and conditions. This classification was modified at the 2017 World Workshop and now incorporates the interproximal clinical attachment loss measured from cementoenamel junction (CEJ) to the base of the sulcus and the assessment of the exposed root surface. ,
- a.
Gingival phenotype
- b.
Gingival/soft tissue recession
- c.
Lack of gingiva
- d.
Decreased vestibular depth
- e.
Aberrant frenum/muscle position
- f.
Gingival excess
- g.
Abnormal color
- h.
Condition of the exposed root surface
Recession Type
-
RT1: Gingival recession with no loss of interproximal attachment ( Fig. 2 )

Fig. 2 Recession type according to the 2017 World Workshop Classification. -
RT2: Gingival recession associated with interproximal attachment loss that is less or equal to the buccal attachment loss
-
RT3: Gingival recession associated with interproximal attachment loss that is greater than buccal attachment loss
Gingival Biotype
The thin periodontium has a high incidence of dehiscence and fenestration defects over which recession occurs and continues until the bone margin is reached. Gingival scallop on anterior teeth can reach 4 to 6 mm. The thick biotype is supported by thick bone resisting recession to occur and is characterized by smaller embrasures and flatter 3- to 4-mm anterior gingival scallop. Three biotypes have been described based on gingival thickness, KT width, bone morphotype, and tooth dimension ( Fig. 3 ) :
-
Thin scalloped biotype is characterized by slender triangular teeth, interproximal contacts close to incisal edge, narrow KT, and thin gingiva and alveolar bone.
-
Thick flat biotype is characterized by square-shaped teeth, prominent cervical convexity, interproximal contacts more apically, broad KT, and thick gingiva and alveolar bone.
-
Thick scalloped biotype is characterized by slender teeth with pronounced gingival scalloping, narrow KT, and thick fibrotic gingiva.

Development of mucogingival surgery
The term “periodontal plastic surgery” was introduced by Miller. , It encompasses regenerative and reconstructive surgical procedures that prevent or correct anatomic, developmental, traumatic, and disease-related defects of oral soft tissue or bone in form and function and enhance soft tissue characteristics around teeth, implants, and prosthetic restorations. , Soft tissue manipulation from adjacent or distant donor sites is generally separated into:
- 1.
Pedicle grafts
- a.
Flap advancement procedures
- •
CAF
- •
Semilunar CAF
- •
- b.
Flap rotation procedures
- •
Laterally sliding flap
- •
Partial-thickness double pedicle graft
- •
Rotational flap
- •
Transpositioned flap
- •
- a.
- 2.
Free soft tissue grafts
-
Free gingival grafts (FGG)
-
Subepithelial tissue grafts (SCTG), CTG
-
Free gingival graft
FGG was introduced in 1966 and it remains the gold standard for augmentation of KT around teeth ( Figs. 4 and 5 ) and implants ( Figs. 6 and 7 ). Additional indications include elimination of the frenal attachments, increase of vestibular depth, stabilization of progressive gingival recession, and protection of denture-bearing surfaces. The autogenous FGG is categorized by thickness into thin (0.5–0.8 mm), average (0.9–1.4 mm), and thick (1.5 to >2 mm).
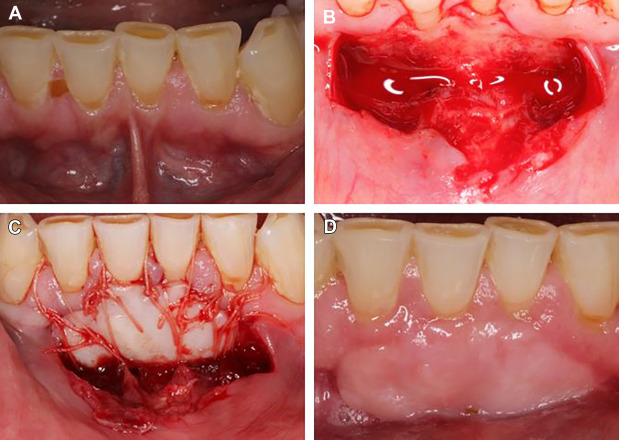



Thin grafts can increase the amount of KT, they provide the best color match, and have to be placed in intimate contact with an intact blood supply to survive (see Fig. 4 ). They heal the fastest and undergo the highest (25%–30%) secondary shrinkage. , The average thickness graft is suited for all types of grafting, it provides acceptable appearance and better protection against future recession. The thick FGG is used for covering exposed root surfaces, is more resistant to future recession, , but results in less esthetic appearance because of color and thickness incompatibility to the adjacent gingiva (see Fig. 4 ). Rapid revascularization is expected for uniform thin or intermediate grafts placed on a periosteum, whereas uneven thicker FGGs placed on bone undergo a prolonged period of revascularization and healing. , FGG can achieve root coverage in 44% and up to 89.9% of the sites or it is used as a two-stage procedure for root coverage with coronal advancement of healed graft (see Fig. 5 D–F).
Technique
The incision is made at the mucogingival junction along the recipient area extending but not involving the sulcus of adjacent teeth or implants. The initial horizontal incision should be placed at the desired new gingival level (CEJ for Miller class I and II; below the CEJ for class III and IV). Vertical incisions are placed on the lateral aspects of the horizontal incision at 90° or slightly divergent toward mucosa. Recipient site is prepared by a split-thickness dissection leaving intact periosteum, removing any aberrant frenal attachments, and de-epithelializing marginal and papillary gingiva (see Figs. 4 B, 6B and 7B ). Gingival grafts should be harvested and shaped with the recipient site in mind (see Fig. 7 C). Graft includes the overlying epithelium and can use soft tissue removed after gingivectomy, palatal, or masticatory gingiva as autogenous donor sources. Graft should be completely immobilized by sutures. Interrupted sutures on the edges enable good marginal adaptation, whereas sling sutures facilitate intimate contact with the vascular bed and elimination of the dead space between FGG and recipient bed (see Figs. 4 C, 5B , 6C and 7D ).
Subepithelial connective tissue graft
SCTG was introduced in the 1980s, , with clinical improvements compared with FGG or pedicle flaps. It comprises most grafts performed for root coverage and augmentation procedures in combination with variety of flap designs and provides long-term stability against recession relapse. The SCTG is divided by thickness into three categories: thin (0.5–0.8 mm), average (0.9–1.4 mm), and thick (1.5 to >2 mm).
Surface Treatment
Root or implant surface should be smooth and clean before receiving the SCTG. Root surface irregularities and restorations should be removed or reshaped. Root planning and chemical root surface treatment with citric acid, tetracycline, or EDTA are used to remove endotoxins and smear layer exposing dentinal tubules essential for new attachment. Chemical conditioning of dentin can stimulate the attachment of fibroblasts and gingival keratinocytes, facilitating the reformation of a junctional epithelium. Citric acid causes greater morphologic alterations than EDTA or tetracycline, , , and is not consistently supported in literature.
Recipient Site Flaps
CAF achieves better root coverage and recession reduction with addition of a graft, which provides superior long-term stability against recession relapse and reduction of KT, especially in cases with suboptimal KT. , The horizontal incision is made at the level of desired gingival margin, usually at the level of CEJ. The incision extends to the interdental area adjacent to the terminal grafted tooth ( Fig. 8 ). Vertical incisions enable increased access, but decrease blood supply and can cause scarring. They should extend beyond mucogingival junction to allow manipulation of the flap in the coronal direction ( Figs. 9 B and 10C ). Graft is sutured in place with resorbable sutures extending to the edges of the recipient bed (see Fig. 9 B). Flap should be sutured with longer lasting monofilament sutures ( Figs. 9 C and 10E ). Use of CAF is better suited for sites with minimal KT and thinner SCTG, frequently seen in Miller class I defects. In the absence of KT, SCTG with CAF results in predictable root coverage and nonkeratinized mucosa as the soft tissue margin ( Fig. 9 D).



Envelope flap was introduced with similar success by undermining partial-thickness dissection in the tissues surrounding the defect without reflecting a traditional flap or vertical incisions. Incision is placed in the sulcus and a split-thickness pouch is developed under the surface of the tissue. The recipient bed should extend to undermine papillary tissue coronally to the CEJ. The envelope flap must extend far enough laterally and apically to allow passive placement of the graft ( Fig. 9 ; Fig. 11 ). This dissection is difficult and tactile sensation guides the preparation of the recipient site among periosteum, mucosa, and gingiva. The suturing technique is also more challenging; however, fewer sutures are needed because of good graft stability. The suturing technique is designed to pull the donor tissue into the tunnel. This technique is used for augmentation of deficient soft tissue contours under fixed prosthesis or around implants (see Fig. 11 ). This flap design provides excellent graft stability and maintenance of ample blood supply from the adjacent papillary, overlying mucogingival and underlying mucoperiosteal sides.

Partially covered CTG can achieve root coverage and increase in KT because the exposed CTG keratinizes over the exposed graft surface. KT width correlates with the presurgical dimensions plus the height of the exposed graft. It is suitable for Miller class I, II, and III recession defects with deficient KT. Partially exposed CTG must be thick enough to survive over the avascular root surface. It offers the advantage in maintaining the vestibular depth and position of mucogingival junction. Exposed retained epithelial collar yields similar root coverage and better gingival augmentation compared with covered de-epithelialized graft that performs better esthetically ( Fig. 10 ).
Double pedicle flap should be considered when the objective includes the increase of KT and maintenance of mucogingival junction position (see Fig. 10 ; Fig. 12 ). Coronally advanced, double pedicle, and tunneling flaps in conjunction with an autogenous SCTG are all effective in obtaining root coverage and improving clinical parameters.





