Introduction
The purpose of this study was to investigate the effect of orthodontic treatment on oral health–related quality of life (OHRQoL) in groups of standard patients with severe malocclusions; cleft lip, cleft palate, or cleft lip and palate patients; and orthognathic surgery patients.
Methods
The study sample consisted of 83 consecutive patients undergoing treatment at the orthodontic unit of Christchurch Hospital, Christchurch, New Zealand, divided into 3 groups: 30 adolescents with severe malocclusions; 24 adolescents with cleft lip, cleft palate, or cleft lip and palate; and 29 adults with severe skeletal discrepancies requiring both orthognathic surgery and orthodontic treatment. Each patient completed the Short Form of the Oral Health Impact Profile (OHIP-14) questionnaire before and after orthodontic treatment.
Results
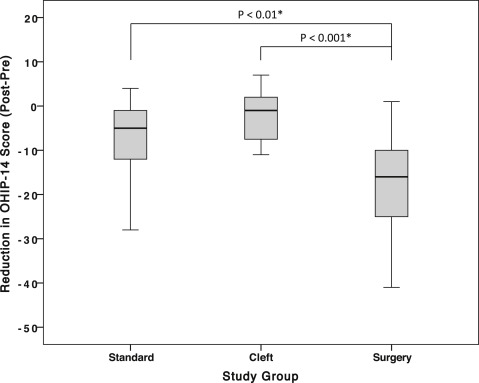
The baseline OHIP-14 subscale scores among the 3 study groups were significantly different, with the surgery patients having nearly twice the OHIP-14 scores of the other 2 groups for nearly half of the items ( P <0.05). The surgery patients experienced the greatest reduction in OHIP-14 scores (ie, improvement in OHRQoL), with the largest effect sizes reported for the psychological discomfort (+2.73) and disability (+2.65) domains. The group with clefts experienced the smallest changes in OHIP-14 scores across all 7 domains (−0.03 to +0.63). After adjusting for age and sex, the surgical patients had a significantly greater reduction in pretreatment OHIP-14 scores than did the standard and the cleft patients ( P <0.01).
Conclusions
The effect of orthodontic treatment on OHRQoL varies for different patient groups even after adjusting for age and sex. The greatest improvement in OHRQoL occurred in adults with a need for orthognathic surgery, whereas the least improvement seemed to occur in adolescents with cleft lip, cleft palate, or cleft lip and palate.
Highlights
- •
Orthognathic surgery patients have relatively poor oral health–related quality of life (OHRQoL) before treatment.
- •
Treatment-related changes in OHRQoL were mainly influenced by patient group.
- •
Orthognathic surgery patients report the greatest improvement in OHRQoL after treatment.
- •
Cleft patients have the least improvement in OHRQoL after orthodontic treatment.
Malocclusion is a relatively common condition that can adversely affect a person’s function and psychological well-being. In contrast to other medical conditions, however, most orthodontic problems do not fit the classical “disease-symptom” model. Most orthodontic patients seek treatment for purely esthetic reasons that often have an underlying psychological component. The importance of these psychological factors in influencing treatment need and outcome has resulted in a paradigm shift toward self-report assessment tools and patient-centered care. Oral health–related quality of life (OHRQoL) instruments are particularly useful in orthodontic populations because of their ability to tap into a wide range of domains including the functional, psychological, and social aspects.
The recent use of OHRQoL instruments in general and orthodontic samples has shown that many malocclusions have a significant impact on the patient’s emotional and social well-being. Children and adolescents with multiple missing teeth, large overjets, and anterior spacing are particularly susceptible to poor OHRQoL. In general, there appears to be a distinctive gradient in OHRQoL scores across the categories of malocclusion severity. This association between malocclusion and OHRQoL raises an important clinical question: Does the etiology and severity of a malocclusion influence the effect of orthodontic treatment on a person’s OHRQoL?
The degree of improvement in OHRQoL after orthodontic treatment may vary in patients with dentofacial deformities. For instance, patients with severe jaw-size discrepancies have reported marked improvements in their general quality of life and OHRQoL after orthodontic treatment and orthognathic surgery. By comparison, cleft lip, cleft palate, or cleft lip and palate (CL/P) patients, who also have severe dentofacial deformities, do not always experience similar improvements in quality of life as do those in the normal population. This lack of improvement in patients with CL/P is further compounded by a lower baseline OHRQoL in comparison with noncleft populations.
So far, the impact of orthodontic treatment on OHRQoL has been largely investigated in isolated samples, which may not necessarily be comparable. Few studies have compared the effect of malocclusion and orthodontic treatment on OHRQoL in a study sample with distinctively different etiologic and clinical backgrounds. Moreover, the validity of findings from studies investigating specific types of malocclusion and dentofacial deformities are often limited, since these studies do not usually include a comparative or control group.
The purpose of this study was, therefore, to investigate the changes between baseline and posttreatment OHRQoL scores in groups of standard, orthognathic surgery, and CL/P patients treated at the same institution. We hypothesized that different patient groups would experience varying degrees of change in OHRQoL after orthodontic treatment. Based on the findings of previous research, it was expected that the greatest improvement would occur in the patients whose underlying concerns were most addressed by treatment.
Material and methods
The overall study sample consisted of 83 consecutive patients who commenced treatment at the orthodontic unit of Christchurch Hospital, Christchurch, New Zealand, between 2005 and 2007. Treatment at the orthodontic department is usually limited to patients with severe malocclusions. The study sample consisted of patients who met the orthodontic department’s eligibility criteria, which included having a severe malocclusion (dental aesthetic index [DAI] score greater than 32), orofacial clefting, or both. Patients with diagnosed genetic syndromes were excluded from the study. Eligible participants received either single-arch (6%) or double-arch (94%) fixed appliances as part of their orthodontic treatment. All study participants were treated by an author (P.V.F.).
The study participants were classified as (1) standard patients with severe malocclusions warranting orthodontic treatment (n = 30, 36.2%), (2) surgery patients with severe skeletal discrepancies requiring both orthodontic treatment and orthognathic surgery (monomaxillary surgery, 14; bimaxillary surgery, 15; n = 29, 34.9%), and (3) nonsyndromic CL/P patients with craniofacial deformities requiring orthodontic treatment as part of their multidisciplinary management (n = 24, 28.9%). OHRQoL changes in the cleft group were mostly assessed after the last stage of orthodontic treatment, with only 3 participants likely to need orthodontic treatment or orthognathic surgery in the future.
Data were collected for the sample’s sociodemographic characteristics, treatment duration, DAI values, and baseline and posttreatment scores from the Short Form of the Oral Health Impact Profile (OHIP-14) questionnaire. This information was obtained as part of a clinical audit designed to evaluate the quality of care delivered by our orthodontic department. All study participants provided consent, and data were collected in accordance with the Helsinki Declaration of 1975.
The DAI is a common epidemiologic index used to assess and rank a person’s dental appearance on a continuous scale. The DAI consists of 10 intraoral measurements, which are multiplied by a regression coefficient to produce a weighted score for each component. The overall DAI score is calculated by adding the scores of the 10 weighted components and summing with a constant of 13. The DAI score was calculated for each participant before treatment. This score was used to classify the severity of a malocclusion into 4 distinct categories: minor (15-25), definite (26-31), severe (32-35), and handicapping (greater than 36).
The OHIP-14 is a widely used self-report questionnaire designed to assess OHRQoL. The Short Form OHIP-14 consists of 14 items that were derived from the original 49-item OHIP. The OHIP-14 items are organized into 7 domains that relate to function, pain, physical disability, psychological discomfort, psychological disability, social disability, and handicap. The participants were asked to complete the OHIP-14 based on their experiences before and after orthodontic treatment (within a 3-month window). They reported the impact for each item using a 5-point Likert-type scale (coded as 4, very often; 3, fairly often; 2, occasionally; 1, hardly ever; and, 0, never). A subject’s overall score ranged from 0 to 56, whereas domain scores ranged from 0 to 8. A higher OHIP-14 score indicated a greater impact on OHRQoL.
Statistical analysis
The data were analyzed using the Statistical Package for Social Sciences (version 20.0; IBM, Armonk, NY). Bivariate analysis was carried out using the chi-square test with the alpha level set at 0.05. Nonparametric tests (Kruskal-Wallis and Mann-Whitney U) were used whenever a continuous variable was not normally distributed. A general linear model was used to assess the changes in OHIP-14 scores between the 3 study groups after adjusting for the effect of age and sex. Bonferroni adjustment was used for post hoc multiple tests.
Effect sizes were used to determine the magnitude of the statistical difference in scores. Effect size was calculated by dividing the mean change in pretreatment and posttreatment scores by the pooled standard deviations after correcting for the amount of correlation between the 2 scores. Effect sizes less than 0.2 were minimal, 0.2 to 0.49 were small, 0.5 to 0.8 were moderate, and greater than 0.8 were large. Accordingly, a larger effect size indicated a greater change as a result of treatment.
Results
The distribution of the sexes was similar across the 3 study groups, although the surgery patients were generally older than were the CL/P and the standard patients ( Table I ). The surgery patients had longer treatment periods than the standard and CL/P patients ( P <0.001), with delays often experienced in accessing surgery. The surgery patients also had significantly higher DAI scores than their standard and CL/P counterparts ( P <0.01).
| Standard (n = 30) | CL/P (n = 24) | Surgery (n = 29) | |
|---|---|---|---|
| Sex | |||
| Male | 17 (56.7%) | 14 (58.3%) | 15 (51.7%) |
| Female | 13 (43.3%) | 10 (41.7%) | 14 (48.3%) |
| Pretreatment age (y) | 14.5 (1.9) ∗ | 12.6 (2.8) | 19.0 (4.3) |
| Posttreatment age (y) | 16.6 (2.0) ∗ | 14.4 (2.7) | 21.8 (4.0) |
| Length of treatment (mo) | 25.2 (6.4) ∗ | 21.7 (9.1) | 33.6 (11.9) |
| DAI ‡ | 45.5 (9.0) † | 45.4 (13.4) | 56.6 (12.8) |
The baseline OHIP-14 scores of the 3 study groups were significantly different for nearly half of the 14 items. Surgery patients had nearly twice the baseline OHIP-14 score of the other 2 groups for most of these items ( P <0.05). There were a number of statistically significant differences among the 3 groups at the posttreatment stage. The CL/P patients had significantly higher posttreatment OHIP-14 scores for several items, including “trouble pronouncing words,” “self-conscious,” “feeling tense,” “difficulty relaxing,” “irritable with others,” and “unsatisfying life” ( P <0.05).
The mean changes in OHIP-14 score after treatment are presented in Table II . Surgery patients experienced significant improvements in all of the OHIP-14 domains. For the surgery group, the effect size ranged from +1.25 to +2.73; this indicated a large and significant improvement in OHRQoL after treatment. The largest effect sizes in the surgery group were noted in the psychological discomfort (+2.73) and disability (+2.65) domains. The standard patients also experienced significant improvements in the physical pain, handicap, psychological discomfort, and psychological disability domains. The greatest effect sizes in the standard group were also noted in the psychological discomfort (+1.21) and disability (+1.15) domains. Conversely, the CL/P group experienced no significant changes between baseline and posttreatment mean OHIP-14 scores in any of the 7 subscales. The effect sizes for the CL/P patients ranged from −0.03 to +0.63, indicating small-to-moderate changes in OHRQoL after treatment. Overall, the surgery and the standard patients experienced large improvements in their total OHIP-14 scores, with effect size means of +2.59 and +1.11, respectively. In contrast, there was a considerably smaller improvement in the CL/P group (effect size, +0.52). The post hoc power of nonsignificant statistical tests in the standard group ranged from 68.3% for the physical disability domain to 91.5% for the social disability domain. In the CL/P group, the post hoc power of nonsignificant statistical tests was particularly low for the physical pain domain (5.2%); the remaining tests ranged from 41.2% for the functional limitation domain to 84.0% for the social disability domain.
| Standard (n = 30) | CL/P (n = 24) | Surgery (n = 29) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (SD) | Posttreatment (SD) | Mean change (SD) | Effect size ∗ | Baseline (SD) | Posttreatment (SD) | Mean change (SD) | Effect size ∗ | Baseline (SD) | Posttreatment (SD) | Mean change (SD) | Effect size ∗ | |
| Functional limitation | 1.23 (1.50) | 0.77 (0.86) | 0.47 (1.55) | +0.47 | 1.75 (1.68) | 1.37 (1.21) | 0.38 (1.50) | +0.37 | 2.03 (2.10) | 0.24 (0.58) | 1.79 (2.19) ‡ | +1.36 |
| Physical pain | 1.50 (1.83) | 0.67 (1.27) | 0.83 (2.23) † | +0.58 | 1.25 (1.70) | 1.29 (1.60) | −0.04 (1.83) | −0.03 | 3.10 (1.90) | 0.86 (1.27) | 2.24 (2.29) ‡ | +1.25 |
| Psychological discomfort | 3.00 (2.52) | 0.70 (1.37) | 2.30 (2.94) ‡ | +1.21 | 2.54 (2.32) | 1.75 (1.85) | 0.79 (1.74) | +0.62 | 4.83 (2.41) | 0.48 (1.12) | 4.35 (2.45) ‡ | +2.73 |
| Physical disability | 0.73 (1.60) | 0.23 (0.73) | 0.50 (1.61) | +0.46 | 0.75 (1.29) | 0.33 (1.09) | 0.42 (1.14) | +0.44 | 1.59 (1.68) | 0.10 (0.41) | 1.48 (1.70) ‡ | +1.58 |
| Psychological disability | 2.67 (2.43) | 0.67 (1.16) | 2.00 (2.67) ‡ | +1.15 | 1.92 (2.15) | 1.33 (1.71) | 0.58 (1.91) | +0.43 | 3.93 (1.91) | 0.24 (0.58) | 3.69 (2.14) ‡ | +2.65 |
| Social disability | 1.27 (2.16) | 0.37 (1.03) | 0.90 (2.22) | +0.63 | 1.17 (1.74) | 0.58 (0.88) | 0.58 (1.67) | +0.63 | 2.00 (2.27) | 0.03 (0.19) | 1.97 (2.26) ‡ | +1.72 |
| Handicap | 1.20 (1.61) | 0.23 (0.68) | 0.97 (1.75) † | +0.90 | 1.1 (1.45) | 0.58 (1.14) | 0.54 (1.29) | +0.51 | 2.03 (1.35) | 0.07 (0.37) | 1.97 (1.50) ‡ | +2.01 |
| Overall | 11.60 (10.93) | 3.63 (5.04) | 7.97 (12.03) ‡ | +1.11 | 10.50 (10.80) | 7.25 (7.28) | 3.25 (8.50) | +0.52 | 19.52 (9.62) | 2.03 (3.13) | 17.48 (10.21) ‡ | +2.59 |
∗ Effect size (Cohen d) was calculated based on the pooled standard deviations corrected for the correlation between the pretreatment and posttreatment OHIP-14 scores.
Changes in OHIP-14 scores were not influenced by sex (F = 2.4; P = 0.124) or age (F = 0.57; P = 0.811), but they differed significantly for study group (F = 7.92; P = 0.001). Post hoc tests showed that the surgery patients had a significantly greater reduction in OHIP-14 scores (ie, improvement) than did both the standard and the CL/P groups ( Fig ).
The OHIP-14 scores of the CL/P group were further analyzed by cleft type ( Table III ). There were no statistically significant differences between the subgroups in terms of age, sex, or DAI score ( P >0.05). Patients with clefting of both the lip and the palate or of just the lip had similar baseline OHIP-14 scores to those with cleft palate. Patients with cleft lip and palate, and cleft lip only, however, experienced a smaller decrease in their baseline OHIP-14 score after treatment, suggesting less improvement in OHRQoL, whereas those in the cleft palate sample reported a nearly 50% reduction ( P >0.05). Patients with clefting of both the lip and the palate or of just the lip had higher posttreatment scores for most of the OHIP-14 domains, although this was not statistically significant ( P >0.05). The post hoc power of these statistical comparisons, however, was always below 20%.
| Cleft palate only (n = 9) | Cleft lip only or cleft lip and palate (n = 15) | |
|---|---|---|
| Mean overall baseline score (SD) | 10.9 (12.2) | 10.3 (10.3) |
| Functional limitation | 2.2 (1.8) | 1.5 (1.6) |
| Physical pain | 1.4 (2.0) | 1.1 (1.6) |
| Psychological discomfort | 2.3 (2.2) | 2.7 (2.5) |
| Physical disability | 0.9 (1.5) | 0.7 (1.2) |
| Psychological disability | 1.9 (2.4) | 1.9 (2.1) |
| Social disability | 1.2 (1.8) | 1.1 (1.8) |
| Handicap | 0.9 (1.5) | 1.3 (1.4) |
| Mean overall posttreatment score (SD) | 5.2 (6.5) | 8.5 (7.7) |
| Functional limitation | 1.1 (1.2) | 1.5 (1.2) |
| Physical pain | 0.9 (1.2) | 1.5 (1.8) |
| Psychological discomfort | 1.3 (1.8) | 2.0 (1.9) |
| Physical disability | 0.1 (0.3) | 0.5 (1.4) |
| Psychological disability | 0.9 (1.4) | 1.6 (1.9) |
| Social disability | 0.3 (0.5) | 0.7 (1.0) |
| Handicap | 0.6 (1.3) | 0.6 (1.1) |
| Mean overall OHIP-14 change (SD) | 5.7 (11.5) | 1.8 (6.1) |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


