Dental trauma from sport: complex injury to the dental hard tissue, periodontal ligament, supporting bone, and the oral soft tissues. (Photo credit: Dr. Paul Nativi)
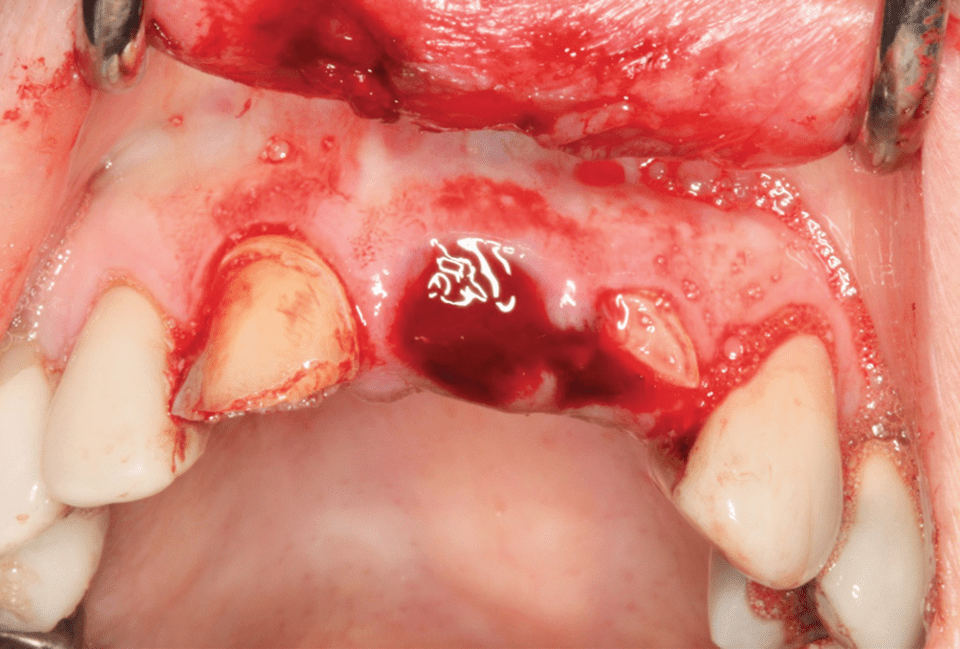
Complex dental trauma resulting from sport: crown fracture, avulsion, crown-root fracture, and soft tissue trauma. (Photo credit: Dr. Mark Roettger)

Participation in youth sports continues to grow exposing more young athletes both male and female to dental trauma from sport. (Photo credit: Dr. Mark Roettger)
Nature of Dental Trauma
-
Involving multiple tissues
-
Damage to intercellular components; tearing
-
Damage to cellular systems; crush, desiccation, contamination
-
Tx aimed at resolving all damage

3.1.1 Dentoalveolar Complex
This chapter focuses on trauma to the dentoalveolar complex. This complex of tissues consists of five tissue compartments, and together they make up the dentoalveolar complex. First the gingival-periosteal complex is composed of the gingiva, free gingiva, attached gingiva, and junctional epithelium as well as the periosteum covering the alveolar process. Second, the compartment is the periodontal ligament cementum complex . Third is the alveolar bone and marrow complex . The fourth is the dentin-pulp complex , and finally there is the oral mucosa-skin complex . The dentoalveolar complex is a very specialized area that allows the emergence of the dentition from the alveolar bone and consists of unique and specialized cells and tissues ([3], pp. 72–96).
3.2 Pathophysiology: Dentoalveolar Trauma
Energy is transferred from an object to the dentoalveolar structures, and as these structures absorb the energy transferred, the damage to normal anatomy occurs. Sporting objects such as balls, pucks, sticks, and opponents’ body parts are the major causes of this energy transfer through the dentoalveolar complex, and these same sporting objects and body parts can trap the soft tissues of the oral cavity against the teeth causing soft tissue damage. These injuries to the dentoalveolar complex can occur in two basic ways, first by direct trauma where a ball, stick, elbow, knee, or other sports implement directly strikes the teeth. Direct trauma injuries usually affect the maxillary anterior teeth, and the injuries most likely encountered in direct trauma are luxation injuries, tooth avulsion, and all types of dental fractures. The energy of impact may also determine the type and the severity of damage as a result of trauma to the oral cavity. High-velocity low-mass-type injuries such as a ball striking the teeth tend to cause damage to the dental hard tissues and less damage to the supporting structure such as the periodontal ligament (PDL) or the alveolar process. The energy of the impact is dissipated in creating the tooth fracture and is not transferred to the supporting tissues. Conversely, low-velocity, high-mass-type injuries such as the teeth striking the ground or other playing surfaces tend to cause more damage to the supporting structures causing fewer dental fractures and more damage to the supporting structures leading to more luxation and avulsion injuries. A second mechanism of dental injury is indirect trauma . This is seen when the mandibular teeth are forcefully crashed into the maxillary teeth. Indirect trauma causes more damage to the posterior teeth than direct trauma, as well as trauma to other craniofacial structures. Injuries resulting from indirect trauma include crown/root fractures of posterior teeth, mandibular fractures [3], temporomandibular joint injuries, and brain concussion (see more in ► Chap. 5).
Dentoalveolar trauma creates complex injuries affecting multiple tissues. There is potential damage to dental hard tissues, osseous hard tissues, dental pulp, periodontal ligament, mucosa, nerves, vessels, intercellular components, and cellular systems. Successful treatment of dentoalveolar trauma must be aimed at resolving damage to all the cellular and intercellular systems. To do this effectively, the sports dentist needs to have a working knowledge of basic wound healing principles.
3.3 Principles of Wound Healing
All wounds ultimately heal; it is how they heal that determines the long-term function of damaged tissues and the outcome of treatment. The goal of all trauma management is to restore damaged tissues to original form and function; this is regeneration of damaged tissues . Repair of damaged tissues is where the damaged tissues are replaced by scar tissues which restores continuity of tissue but does not restore original form and function. In dentoalveolar trauma, we also identify failure healing especially when describing healing of the dental pulp and periodontal ligament. Failure healing in the pulp would be pulp necrosis or infection, and in the periodontal ligament, failure healing would be inflammatory resorption. There is another term used in wound healing and that is tissue metaplasia which is used when one type of tissue is replaced by another type of tissue after trauma occurs [1].
Healing of most wounds in the human body whether made by surgery or trauma is through the process of repair and the formation of scar tissue which can and does alter the structure and function of the organ affected. Dental tissues are unique when compared to the rest of the body due to their marked capacity for regeneration. Injuries to the dental pulp and periodontal ligament may heal by regeneration restoring normal form and function or by repair with scar tissue or bone. Repair of the injured dental pulp results in pulp canal obliteration (PCO), and repair of the periodontal ligament results in ankylosis and replacement resorption. Regeneration of dentoalveolar tissues is the key to complete recovery from trauma, and while the dental tissues exceed many other tissues in their capacity for regeneration, many oral wounds heal by repair as we will see later in this chapter ([3], pp. 62–132, [4]). There are research efforts underway presently that look into cell transplantation or use of bioactive molecules such as enamel matrix proteins to tip the scales in favor of regeneration over repair. Regenerative biology is a very active field within medicine today, and progress is being made on multiple fronts including dentoalveolar trauma healing [5]. Where we currently have some influence over healing in dental trauma cases, is the timing of treatment as in replantation of avulsed teeth and in the control of infection during healing in all types of dental trauma.
Dental Trauma: Healing Outcomes
Regeneration: Pulp → revascularization
PDL → normal PDL
Repair: Pulp → pulp canal obliteration
PDL → replacement resorption (ankylosis)
Failure: Pulp → pulp necrosis
PDL → inflammatory resorption
All wounds heal; it is how they heal that determines outcome.
3.4 Preparation: Dentoalveolar Trauma
Management of dental trauma requires some preparation in order to provide the best care to the patient when it happens. Dental trauma occurs with no regularity, and it cannot be anticipated, so having appropriate materials available in the dental office or in a team dentist kit is strongly suggested. Treatment planning resources are useful, and two recommendations would be “Traumatic Dental Injuries: A Manual; Third Edition” [6] and an online reference “IADT Trauma Guide” (► www.dentaltraumaguide.org) [7]. Both of these references in addition to this book are helpful because they are easy and quick to use for use at the time of trauma. The definitive resource for dental trauma remains “Textbook and Color Atlas of Traumatic Dental Injuries to the Teeth” [3]. The latter is a comprehensive volume on dental trauma and is recommended for study and preparation when no patient is in need of care. Additionally preparation for dental trauma requires appropriate materials, most of which can be found in a dental clinic: restorative materials, endodontic supplies and equipment, dental splint materials, dental storage media, and surgical supplies. There are recommendations for on-field dental emergency kits in the final chapter of this book.
3.5 Examination of the Dentoalveolar Trauma Patient
Dentoalveolar trauma is considered an emergency and requires thoughtful care to relieve pain, control bleeding, and replace teeth to their proper position in the dental arches. Treatment requires diagnosis, and diagnosis requires thorough examination of the injured patient. Serious dental trauma is an emotional injury and often patients, parents, or concerned onlookers bring a high level of anxiety to the operatory where the examination is taking place. This requires the practitioner to be comfortable and confident in his or her ability to examine and ultimately manage the trauma patient. Inaccurate examination of a trauma patient can lead to improper diagnosis and treatment of a patient. To avoid inaccuracy in examination, we need to take a systematic approach to the evaluation of the trauma patient.
One area where we may need to deviate from our systematic approach to the trauma patient will be in the case of tooth avulsion. These injuries as we will see later in this chapter require immediate treatment to maximize healing potential. After appropriate tooth reimplantation is completed, and systematic examination of the patient can continue.
Dentists should never treat a stranger. This concept was made famous by William Osler who was a Canadian physician who was instrumental in the formation of Johns Hopkins Hospital. We need to know a significant amount of history medical, dental and personal, about any patient that we treat and this holds true for the trauma patient. We accomplish this in the trauma patient, who may be a new patient to the treating dentist, through systematic examination using a trauma checklist.
Trauma Checklist
|
5 Consent for treatment (emergency) |
5 Clinical exam extraoral |
|
5 Emergent care CAB |
5 Facial bones |
|
5 Airway and vitals |
5 Nose |
|
5 Medical history |
5 Eyes |
|
5 Dental history |
5 Clinical exam intraoral teeth and soft tissue |
|
5 Previous injury? |
5 TMJ exam |
|
5 HPI |
5 Imaging |
|
ʿ When |
5 Conventional |
|
ʿ Where |
5 CBCT |
|
ʿ How |
3.5.1 Medical History
This important part of the examination is where the clinician gets to know the patient. This also is where the important process of emergency consent for treatment is accomplished. We also inquire about patient allergies to medications, past bleeding disorders, the need for antibiotic prophylaxis, history of seizures and medications currently being taken by the patient, cardiovascular conditions, and potential airway issues ([8], pp. 105–131).
3.5.2 Dental History
- 1.
When did the injury occur? This gives us important information of time passed which will give us insight as to the prognosis of our treatment.
- 2.
What happened or how did the injury occur gives information and acuity on the mechanism of the trauma and what type of tissue damage we should be looking to find. Also, these questions can shed light on the possible severity of the injuries.
- 3.
Where did the injury occur can tell us about the severity of the injury as well as the issues of contamination of the traumatized tissues and tell us about the need for antibiotic coverage and need for tetanus booster.

Record of dental trauma. (Credit: Academy for Sports Dentistry)
Asking these open-ended questions of the patient is obviously important information as described above, but in addition, the accuracy of the answers can be the beginning of the next phase of our systematic examination of the trauma patient by providing clues to the patient’s cerebral function.
3.5.3 Brief Neurologic Examination
Trauma to the dentoalveolar structures which are close to the brain means that there can be concomitant neurological damage in these patients. If patients come directly to the dental office and are not cleared by medical personnel, we need to conduct a brief neurological exam as a part of a complete trauma examination. Neurological deficits will require referral to appropriate medical providers for evaluation. This brief neurological exam should begin with a cursory cranial nerve assessment where we can test selected cranial nerves and determine if they are intact or weak and if this is asymmetrical ([8], p. 684, 702). More information on cranial nerve evaluation can be found in ► Chap. 5.
A quick neurological history can also be taken from the patient. A series of questions can help determine the need for medical referral. Question the patient as to presence of headache, lethargy, nausea and vomiting, loss of consciousness, and amnesia. A positive response to presence of any of the above should generate a medical consult. It is also useful to determine the patient’s orientation to their surroundings. Orientation × 3 represents that the patient knows who they are, where they are, and the approximate time. Any deficit to orientation should also generate a medical referral.
Any suspicion of intracranial bleeding needs to be followed by appropriate medical personnel immediately.
3.5.4 Clinical Exam of the Head and Neck
This topic is covered more completely in ► Chap. 5 on maxillofacial injuries but is mentioned here as a part of the systemic evaluation of the dentoalveolar trauma patient. We begin this part of the assessment with a look at the skin, looking for disruptions causing bleeding. We will look for abrasion, contusion, laceration, edema, and ecchymosis. The patterns of soft tissue injuries to the face may give clues to how the trauma occurred as well as potential underlying bone trauma ([9], pp. 491–518).
As we survey the skin of the head and neck , we also begin our evaluation of the underlying bony structures, maxilla, mandible, bony orbit, zygoma, and frontal bones and sinuses. At this level of the evaluation, we look for signs of fracture such as mobility, crepitus, tenderness, and facial asymmetry. Signs of facial fractures will trigger referral to oral surgery personnel, remembering that facial fractures can compromise the patient’s airway ([9], pp. 491–518, [10]).
Nasal fractures are some of the most common of the facial fractures, and the nose should be evaluated looking for epistaxis or displacement of the nasal complex.
Trauma to the face can and does result in eye injuries. These can be caused by direct trauma or by fractures of the bony orbit. The two most common sports injuries to the eye are corneal abrasion and hyphemia. Corneal abrasion is usually a minor, although painful, injury to the eye. Most minor corneal abrasions will heal in a few days, but more severe abrasions may cause permanent damage to the eye, so they should be evaluated by an ophthalmologist. Hyphema is bleeding between the cornea and the iris and is often caused by blunt force trauma to the eye. Again most hyphemas resolve with no treatment; traumatic hyphema has an increased chance to raise intraocular pressure, so they should be followed by ophthalmology [8].
Examination of the ears can help rule out more serious injuries. Check to see if the ears are clear of fluid. If there is fluid in the ears, it may be cerebrospinal fluid, and the patient should be immediately referred to the appropriate medical providers.
3.5.5 Temporomandibular Joint (TMJ) Evaluation
Again this topic will be addressed more completely in ► Chap. 5 but is mentioned here as a part of our dentoalveolar trauma checklist. We will do a cursory TMJ evaluation to see if further evaluation is indicated. Have the patient open and close a few times and inquire about joint pain on opening or closing. Measure the inter-incisal opening in mm to see if there is normal range of motion. As the patient opens and closes, look for deviations to the right or to the left during both opening and closing. Listen and feel for clicks, pops, or disruptions in smooth rotation and translation of the temporomandibular joint. Check the occlusion of the teeth for open bites anterior or posterior and deviations in occlusion right or left. We are, in this cursory examination, ruling out condylar fractures or hemarthrosis of the temporomandibular joint ([9], p. 627).
3.5.6 Intraoral Examination
Looking inside the mouth for damage from trauma should continue systematically. The intraoral examination begins by inspecting the soft tissues. Look for abrasions, contusions, and lacerations. Through and through, lacerations of the lips require meticulous care to avoid disfigurement. It is imperative that both the cutaneous and the mucosal sides of these wounds are closed to insure proper healing. This will be discussed in more detail later in this chapter. Any time there are fractured teeth with tooth fragments that are not located, it must be assumed that they may be embedded in the soft tissue wounds. Careful exploration and imaging will help to locate or rule out embedded tooth fragments in soft tissue. Lacerations of the gingiva are often associated with tooth luxation. Contusions may signal more injuries below the surface tissue. Contusion of the floor of the mouth may indicate a mandibular fracture.
A check of the patient’s occlusion will help to locate possible displaced teeth or disruptions that could indicate a bony fracture. Open bites may indicate fractures or possibly hemarthrosis of the temporomandibular joint. Assessing the overjet may indicate the possibility of previous injury, considering the propensity of traumatic injury to maxillary incisors in patients with severe overjet.
Many dental injuries will be evident upon initial inspection of the teeth. Luxations and most dental fractures are obvious and usually easy to find. Cleansing the teeth and careful examination of the teeth using direct vision and transillumination can reveal more subtle damage to the dental tissues. While evaluating dental fractures, it is important to record whether the fractures involve enamel only, enamel and dentin (simple fractures), or enamel, dentin, and pulp (complex fractures). Examination of complex dental fractures that involve the dental pulp includes an assessment of the pulp seen. Determination of the condition of the pulp from bleeding to ischemic to necrotic can indicate the possibility of concomitant periodontal ligament issues and may alter treatment plans. Fractures that also include cementum are crown-root fractures and should be evaluated to determine the restorability of the tooth.
Examination of the dental trauma patient also includes mobility tests for all of the teeth, also noting loose and missing teeth. If any teeth are missing and unaccounted for, the patient should be referred for chest and abdominal imaging to rule out aspiration or swallowed teeth. Loose teeth are assessed for displacement that requires reduction and splinting. Displaced teeth that interfere with normal occlusion require more immediate treatment than those that do not interfere with biting or chewing.
Percussion tests are helpful to assist in the examination of the dental trauma patient. Finding pain on percussion helps to determine the imaging plan for the patient. High ankylotic tone can indicate lateral luxation or intrusive luxation injuries [6]. Dull ankylotic tone may indicate luxation-type injuries.
Pulp sensitivity is usually a help in determining the extent of a dental injury. Thermal and electronic testers assess the nerve supply to the dental pulp. Pulp testing following traumatic dental injuries is controversial. There are many false-negative and false-positive reading early in the post-trauma time period. Some may be due to the nature of the trauma, while other failures may result from the fact that a calm relaxed patient is needed to get accurate pulp sensibility readings, and this is usually not the case in the immediate post-trauma time period. Patients and family members tend not to be calm and relaxed. Pulpal sensibility tests immediate post-trauma may be helpful to determine a baseline when accurate readings can be obtained [11].
3.5.7 Imaging of Dentoalveolar Trauma
Initial radiographic examination for suspected dental trauma should include intraoral periapical radiographs. In cases of suspected concussion, a periapical radiograph may reveal no change or slight widening of the PDL spaces. Follow-up radiographic examinations conducted months or years after the trauma may demonstrate reduction in the size of the pulp chamber and root canals. In addition, such radiographic examination may also reveal refining osteitis or internal root resorption. Although a periapical radiograph may provide important diagnostic information about luxation, a CBCT scan helps in ruling out labial or palatal displacement of a root. In addition to the status of the tooth, a CBCT scan is more reliable in ruling out fracture of the alveolar bone. However, scans of patients with multiple coronal or endodontic restorations may be degraded due to image artifacts. Small fractures can remain undetected in scans with image artifacts.
For patients with suspected horizontal root fracture, multiple periapical radiographs at different vertical angulation should be acquired. Such multiple exposures can reveal a fracture which may remain undetected with a single exposure if the central beam of the X-ray did not travel through the line of fracture.
For vertical root fracture, a CBCT scan at a high resolution is a better examination than periapical radiography when the tooth is not endodontically treated. However, the superiority of a CBCT scan is not proven when a tooth is endodontically treated.
Since a large number of sports-related dental traumas occur in young children, CBCT scan time should be short to minimize motion. In addition, the field of view should be limited to area of question. A smaller field of view can also be obtained at a higher resolution. A large field of view scan often can be obtained only at a lower resolution.
3.6 Classification of Dental Trauma
Diseases and conditions are classified to allow study and definition of pathology, treatment, and prognosis. Dental trauma has been classified in a number of ways over the years regarding factors such as anatomic location, urgency of treatment, etiology, treatment, and pathology. We will review two methods of classification that can be useful to interprofessional teams of providers responsible for the oral care of athletes.
3.6.1 World Health Organization Classification
This classification uses anatomic factors in classifying dental trauma. It is from the Application of the International Classification of Diseases to Dentistry and Stomatology adopted by the World Health Organization (WHO) [12]. The WHO classification includes injuries to the dental hard tissues and dental pulp, injuries to periodontal tissues, injuries to the supporting bone, and injuries to the gingiva or oral mucosa (see “WHO Classification of Dental Trauma” in ► Chap. 2).
3.6.2 Classification of Dental Trauma by Treatment Urgency

Duty instruction: dentoalveolar trauma. (University of Minnesota Medical Center Dental Service)
Classification of Dental Injuries: Anatomical
- 1.
Injuries to dental hard tissues and pulp
-
Enamel fracture
-
Enamel-dentin fracture (simple)
-
Complex crown fracture
-
Crown-root fracture
-
Root fracture
-
- 2.
Injuries to the periodontal tissues
-
Concussion
-
Subluxation
-
Extrusive luxation
-
Lateral luxation
-
Intrusive luxation
-
Avulsion
-
- 3.
Injuries to gingival or oral mucosa
-
Laceration
-
Contusion
-
Abrasion
-
Always look for combination of injuries!!!
3.7 Injuries to the Hard Dental Tissues and the Pulp
This section will describe fractures to the tooth in all areas and covers fractures to the crown of the tooth, fractures that involve the crown and root, and fractures that involve the root of the tooth.
3.7.1 Crown Fractures

Simple crown fracture of maxillary central incisors; note no exposure of the pulp is seen. (Photo credit: Mark Roettger DDS)

Complex fracture of left central incisor; note exposure of the dental pulp. (Photo credit: Mark Roettger DDS)
Radiographic Findings of Crown Fracture
The lost part of the tooth can be seen on normal dental radiographs, but infractions are often times not seen on dental radiographs.
Pathophysiology of Crown Fractures
Crown fractures alone have few biologic issues. Exposed dentin after a fracture can allow bacteria or their toxins to transport the dentinal tubules to the pulp to cause pulpal inflammation . The severity of the inflammatory reaction is dependent on the health of the pulp tissue. Covering the dentin with the tooth fragment or dental restorative materials will usually allow complete pulp healing after a simple crown fracture. There is significant confusion in the dental community on the proper management of complex crown fractures which leads us to: Common Misconception #1: Every traumatic pulp exposure requires endodontic treatment.
Misconception #1: Every Exposed Pulp Needs to Be Extirpated

In fact, most traumatic exposure of the pulp can be treated by direct pulp capping or by partial pulpotomy, and a 90–99% success rate can be expected even if the pulp has been exposed to the oral environment for multiple days [14].
Emergent Treatment of Traumatic Crown Fractures
Complex crown fracture requires minor pulpal therapy prior to the dental restorative work. Direct pulp cap involves placement of calcium hydroxide over the pulp exposure prior to restoration. Partial pulpotomy sometimes called the Cvek-type pulpotomy (after Dr. M. Cvek) involves removing some of the pulp tissue at the site of exposure. A new round diamond bur in a high-speed handpiece is used to remove 2–3 mm of pulp tissue. When pulpal hemostasis is achieved, calcium hydroxide or mineral trioxide aggregate (MTA) is placed over the pulpal wound. Resin-modified glass ionomer cement is placed over the calcium hydroxide or the MTA. Calcium hydroxide has high success rates in traumatic pulp exposures, and MTA has slightly improved success rates in the same traumatic exposure category [15–17]. MTA has a much higher cost per treatment than calcium hydroxide and has the issue of tooth discoloration after use. When the pulp treatment is accomplished, the tooth fracture can be restored like any other by bonding the fragment, composite restoration, or fabrication of an esthetic crown. This will be covered in detail in ► Chap. 6.
Treatment Schemes Traumatic Pulp Exposure
- 1.
Pulp was normal prior to trauma.
- 2.
Intact vascular supply to pulp after trauma.
- 3.
Use of appropriate capping or amputation technique.
- 4.
Exclusion of bacteria during treatment and healing.
- 5.
RCT is not automatically indicated for tx of traumatic exposures!!!
- 6.
If absence of pulp is desired (post), the pulp should be extirpated.
Pulp Capping vs. Partial Pulpotomy
|
Pulp capping |
Partial pulpotomy |
|
1. Isolate with rubber dam |
1. Isolate with rubber dam |
|
2. Fx surface cleaned with CHX and hypochlorite |
2. Fx surface cleaned with chx |
|
3. Ca(OH)2 or MTA is applied to pulpal wound |
3. Use round diamond bur to prep to a depth of 2–3 mm |
|
4. Restore with bonding; fragment bonding |
4. Hemostasis |
|
5. Thin layer of Ca(OH)2 or MTA |
|
|
6. Layer of resin-modified glass ionomer |
|
|
7. Restore with bonding or bonding fragments |
Outcomes of Crown Fracture Treatment

a Simple crown fracture from a basketball injury. b Treatment of crown fracture by bonding fragment. (Photo credit: Mark Roettger DDS)

a Softball injury: hit by the ball creating a luxation injury to the right central incisor and a complex fracture to the left central incisor. b Luxation injury has been splinted to stabilize, and in this view, the pulp exposure on the left central incisor is evident. c The luxated right central incisor splinted and the fractured left central incisor has been treated with calcium hydroxide Cvek pulpotomy and composite bonding to restore tooth structure. (Photo credit: Mark Roettger DDS)
Pulp Capping vs Partial Pulpotomy
|
Pulp capping |
Partial pulpotomy |
|
1. Long-term studies show very high success rates with respect to pulp survival 90–95% |
1. Long-term studies show very high success rates with respect to pulp survival 95–99% |
|
2. That is without concomitant luxation injuries |
2. That is without luxation injury |
3.7.2 Crown-Root Fractures

a Crown-root fracture from a curling injury; note the hinge axis on the palatal side of the tooth. b Coronal fragment removed and cleaned. c Fragment removed, hemostasis achieved in palatal tissues, and Cvek pulpotomy completed. d Fragment bonded back over the root. The tooth is awaiting definitive restoration. (Photo credit: Mark Roettger DDS)
Radiographic Findings Crown-Root Fracture
Radiographic examination of crown-root fractures is rarely helpful in making a diagnosis on in establishing a prognosis. The radiograph will likely show the facial fracture line but seldom show the apical extent of the hinge portion of the fracture. Radiographic examination can be helpful in seeing the extent of a proximal crown-root fracture in an anterior tooth. Also radiographs can be used to evaluate the root of the tooth.
Pathophysiology of Crown-Root Fractures

Biologic width graphic showing the relationship of the sulcus to the crest of the alveolar bone. (Credit: ► www.speareducation.com)
Emergent Treatment of the Crown-Root Fractured Tooth
- 1.
Fragment removal only
- 2.
Fragment removal and ostectomy
- 3.
Fragment removal and surgical extrusion of the tooth
- 4.
Fragment removal and orthodontic extrusion of the tooth
- 5.
Extraction of the tooth and placement of dental implant
Fragment removal only is reserved for cases where the apical extent of the fracture is near the cementoenamel junction (CEJ) and where there is no pulp exposure. In these cases, the loose fragment is removed as soon after the injury as possible, and the tooth is restored with composite only supragingivally (◘ Fig. 3.10). Meticulous oral hygiene is required to allow appropriate gingival healing after restoration.

a Bicycle accident simple crown fracture #7 and crown-root fractures on #8 and 9 with subluxation. b Trauma from incisal view. c Crown fragments removed and pulp is exposed. d Teeth #8 and 9 have been treated with Cvek pulpotomy with white MTA and covered. e Crown fragment #8 bonded back and a denture tooth added to the splint for #9 to allow possible eruption. f Temporary restoration; plans considered for orthodontic extrusion at a later date. (Photo credit: Mark Roettger DDS)


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


