The most widely used method for controlling pain during dental procedures is the intraoral administration of local anesthetics in close proximity to a specific nerve or fiber to obtund nerve conduction. The most commonly anesthetized nerves in dentistry are branches or nerve trunks associated with the maxillary and mandibular divisions of the trigeminal nerve (cranial nerve V). However, other nerves may be inadvertently affected by intraoral local anesthesia injections, resulting in anesthetic complications of structures far from the oral cavity. Practitioners should be aware of potential ocular complications following intraoral injections in dentistry. These complications include oculomotor paralysis and vision loss. The knowledge of these conditions and their potential cause should alert the dentist to the importance of appropriate injection techniques and an understanding of management protocol.
The most widely used method for controlling pain during dental procedures is the intraoral administration of local anesthetics. The anesthetic solution is deposited in close proximity to a specific nerve or fiber to obtund nerve conduction. The most commonly anesthetized nerves in dentistry are branches or nerve trunks associated with the maxillary and mandibular divisions of the trigeminal nerve (cranial nerve V). However, other nerves may be inadvertently affected by intraoral local anesthesia injections, resulting in anesthetic complications of structures far from the oral cavity.
One such distant complication is of the eye. Symptoms of this unexpected complication have been described as blurring of vision and amaurosis (temporary blindness). In addition, anesthesia of motor neurons can result in mydriasis (pupillary dilation), ptosis (droopy eyelid), and diplopia (double vision). Horner-like manifestations involving ptosis, enophthalmos (recession of the eyeball within the orbit), and miosis (papillary restriction) have also been reported. Generally, symptoms develop immediately after injection of the anesthetic solution and last for several hours. These symptoms are attributed to the anesthetic solution reaching the orbit or cavernous sinus.
When these complications occur, they can be distressing to both the patient and the dentist. Although permanent damage to tissues, nerves, and eyes is rare, the practitioner should be able to detect and effectively treat the complication to avoid the development of permanent sequellae.
Clinical reports and implications
In 1962, Cooper presented one of the most cited ocular complication cases in the dental literature. The case describes a 46-year-old woman who was given a right mandibular block with 2% mepivacaine with vasoconstrictor. She immediately experienced transitory blindness followed by diplopia, which continued for 5 hours. The ophthalmologists who examined her 15 minutes after local anesthetic administration discovered a total paralysis of the right lateral rectus muscle. The patient was without ocular signs and symptoms when she was evaluated the following day.
Blaxter and Britten similarly reported several cases involving transient loss of vision, diplopia, and amaurosis. They postulated that an intra-arterial injection of the inferior alveolar artery occurred, with a retrograde flow pattern carrying the anesthetic to the area of the eye. In all of their reported cases, the patients recovered completely. Goldenberg reported a similar case following a mandibular injection, in which the patient developed dizziness, diplopia, and blanching of the ipsilateral upper eyelid. The proposed cause was traced to the lacrimal artery, which affected the innervation to the lateral rectus muscle. Dryden reported a case following a Gow-Gates injection, in which the patient complained of a burning sensation around the infraorbital region after the second injection. Diplopia of the right eye developed, as well as blanching of the skin coinciding with the infraorbital artery.
The most calamitous ocular outcome of a local anesthetic injection was reported in 1957 by Walsh. In his report, the patient experienced permanent blindness immediately after an intraoral injection of 2% procaine-adrenaline (1:50,000) solution. The patient stated a sensation of blue color for a moment followed by a reduced perception of light. Examination 4 days after the injection revealed areas of early retinal damage and lack of visual acuity.
A review of literature since 1957 revealed a total of 48 cases (including the new report presented later in the article) involving ophthalmic complications. Twenty-seven reports occurred after maxillary injection (posterior superior alveolar nerve block or middle superior alveolar field block) and 21 reports were related to mandibular injections (inferior alveolar nerve block). The symptoms associated with the maxillary and mandibular injections are listed in Table 1 . The demographic data overall were somewhat inconclusive; however, a predilection was observed with 72.9% of cases (n = 48) involving women.
| Symptom/Manifestation | Total Reports | Maxillary Injections | Mandibular Injections |
|---|---|---|---|
| Ophthalmoplegia (Paralysis of eye muscles) | 14 | 12 | 2 |
| Ptosis of the eyelid | 12 | 7 | 5 |
| Mydriasis | 9 | 6 | 3 |
| Amaurosis (Blindness/Loss of vision) | 9 | 3 | 6 |
| Diplopia | 7 | 3 | 4 |
| Diplopia by lateral rectus palsy | 8 | 3 | 5 |
| Diplopia by medial rectus palsy | 2 | 1 | 1 |
| Miosis | 3 | 3 | 0 |
| Dizziness | 6 | 2 | 4 |
| Blurred vision | 4 | 1 | 3 |
| Partial paresis | 1 | 1 | 0 |
| Blanching | 2 | 0 | 2 |
| Burning sensation | 1 | 0 | 1 |
| Horner syndrome | 1 | 0 | 1 |
| Nausea | 1 | 0 | 1 |
| Tearing | 1 | 0 | 1 |
| Totals | 81 | 42 | 39 |
a Based on 48 case reports (including the case report presented in the article). All manifestations were included, allowing for multiple symptom reports in an individual article.
As shown in Fig. 1 , the onset times of symptomatic response are not always reported. For the cases in which onset was documented, most symptoms were seen within the first 5 minutes following the injection. It should be noted that comparisons between onset times and location of injection revealed no statistically significant difference between maxillary or mandibular injection techniques.
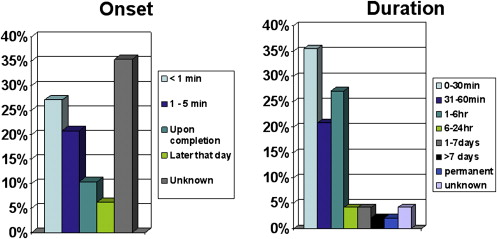
The duration of symptoms was examined for these reports from literature (see Fig. 1 ). Forty reports (83.3%) have described transient manifestations that disappeared within 6 hours of anesthetic administration. However, because of the usually benign and transient nature of the manifestations, most patients never received detailed examinations by an ophthalmologist and specifics of the ocular deficits are not well documented.
As shown in Table 1 , the most common symptom identified by the investigators of the 48 case reports was diplopia (17 manifestations), followed by muscle paralysis (14 manifestations), ptosis (12 manifestations), mydriasis (9 manifestations), and blindness or loss of vision (9 manifestations). In addition, most patients experience approximately 2 symptoms per manifestation. On evaluating these literature reports by injection location, 42 symptoms followed maxillary injections and 39 symptoms followed mandibular injections. Comparisons of symptoms revealed that ophthalmoplegia, mydriasis, and ptosis were more commonly seen with maxillary injections, whereas amaurosis, diplopia, and blurred vision were observed more frequently after mandibular injections.
The authors also completed an evaluation of the types of anesthetic used and their relation to ocular complications ( Table 2 ). A particular pattern was discovered as it relates to articaine and maxillary injections. It was noted that in 15 of the 27 (55.6%) case reports relating to ophthalmic complications with maxillary injections, 4% articaine with 1:100,000 epinephrine was used. Conversely, articaine was not involved with any of the mandibular injection complications. Given that the most commonly proposed cause of ocular manifestations with maxillary injections is diffusion, it could be proposed that the diffusion properties of articaine may be more extensive than those of the other local anesthetics evaluated. Given the increased use of articaine in North America in the last few years, this pattern may continue to be seen in the future.
| Type of Anesthetic | Total | Maxillary Injections | Mandibular Injections |
|---|---|---|---|
| 1% Lidocaine with Adrenaline | 1 | 1 | 0 |
| 2% Lidocaine with 1:80,000 Adrenaline | 6 | 2 | 4 |
| 2% Lidocaine Plain | 1 | 1 | 0 |
| 2% Lidocaine with 1:100,000 Epinephrine | 9 | 2 | 7 |
| 3% Mepivacaine Plain | 4 | 2 | 2 |
| 2% Mepivacaine with Vasoconstrictor | 2 | 0 | 2 |
| 4% Articaine with 1:100,000 Epinephrine | 15 | 15 | 0 |
| Procaine | 1 | 1 | 0 |
| Procaine with 1:300,000 Adrenaline | 3 | 0 | 3 |
| Butethamine hydrochloride with 1:100,000 Adrenaline | 1 | 0 | 1 |
| Unknown/Not Reported | 5 | 3 | 2 |
Etiology of ocular complications
There is currently no agreement to the exact cause of ocular complications seen following intraoral local anesthesia injections. However, it is generally agreed that (1) the local anesthetic solution reaches the area of the orbit through vascular, neurologic, myofascial, and/or lymphatic networks and (2) the cause is likely to be different for the injections administered in the maxilla or mandible.
Proposed Causes of Ocular Complication with Mandibular Nerve Block Injections
Arterial
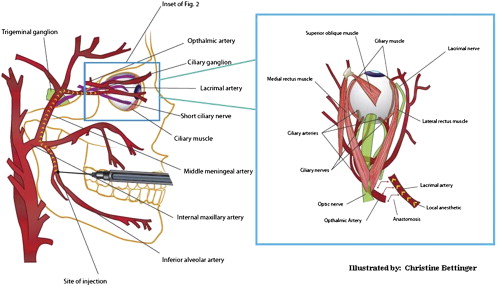
This theory is supported by the frequent symptoms of temporary dizziness, blanching of the skin, and anesthesia of the eyelids, which are supplied by the lacrimal nerve that depends on the lacrimal artery. The inferior alveolar artery runs posterior to the inferior alveolar nerve, and therefore, local anesthetic solution may accidentally be injected into the artery. Given that the solution is injected under pressure, the solution may be forced back into the maxillary artery (via retrograde flow) and gain access to the middle meningeal artery ( Fig. 2 ). The ophthalmic branch of the middle meningeal artery may anastomose with the lacrimal artery. The blood supply of the lateral rectus muscle derives from the lacrimal artery and from the lateral muscular trunk of the ophthalmic artery. Therefore, the intra-arterial injection of the local anesthetics may reach and paralyze the lateral rectus muscle and cause diplopia.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


