Introduction
Our aim in this study was to evaluate the effect of augmented corticotomy on the decompensation pattern of mandibular anterior teeth, alveolar bone, and surrounding periodontal tissues during presurgical orthodontic treatment.
Methods
Thirty skeletal Class III adult patients were divided into 2 groups according to the application of augmented corticotomy labial to the anterior mandibular roots: experimental group (with augmented corticotomy, n = 15) and control group (without augmented corticotomy, n = 15). Lateral cephalograms and cone-beam computed tomography images were taken before orthodontic treatment and before surgery. The measurements included the inclination and position of the mandibular incisors, labial alveolar bone area, vertical alveolar bone height, root length, and alveolar bone thickness at 3 levels surrounding the mandibular central incisors, lateral incisors, and canines.
Results
The mandibular incisors were significantly proclined in both groups ( P <0.001); however, the labial movement of the incisor tip was greater in the experimental group ( P <0.05). Significant vertical alveolar bone loss was observed only in the control group ( P <0.001). The middle and lower alveolar thicknesses and labial alveolar bone area increased in the experimental group. In the control group, the upper and middle alveolar thicknesses and labial alveolar bone area decreased significantly. There were no significant differences in dentoalveolar changes between the 3 kinds of anterior teeth in each group, except for root length in the experimental group ( P <0.05).
Conclusions
Augmented corticotomy provided a favorable decompensation pattern of the mandibular incisors, preserving the periodontal structures surrounding the mandibular anterior teeth for skeletal Class III patients.
Highlights
- •
Treatment effects of augmented corticotomy for skeletal Class III malocclusion are presented.
- •
Augmented corticotomy provided a favorable outcome after decompensation of the mandibular anterior teeth.
- •
The 6 mandibular anterior teeth were all evaluated using cone-beam computed tomography data.
- •
Significant vertical alveolar bone loss was observed only in the control group.
- •
Favorable responses were obtained on incisal thirds of the alveolus and alveolar crest without using a barrier membrane.
Presurgical orthodontic treatment is typically necessary to correct compensated tooth positions that result from undesirable jaw growth. Correcting the dental compensations allows the most favorable positioning of the jaw segments during surgery and permits a more accurate and stable occlusion after surgery. In the correction of Class III malocclusion, decompensation of the mandibular anterior teeth labially to an ideal relationship to the supporting bone will allow the best improvement of facial esthetics after surgery. However, labial incisor movement can be limited by the alveolar housing. A previous study has shown that excessive labial incisor movement is associated with dehiscence of the labial bone. The authors found a high correlation between the labiolingual inclination of the teeth and the frequency of dehiscence or gingival recession.
Recently, cone-beam computed tomography (CBCT) has been an indispensable diagnostic imaging tool for dentoalveolar evaluation. CBCT studies of skeletal Class III patients after orthodontics and orthognathic surgery have confirmed that mandibular incisors experience more vertical alveolar bone loss than do maxillary incisors, and the alveolar bone becomes thin at the root apex area. Particularly, labioversion of the mandibular anterior teeth induces decreases of alveolar bone and thickness of bone around the mandibular incisors.
Augmented corticotomy has been reported as a method to achieve sufficient labioversion of the mandibular anterior teeth while minimizing gingival recession and alveolar bone loss. Before orthodontic forces are applied, the clinician performs selective decortications around the target teeth and alveolar bone grafting with particulate bone grafting material. This technique has been used to achieve the regional acceleratory phenomenon, resulting in accelerated tooth movement, with the benefit of maintaining sound a periodontium at the end of orthodontic treatment.
In a preliminary study, we reported using this technique based on the lateral cephalometric analyses of 15 skeletal Class III patients who had orthognathic surgery after decompensation of the mandibular anterior teeth. The augmented corticotomy provided effective decompensation of the mandibular incisors in skeletal Class III patients while maintaining labial bone thickness and with few periodontal side effects. The pilot study had a small sample size, and the lateral cephalometric x-rays provided compromised evaluations of the dentoalveolar regions of individual teeth. Recent studies have reported on augmented corticotomy in the mandibular anterior regions with CBCT in Class III patients. Although the images are more accurate, the studies had small sample sizes and no control groups, and evaluated only incisors. Most studies have used the guided bone regeneration technique with collagen membranes. The mandibular canines are the high-risk sites of dehiscence; a comprehensive study of this problem should include the canines as well as the incisors.
The purpose of this study was to elucidate the effect of augmented corticotomy applied in skeletal Class III patients before presurgical orthodontic treatment to decompensate the mandibular anterior teeth, including the central incisors, lateral incisors, and canines.
Material and methods
The subjects in this retrospective study included 30 adult patients characterized by skeletal Class III malocclusion who had orthognathic surgery at the Department of Orthodontics at the Kyung Hee University Dental Hospital in Seoul, Korea ( Table I ). They were divided into 2 groups, matched for age, sex, and pretreatment mandibular central incisor position, according to the application of augmented corticotomy: experimental group (with augmented corticotomy; n = 15 [7 men, 8 women]; mean age, 23.06 ± 6.16 years) and control group (without augmented corticotomy; n = 15 [7 men, 8 women]; mean age, 21.51 ± 3.34 years). The augmented corticotomy was performed when the amount of labioversion of the mandibular incisors (IMPA changes) was planned to be more than 5°, and the labial alveolar bone thickness of the mandibular incisors was less than 1 mm. Five patients had 1-jaw surgery, and 10 patients had 2-jaw surgery in the experimental group; 3 patients had 1-jaw surgery, and 12 patients had 2-jaw surgery in the control group.
| Measurement | Experimental group (n = 15) | Control group (n = 15) | Total (n = 30) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| SNA (°) | 83.45 | 3.53 | 82.01 | 2.38 | 82.73 | 3.04 |
| SNB (°) | 86.56 | 4.50 | 85.99 | 2.66 | 86.27 | 3.65 |
| ANB (°) | −3.11 | 2.67 | −3.98 | 2.47 | −3.54 | 2.56 |
| SN-MP (°) | 32.95 | 8.72 | 32.76 | 4.68 | 32.85 | 6.88 |
| FMA (°) | 25.98 | 7.50 | 25.61 | 3.47 | 25.80 | 5.75 |
| Age (y) | 23.06 | 6.16 | 21.51 | 3.34 | 22.29 | 4.94 |
| Treatment duration (mo) | 8.73 | 2.46 | 10.87 | 2.45 | 9.80 | 2.65 |
The mean periods of presurgical orthodontic treatment were 8.7 months in the experimental group and 10.9 months in the control group, from the first medical examination to the orthognathic surgery. The study was performed with the approval of the institutional review board of Kyung Hee University Dental Hospital (KHU-IRB-1208-01). The inclusion criteria were bilateral skeletal and dental Class III relationships, without severe facial asymmetry (<5 mm of lower midline deviation from the facial midline), mild to moderate crowding in the mandibular arch (<5 mm), no missing or malformed teeth, and no recession of attached gingiva or alveolar bone loss on the mandibular anterior teeth.
All patients had orthodontic treatment with a 0.022-in Roth prescription appliance, fully bonded to the second molars. Augmented corticotomy, with patient consent, was performed after or right before the attachment of the brackets. Crevicular incision on the labial side of the gingiva from the mandibular left second premolar to the mandibular right second premolar preceded the full-thickness flaps. Vertical corticotomy was performed in the cortical plate between the teeth with a number 2 round bur or a piezoelectric surgical device. The range of vertical corticotomy was from 2 to 3 mm below the crest of the alveolar bone to 2 to 3 mm below the apex. Then, a horizontal corticotomy was performed 2 to 3 mm below the apices. The horizontal corticotomy line was connected to the vertical corticotomy lines, completing a circumscribed corticotomy ( Fig 1 , A ).
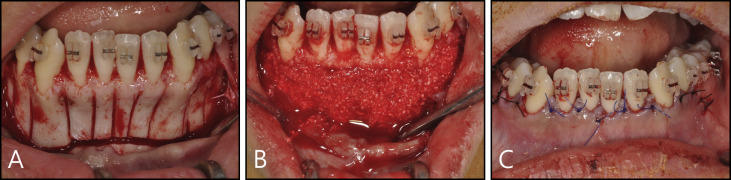
When bleeding was sufficient after the corticotomy, bone augmentation was done between the labial alveolar bone and the gingival flap using mineralized and deproteinized bovine bone mineral (Bio-Oss; Geistlich Pharma, Wolhusen, Switzerland) ( Fig 1 , B ). After the interdental papillae and flap were repositioned, vertical everting mattress sutures were placed with 5-0 or 6-0 nylon ( Fig 1 , C ). The sutures were removed a week after surgery. A 0.016 × 0.022-in rectangular nickel-titanium wire was engaged to begin decompensation on the same day. The process of treatment was explained in detail in our previous article.
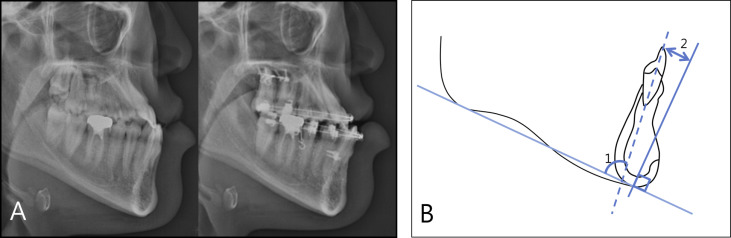
To analyze the lateral cephalometric x-ray, 2 lateral cephalograms, taken before orthodontic treatment and before surgery (completion of preoperative orthodontic treatment), were measured with the PiView STAR program (Infinit Technology, Seoul, Korea). To evaluate the variations of inclination of the mandibular anterior teeth and the amount of decompensation of the mandibular incisors, the rater (D-H.S.) set the baselines and points, and measured IMPA and the shortest distance between the crown tip of the mandibular central incisor and the perpendicular line to the mandibular plane, drawn from menton (menton vert-L1) ( Fig 2 ).
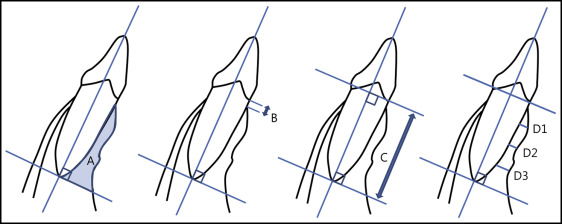
Two CBCT images, taken before orthodontic treatment and before surgery (completion of preoperative orthodontic treatment), were analyzed with the InVivo Dental program (Anatomage, San Jose, Calif). These scans were taken with a CBCT device (Alphard-3030; Asahi Roentgen, Kyoto, Japan) with dosimetry parameters of 10 mA, 80 kV, and 17-second scan time. I mode (0.15 mm 3 voxel size) with a field of view that included the anterior dentition and the body of mandible was used. The CBCT raw data of both groups were gathered without any marks, randomly mixed, and sequentially numbered before evaluation. When the second evaluation was performed after 2 weeks, the data were randomly mixed again and assigned new numbers. The rater set the baselines and points, and measured the labial alveolar bone area (LABA), vertical alveolar bone level, root length, and upper, middle, and lower alveolar bone thicknesses on the labial side ( Fig 3 ).
Statistical analysis
All measurements were repeated by the same operator (S-H.K.) after 2 weeks. The 6 mandibular anterior teeth were divided into 2 groups. The CBCT measurements of the mandibular left teeth were assigned numbers from 1 to 15, and the right teeth were assigned numbers from 16 to 30. Since there were no differences in the values of all variables between the right and left sides, the data were combined to develop the statistical analysis. The mean of the 2 measurements was used for this study. The differences ranged from 0.26 to 0.34 mm for linear measurements, from 0.24° to 0.45° for angular measurements, and from 0.32 to 0.46 mm 2 for area measurements, according to Dahlberg’s formula. The independent t test was performed for the comparisons between the 2 groups, the paired t test was used for the comparisons between baseline and after decompensation in each group, and 1-way analysis of variance with the Duncan multiple comparison test was used for the comparisons between the central incisors, lateral incisors, and canines. The P <0.05 level of significance was chosen for all tests.
Results
We looked at the decompensation pattern of the mandibular incisors using lateral cephalograms ( Table II ). The changes of IMPA were statistically significant in both the experimental and control groups ( P <0.001). The average changes of IMPA were 7.51° (from 78.55° to 86.05°) in the experimental group and 5.31° (from 78.57° to 83.87°) in the control group. The variation of menton vert-L1 was also statistically significant in the groups (both, P <0.001). The average change of menton vert-L1 was 2.35 mm in the experimental group, which was almost double compared with the change in the control group (1.14 mm). When comparing the 2 groups, only the labial movement of the incisor crown tip (menton vert-L1) showed a significant difference ( P <0.05).
| Experimental group (n = 15) | Control group (n = 15) | Comparison between groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | P value ∗ | Before | After | P value ∗ | ||||||
| Mean | SD (IQR) | Mean | SD (IQR) | Mean | SD (IQR) | Mean | SD (IQR) | P value † | |||
| IMPA (°) | 78.55 | 4.25 (6.00) | 7.51 | 5.68 (9.90) | 0.0002 § | 78.57 | 6.12 (8.00) | 5.31 | 3.67 (8.10) | 0.0001 ‡ | 0.2184 |
| Menton vert-L1 (mm) | −9.77 | 2.95 (4.50) | 2.35 | 1.63 (1.98) | 0.0001 § | −9.77 | 4.17 (4.60) | 1.14 | 0.76 (1.50) | 0.0000 ‡ | 0.0145 ‡ |
Dentoalveolar changes surrounding the mandibular anterior teeth were seen in the CBCT images ( Figs 4 and 5 ). For the mandibular canines, there was a statistically significant vertical alveolar bone loss (CEJ-crest) in the control group ( P <0.001; Table III ). There was a slight vertical alveolar bone gain in the experimental group, although it was not statistically significant. After decompensation, the upper and middle alveolar thicknesses in the control group decreased with statistical significance ( P <0.001). The upper alveolar thickness in the experimental group also decreased ( P <0.05), whereas the middle and lower alveolar thicknesses increased (lower thickness, P <0.001). Labial alveolar bone area decreased in the control group and increased in the experimental group (both, P <0.001). Root length in both groups decreased with statistical significance ( P <0.001). When we compared the measurement changes between groups, all measurements showed significant differences except for root length and upper alveolar thickness (LABA; CEJ-crest, middle and lower alveolar thicknesses; all P <0.001).
| Experimental group (n = 15) | Control group (n = 15) | Comparison between groups | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | P value ∗ | T0 | T1 | P value ∗ | At T0 | T1-T0 | |||||
| Mean | SD (IQR) | Mean | SD (IQR) | Mean | SD (IQR) | Mean | SD (IQR) | P value † | P value † | |||
| Central incisors | ||||||||||||
| LABA (mm 2 ) | 3.77 | 1.84 (2.19) | 6.61 | 5.72 (6.12) | 0.0068 § | 5.23 | 2.22 (3.17) | 2.94 | 2.84 (4.45) | 0.0003 ‖ | 0.0074 § | 0.0000 ‖ |
| CEJ-crest (mm) | 4.88 | 3.75 (6.83) | 4.26 | 2.85 (4.80) | 0.4042 | 2.05 | 1.71 (0.97) | 5.63 | 3.41 (6.87) | 0.0000 ‖ | 0.0011 § | 0.0000 ‖ |
| Root length (mm) | 10.86 | 1.07 (1.79) | 10.27 | 1.08 (1.35) | 0.0000 ‖ | 11.11 | 0.74 (1.08) | 10.41 | 0.68 (1.22) | 0.0000 ‖ | 0.4289 | 0.4535 |
| Upper bone thickness (mm) | 0.51 | 0.29 (0.32) | 0.45 | 0.33 (0.64) | 0.2477 | 0.71 | 0.29 (0.41) | 0.26 | 0.35 (0.55) | 0.0000 ‖ | 0.0133 ‡ | 0.0000 ‖ |
| Middle bone thickness (mm) | 0.31 | 0.20 (0.19) | 0.67 | 0.41 (0.66) | 0.0001 ‖ | 0.48 | 0.18 (0.17) | 0.26 | 0.36 (0.49) | 0.0002 ‖ | 0.0001 ‖ | 0.0000 ‖ |
| Lower bone thickness (mm) | 0.31 | 0.27 (0.38) | 1.46 | 1.18 (1.38) | 0.0000 ‖ | 0.46 | 0.23 (0.18) | 0.46 | 0.63 (0.65) | 0.9771 | 0.0070 § | 0.0000 ‖ |
| Lateral incisors | ||||||||||||
| LABA | 5.13 | 2.67 (3.79) | 10.11 | 7.73 (10.53) | 0.0020 § | 6.47 | 2.75 (3.80) | 4.04 | 3.44 (4.84) | 0.0003 ‖ | 0.0617 | 0.0000 ‖ |
| CEJ-crest | 4.46 | 4.07 (7.77) | 4.25 | 2.80 (4.69) | 0.3474 | 1.79 | 0.92 (1.51) | 6.03 | 3.52 (7.28) | 0.0000 ‖ | 0.0071 § | 0.0000 ‖ |
| Root length | 11.96 | 1.26 (1.63) | 11.16 | 1.14 (1.86) | 0.0000 ‖ | 12.50 | 1.21 (0.93) | 11.77 | 1.05 (1.47) | 0.0000 ‖ | 0.1624 | 0.4535 |
| Upper bone thickness | 0.64 | 0.31 (0.41) | 0.58 | 0.51 (0.91) | 0.5395 | 0.72 | 0.40 (0.37) | 0.31 | 0.43 (0.65) | 0.0000 ‖ | 0.3911 | 0.0000 ‖ |
| Middle bone thickness | 0.33 | 0.14 (0.15) | 0.85 | 0.64 (0.85) | 0.0001 ‖ | 0.43 | 0.17 (0.16) | 0.22 | 0.36 (0.36) | 0.0002 ‖ | 0.0065 § | 0.0000 ‖ |
| Lower bone thickness | 0.40 | 0.46 (0.41) | 1.99 | 1.15 (1.53) | 0.0000 ‖ | 0.48 | 0.28 (0.29) | 0.56 | 0.84 (0.85) | 0.9771 | 0.0158 ‡ | 0.0000 ‖ |
| Canines | ||||||||||||
| LABA | 6.86 | 4.41 (5.17) | 11.37 | 7.04 (9.75) | 0.0004 ‖ | 9.20 | 5.83 (6.17) | 7.09 | 5.60 (8.21) | 0.0657 | 0.0385 ‡ | 0.0001 ‖ |
| CEJ-crest | 7.43 | 4.44 (9.15) | 6.58 | 3.04 (4.49) | 0.3420 | 4.37 | 4.28 (7.83) | 8.63 | 3.60 (4.85) | 0.0000 ‖ | 0.0156 ‡ | 0.0001 ‖ |
| Root length | 13.56 | 1.81 (3.10) | 13.14 | 1.68 (2.65) | 0.0000 ‖ | 14.40 | 1.25 (1.70) | 13.81 | 1.37 (2.24) | 0.0000 ‖ | 0.0415 ‡ | 0.2213 |
| Upper bone thickness | 0.51 | 0.39 (0.68) | 0.28 | 0.35 (0.59) | 0.0340 ‡ | 0.60 | 0.33 (0.30) | 0.15 | 0.31 (0.00) | 0.0000 ‖ | 0.5045 | 0.0785 |
| Middle bone thickness | 0.25 | 0.25 (0.41) | 0.44 | 0.54 (0.91) | 0.1112 | 0.38 | 0.24 (0.30) | 0.10 | 0.23 (0.00) | 0.0000 ‖ | 0.0163 ‡ | 0.0006 ‖ |
| Lower bone thickness | 0.53 | 0.58 (0.90) | 1.79 | 1.12 (1.68) | 0.0000 ‖ | 0.73 | 0.71 (0.70) | 0.93 | 1.11 (1.68) | 0.2893 | 0.1357 | 0.0005 ‖ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


