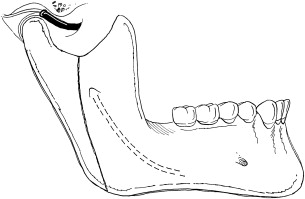
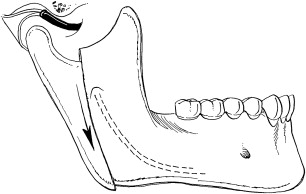
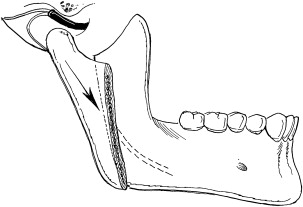
The modified condylotomy is an extra-articular surgical procedure used to manage patients with temporomandibular joint dysfunction. The primary purpose of the procedure is to increase joint space by allowing the mandibular condyle to move inferiorly with respect to both the articular disc and eminence ( Figs 1 and 2 ). An additional goal in some patients is to establish a more normal condyle/disc relationship, particularly for Wilkes I, II, and III (early) internal derangements. This disc relationship can be achieved in many patients by allowing the condyle to move anteriorly in addition to inferiorly ( Fig. 3 ).
Condylotomy may be considered in patients with intra-articular pain or locking in association with internal derangement. The procedure has also been advocated for recurrent temporomandibular joint dislocation. The main advantages of the procedure over arthroplasty are the extra-articular approach that avoids entry into the temporomandibular joint, the short duration of the procedure, and the ability to complete the surgery in an ambulatory setting. Disadvantages of the technique include the inability to address additional sources of intra-articular pain and locking, such as synovitis, fibrous adhesions, pseudowalls, osteoarthritis, chondromalacia, and synovial chondromatosis. Furthermore, patients require arch-bars and a period of elastic maxillomandibular fixation lasting 10 days to 6 weeks. A change in the occlusion following this procedure is common, although spontaneous tooth movement over time compensates adequately for the malocclusion in many patients. However, a small number of patients will need occlusal equilibration, orthodontics, or additional surgery to correct the malocclusion. The use of modified condylotomy in patients with an existing anterior open bite or a class II malocclusion is not recommended because of the potential for worsening of the anterior open bite or class II dental relationship.
Technique
The basic set of instruments required to perform a modified condylotomy includes wire twisters and wire cutters for arch-bar application; electrocautery for incision and hemostasis; a Molt periosteal elevator (No. 9) and Freer periosteal elevator for the lateral ramus and posterior border, respectively; a J-stripper for the lower border; a Woodson periosteal elevator to identify the sigmoid notch; a dental mirror to visualize the osteotomy site; a small curved osteotome and mallet to complete the osteotomy; Yankauer and Frazier suckers; a Molt mouth prop; needle holders; and a pair of Debakey forceps. The most critical instruments are Bauer retractors, Obwegeser retractors including a notched retractor, and an angled oscillating saw with a 7-mm blade. A thick ramus may occasionally necessitate a longer blade. An additional blade should be available for bilateral cases.
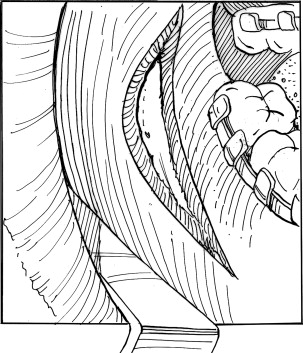
With the patient under general anesthesia, arch-bars are initially adapted to the maxilla and mandible from first molar to first molar using 25-gauge or 26-gauge wire. Bupivacaine 0.5% with 1:200,000 epinephrine is then injected into the soft tissues overlying the anterior aspect of the mandibular ramus. The Molt mouth prop is then inserted on the contralateral side and activated. A 5-cm incision is made through the mucosa overlying the external oblique ridge and extended superiorly along the anterior border of the ramus of the mandible for approximately 1 cm ( Fig. 4 ). The distal aspect of the incision proceeds through mucosa, submucosa, buccinator, and periosteum. The proximal 1 cm of the incision is through mucosa only to protect the long buccal nerve. A notched Obwegeser retractor is then used to expose the anterior ramus and dissect the inferior aspect of the temporalis tendon from the coronoid process ( Fig. 5 ). The use of Colorado tip electrocautery during this process greatly facilitates hemostasis and temporalis muscle dissection. A Molt periosteal elevator (No. 9) is then used to develop a subperiosteal plane over the lateral ramus extending to the posterior and inferior borders. It is helpful to gently strip periosteum from the posterior and inferior border using a curved Freer elevator and J-stripper, respectively. The sigmoid notch should be identified with the use of a Woodson periosteal elevator. Bauer retractors should be placed easily in the sigmoid notch and at the lower border if adequate periosteal stripping has been performed. The antilingula and the posterior border should be easily visualized. Difficulty visualizing these areas requires further periosteal stripping.