Manual Functional Analysis
Manual examination techniques for systematic testing of the musculoskeletal system can be traced back to the London orthopedist Cyriax. His 1933 textbook describes specific techniques for examining the temporomandibular joint. During recent decades, conventional functional diagnostics in dentistry was based primarily upon the study of active movements and muscle palpation (Dworkin et al. 1988, Fuhr and Reiber 1989, Siebert 1996). The system used was derived mostly from the examination techniques of Krogh-Poulsen (1966). Hansson et al. (1980, 1987) were the first to advocate applying the examination methods from orthopedics and manipulative therapy (Cyriax 1947; Mennell 1949; Maitland 1964; Wolff 1970; Mennell 1970, 1978; Kaltenborn 1976L; Cyriax 1947, 1979; Frisch 1987) to examination of the temporomandibular joint.
Over the years many other authors adopted various orthopedic tests and described their diagnostic potential (Friedman and Weisberg 1982, 1984; Palla 1986; Solberg 1986; McCarroll et al. 1987; Roller 1989; Hesse et al. 1990; Steenks and de Wijer 1991; De Laat et al. 1993; Lobbezoo-Scholte et al. 1993, 1994; Hesse 1996; Hesse et al. 1996, 1997).
By itself, however, the application of the “new” examination techniques to complement the conventional evaluation of active movements and muscle palpations still did not represent a decisive advance in clinical functional diagnostics.
The multitude of examination techniques available were taken up in 1988 by G. Groot Landeweer and A. Bumann and further developed into a systematic, practice-oriented examination concept. The term manual functional analysis was introduced to describe the new concept (Groot Landeweer and Bumann 1991, Bumann et al. 1993, Bumann and Schwarzer 1995, Bumann and Groot Landeweer 1996a, b) and to differentiate it from instrumented functional diagnostics, which was highly rated at that time, and from the term clinical functional analysis, which was used for the conventional procedures.
After a few years of intensive clinical experience, the initial concept (Groot Landeweer and Bumann 1992, Bumann and Groot Landeweer 1992) of the basic examination and the expanded examination-associated with the spiritual father of manipulative medicine-was abandoned in favor of a systematic, goal-oriented testing of the individual anatomical structures (joint surfaces, bilaminar zone, capsule and ligaments, muscles of mastication), in addition, specific techniques for differentiating various clicking phenomena in the human temporomandibular joint were described (Bumann and Groot Landeweer 1993), and the reliability of these for diagnosing partial and total disk displacements was demonstrated (Bumann and Zaboulas 1996).
The introduction of the so-called loading vector represents a major advance in manual functional analysis. This describes the direction of any load that is responsible for an area of tissue damage within the joint and provides a better understanding of malfunctions of the system. A determination of the specific loading vector is important if one is to follow an effective procedure for arriving at a diagnosis and treatment plan. Therefore the current concept of manual functional analysis takes the following aspects into consideration:
• A search for the loading vector at any given time
• Tests for any possible restrictions to movement
• Determination of various harmful influences
The Masticatory System as a Biological System
The introduction contains a brief discussion on how influences, mechanisms of adaptation and compensation, and the emergence of symptoms are interrelated. Whether or not symptoms will arise in the masticatory system depends primarily on the equilibrium between the harmful influences and the patient’s capacity for adaptation. The resultant influence is a combination of the number, duration, amplitude, and frequency of all the individual influences (static and dynamic occlusion, parafunctions, and dysfunctions). The dentist can alter this equilibrium only to a very limited extent. Because the patient’s individual adaptability cannot be influenced directly, one who treats a biological system such as the masticatory system can only indirectly help the organism to adapt by reducing the sum total of the harmful influences. For the dentist, this means that he/she can bring about a positive influence on a disrupted functional system only if the functional disturbance is at least partially the result of a nonphysiological static and/or dynamic occlusion.
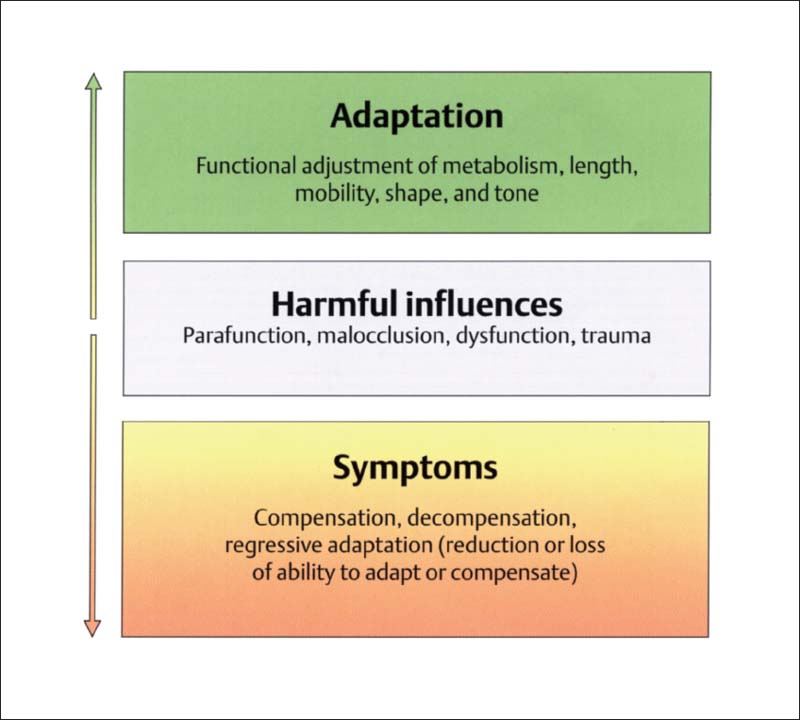
135 Biological systems
Influences within biological systems are processed through two mechanisms. When a system has the ability to assimilate the acting stimulus passively without a further increase of its inherent energy, an adaptive condition exists. The second mechanism is compensation, in which there is an increase of the system’s inherent energy with either an absence or a decrease in adaptation. With persisting un-physioiogical loading the system can lose its ability to compensate (decompensation) and undergoes collapse, usually with the appearance of clinical symptoms. It is essential during examination of the masticatory system that the clinician is able to differentiate between these two conditions, adaptation on the one hand and and loss of adaptation or loss of compensation on the other. Systems that are in an adaptive state require no treatment. When adaptation becomes lost, treatment is necessary; the treatment goal is the restoration of an adapted condition.
The first part of the manual functional analysis procedure determines the patient’s complaints and the degree of damage of the relevant tissue. The principle of the examination is similar to that of a stress EKG: the structures of the masticatory system are loaded to the maximum in a specified sequence. A patient may react to this in one of three ways:
• The stress on the tissue provokes no pain or other symptoms. This is a physiological response and is a sign that the structures are either unaltered or optimally adapted.
• In the second type of response, symptoms are brought forth only during application of the stress and are therefore not experienced during the patient’s normal activities. This condition is referred to as a compensated functional disturbance.
• The third possibility is the reproducible provocation of the same symptoms that brought the patient to the clinician and which were reported in the patient history. This indicates the presence of a decompensated or regressively adapted functional disturbance. It is caused either by overloading of a muscle (decompensation), traumatic tissue damage, or, most commonly, by inflammatory tissue destruction (regressive adaptation).
Specific and Nonspecific Loading Vectors
As soon as clinically reproducible symptoms are provoked by manipulation, the examiner knows that a functional disturbance is present that may be either compensated, decompensated, or regressively adapted. In any biological system, functional symptoms are caused by chronic non-physiological loading. Therefore, for the sake of treatment, it is important for the therapist to know the direction of the overloading. A nonphysiological load of a certain amount in a certain direction is called a loading vector. This may be specific or nonspecific.
A specific loading vector is present if symptoms appear only in one main direction during the tissue-specific examination. If, however, symptoms can be provoked in various directions, or even to some extent in opposite directions, then one is dealing with a nonspecific loading vector. In this case the second part of manual functional analysis, the specific clarification of the influences, would be nonproductive and should not be continued because of the ubiquitous manifestations of inflammation.
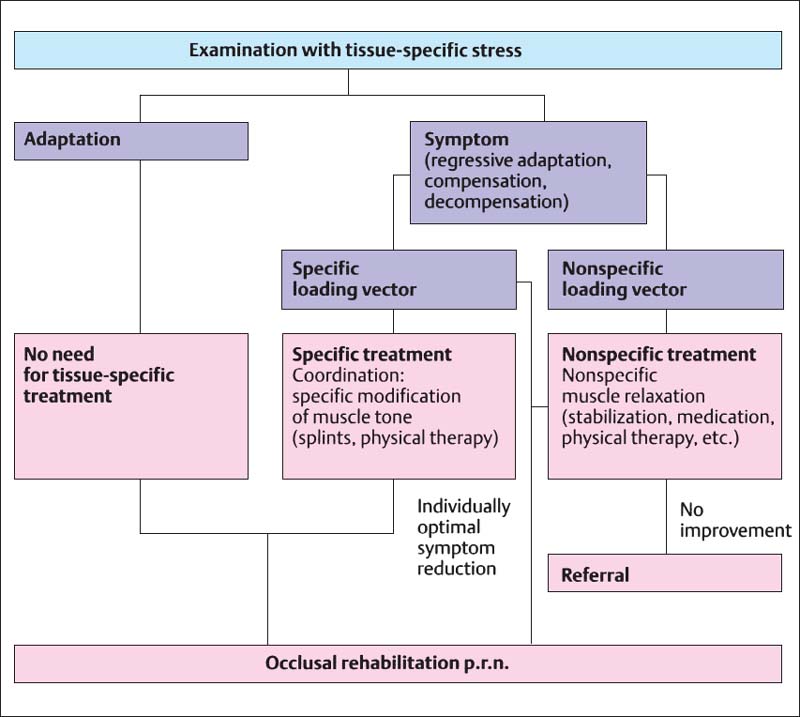
136 Treatment paths
Diagram of treatment paths based upon the findings arrived at through manual functional analysis. The musculoskeletal parts of the masticatory system are investigated by manipulative testing methods in which tissue-specific stress is applied to the structures being examined. This differentiates between adaptive and nonadaptive conditions. The latter (regressive adaptation, compensation, and decompensation) are then identified by the patient’s response to the mechanical loading. In this way an injured structure can be located by means of tissue-specific stress in either a single (specific) or in multiple (nonspecific) loading directions. Injuries with a nonspecific loading vector call for general, nonspecific muscle relaxation, while those with one specific loading vector require targeted neuromuscular deprogramming followed by occlusal reconstruction.
A patient with a nonspecific loading vector is first given only primary, nonspecific pain treatment by stabilizing the system with the aid of an occlusal splint fabricated at the least painful mandibular position, as determined by the patient. In some cases this is supplemented with analgesic and/or anti-inflammatory medication, and/or physical therapy. During this phase, physiotherapeutic measures can be effective only if there are joint-relaxing vectors present that are not painful. As a rule, this is not the case when nonspecific loading vectors are present. It is hoped that during the primary pain treatment phase the nonspecific loading vector will be converted into a specific loading vector or, better yet, completely eliminated.
With identification of a specific loading vector, “clarification of the influences” (static and dynamic occlusion, parafunction, dysfunction, trauma) is completed. Cause-directed occlusal treatment is possible only if static or dynamic occlusal influences can be demonstrated. This type of treatment almost always begins with an occlusal splint to eliminate the occlusion-related part of the overall loading vector. Depending upon the number of influences present, this measure may allow the previously damaged structures to become completely adapted or be transformed into a compensated status. If success cannot be attained, the patient should be referred to a specialist.
Examination Form for Manual Functional Analysis
In the past, only information that had very limited relevance to treatment could be derived from the tests of active movements then used and the palpation of the muscles of mastication.
An examination procedure that goes back to Cyriax (1947, 1979), Kaltenborn (1974), Maitland (1964, 1967), and Mennell (1970) was First recommended for use in dentistry by Hansson et al. (1980). At the end of the 1980s with the perspective gained through more than 10 years of application, this procedure was modified, systematically expanded, and optimized with a view to increasing its clinical relevance.
The front side of the examination form we use contains, in addititon to the patient’s clerical information and history, an overview of the current tissue-specific primary diagnosis (e.g. regressively adapted or decompensated functional disturbances) and secondary diagnosis (compensated functional disturbances) as well as their loading vectors and the individual harmful influences. This differentiation is important for treatment planning as well as for establishing the treatment goal for the patient. Furthermore it gives an overview of diagnostic procedures and specific musculoskeletal impediments in the direction of treatment.
Form for recording findings of manual functional analysis While the front of the examination form summarizes the diagnostic and therapeutic information, the reverse side is reserved for only the individual findings of the tissue-specific examination.
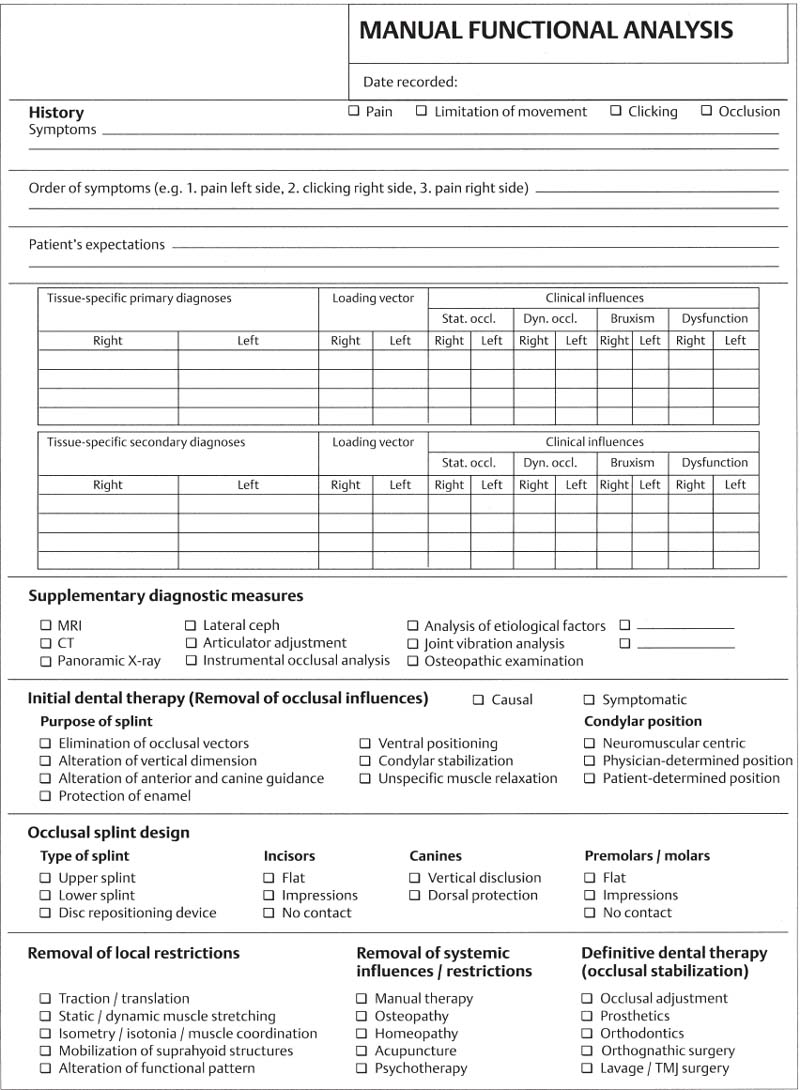
137 Front side of form
This side provides an overview of the tissue-specific primary and secondary diagnoses, etiological factors (influences), further diagnostic measures, and treatment planning.
The reverse side of the examination form serves to document tissue damage. After a brief intraoral and extraoral inspection, the active movements are recorded here and in some cases these are complemented by passive movements. Next the individual structures of the masticatory system are systematically tested in the following sequence:
• First, dynamic compressions and dynamic translations with compression are applied to test the joint surfaces.
• This is followed by testing of the bilaminar zone by means of passive compressions.
• Translations and traction allow specific loading of the joint capsule and ligaments.
• Functional testing of the muscles of mastication is accomplished through isometric contractions rather than by palpation.
• Joint play techniques and isometric contractions are used to help distinguish between arthrogenic and myogenic problems.
• Finally, dynamic tests are used to differentiate clicking sounds in the joints.
138 Reverse side of form
This side has spaces for all the information necessary for the tissue-specific examination of the extra-oral portions of the masticatory system. Entering the individual findings with a defined color-coding system allows a quick and convenient overview of which structures are adapted and which are not, as well as the corresponding loading vectors.
Patient History
The patient history is the foundation and a prerequisite for the diagnosis and treatment of functional disturbances. Together with the examination findings, it is used primarily in attempting to identify all regions of the masticatory system that have undergone structural damage (Okeson 1998). It serves further to help recognize the necessity for additional therapeutic measures and should protect both the patient and the clinician from failure (Nilges 1996). The history should be taken with the patient sitting upright in a quiet, relaxed atmosphere, ideally away from the treatment room.
As a rule, the general history can be adequately elicited by using a questionnaire. Eye contact and a friendly, interested demeanor on the part of the clinician promotes body language that will enhance nonverbal communication. If the patient’s descriptions become too long-winded, the clinician should politely interrupt and guide the discussion back to the relevant main questions of the specific history and the most prominent current symptoms. By repeating and summarizing the patients comments, the interviewer can help avoid misunderstandings.
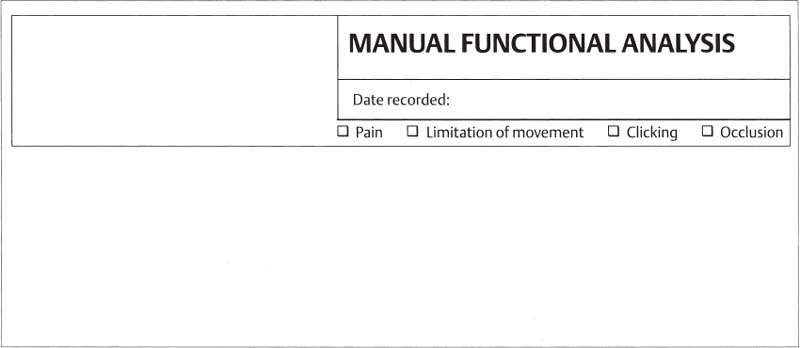
139 General patient data
To the left of the examination form heading is a box for the imprint data from the patient’s insurance card. To the right, under the recording date, the patient is to check one or more of the main symptom groups.
The procedure followed for the specific history is based upon the assumption that the dentist is able to recognize symptoms in his/her area of specialty and reproduce them at will. In the introduction we identified two major divisions of the diagnostic phase:
• “What does the patient have?” or “Is a loading vector pre sent?” and
• “Why does the patient have this loading vector?” or “Are corresponding occlusal influences present?”.
Without evidence of a loading vector or, to put it another way, without the ability to repeatedly demonstrate a lesion that causes local or projected pain, there is no rationale for dental treatment, contrary to what was often previously assumed. Therefore all questions related to the “why?”, that is, concerned with influences, should at first be strictly avoided in taking the specific history. Background inquiries into possible causes and previous therapeutic considerations (e.g. descriptions of the psychosocial environment, psychological questionnaires, detailed descriptions of previous treatments, etc.) are usually very time-consuming. Therefore a structured, symptom-related, tissue-specific examination is preferred. If the reported symptoms cannot be reproduced by this, then the patient must be referred for evaluation of systems in other fields such as orthopedics, neurology, psychology, or otolaryngology. If, on the other hand, the symptoms can be provoked, a search for possible causes and influences is conducted. A basic rule following from this is to concentrate ones efforts on those patients for whom dental procedures seem reasonable as a primary or supplemental treatment.
For this targeted, clinically appropriate interview process, three main questions have proven useful over the past few years:
“What are the Complaints that Brought You to Me?”
A meaningful entry in the specific history is an exact description by the patient of the presenting symptoms. Here the patient will usually report symptoms such as pain, restricted movement, clicking sounds in the joints, tinnitus, vertigo, burning tongue, lump in the throat, or a nonspecific sensation of pressure and tension. If the patient exhibits only one symptom, the course of the specific history will usually be relatively simple.
Whenever a pain symptom is reported, special attention must be given to its location, characteristics, initial occurrence, and the factors that increase its severity. The more vaguely a patient localizes the pain, the more specific the examiner’s inquiry must be and the more strongly he must encourage the patient in his or her account. Pain that is described as localized and sharp, unlike dull, widespread pain, is quite unreliable for differentiating between arthirogenic and myogenic disturbances. Nevertheless, the precise localization of pain, and especially an account of whether a larger area of pain is provoked by one or more localized pains, is of great importance for the later progress of the examination.
If an area of pain extends from the angle of the jaw to the temporal region, the examiner must clarify:
• whether the problems all come from one point and spread out over the entire affected region or
• whether one part of the pain comes, for example, from a point in front of the ear and radiates into the temporal region while another part is caused by a “different” pain directly in the region of the angle of the jaw. In this case the clinician is dealing with two separate pains that just happen to be close together.
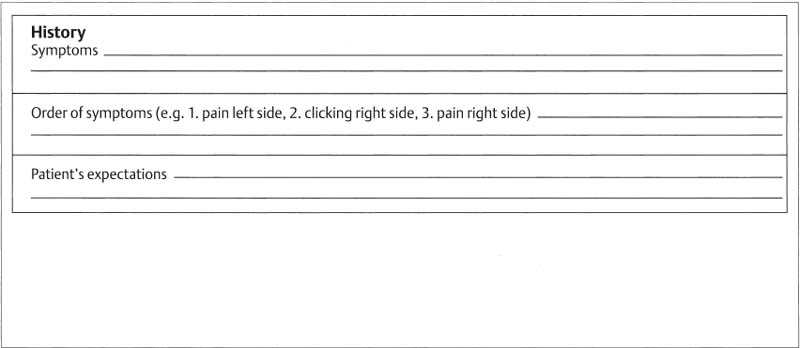
140 Special history
This section of the questionnaire is especially for patients with functional disturbances. It is essential that each patient answers the questions to his symptoms and his expectations. They can be supplemented as needed for individual cases. The answers to these questions will determine the precise course of the examination as well as the type and extent of therapeutic measures to be introduced.
This distinction has definite consequences for the examination procedure that will follow as well as for the treatment. If one wishes to completely eliminate the patient’s symptoms when the pains are separate, one must be able to elicit two pains that differ in their quality and location during the tissue-specific loading of the individual structures. If, for example, only one of the multiple pains reported in the patient history can be provoked, it will probably not be possible to rid the patient completely of all symptoms through dental treatment alone.
Therefore the fundamental rule is that if a symptom reported in the patient’s history is to be eliminated through dental treatment then one must be able to repeatedly reproduce it during the course of the tissue-specific examination. An analogous practice is followed in the diagnosis of pulpitis: If the pain described by the patient cannot be reproducibly provoked and no lesion (such as caries) can be detected, one would not normally proceed with endodontic treatment.
After the patient has described his or her complaints more accurately the dentist summarizes the information once more and concludes by inquiring about other symptoms. For example: “If I understand you correctly, you have pain on the right side in front of the ear and at the angle of the jaw. Beyond that you have no other problems. There is no clicking in the joints, and you can always open your mouth as far as it is supposed to go. Is that correct?”
“Rank Your Problems in Order of Severity”
When multiple symptoms are reported the patient is asked to rank them according to their impact on his/her well-being (primary symptom, secondary symptoms).
“What Exactly Do You Expect from Me?”
At the end of the history taking there is the question of the expectations the patient had in corning to the dentist. One patient might seek only an explanation of a troublesome symptom but no further treatment, another may expect thorough diagnostic procedures and complete treatment, while a third may want only relief of the primary symptom.
The patient’s expectations will have a substantial influence on the course of the examination and the treatment plan.
Taken together these three main questions of the specific history serve as a framework on which to organize the case presentation that will be given following the tissue-specific examination with manual functional analysis. This ensures that patients receive relevant information about the symptoms afflicting them and the answers to their questions.
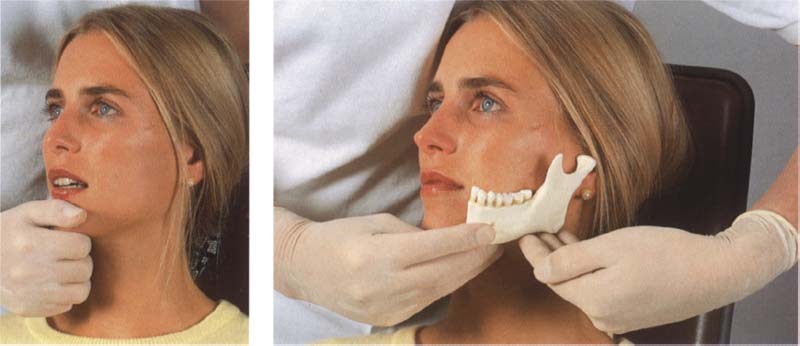
Positioning the Patient
The position of the patient is an important condition for a specific examination and is different for each section of the examination:
• History taking is always carried out with the patient sitting upright.
• The examination procedures for manual functional analysis are performed from the 12 o’clock position, or more precisely, between the 11 and 1 o’clock positions. Three arrangements are possible, the choice depending upon the examiner, the patient, and the space available. These are:
a) The patient is semi-reclined with the backrest at about a 45° angle and the examiner is standing upright behind the patient.
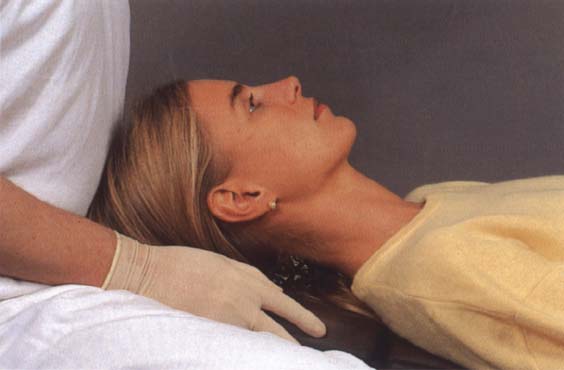
b) The patient is supine and the examiner is standing upright.
c) The patient is supine and the examiner is seated (the most effective variation).
• Testing for harmful influences can be carried out with the patient either fully reclined or sitting upright.
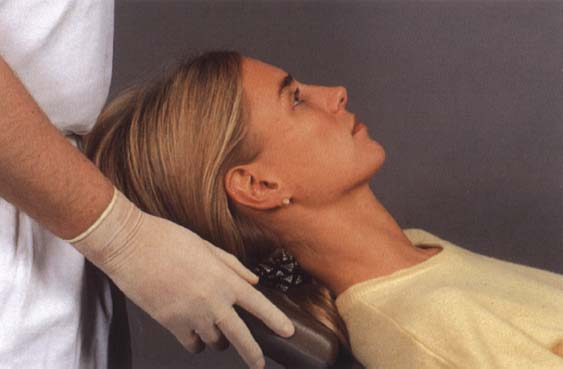
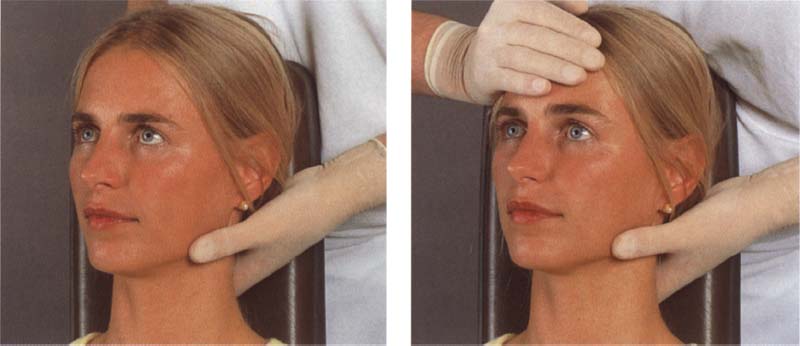
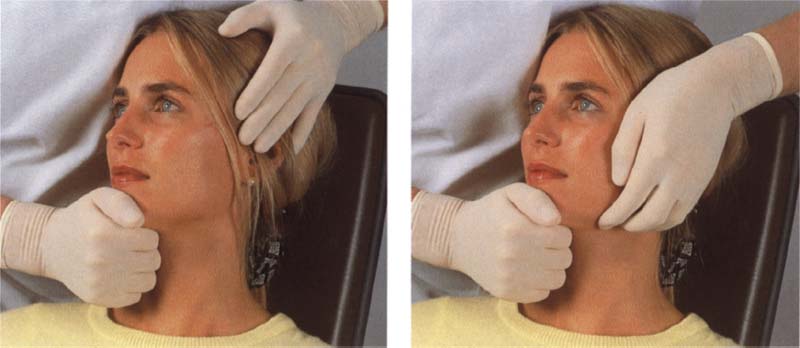
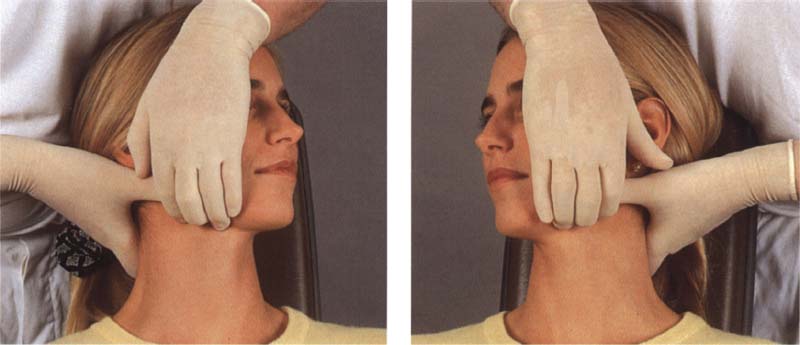
141 Examiner standing and patient semireclined
This arrangement is equally comfortable for both the clinician and the patient. It is normally chosen if for any reason the examiner prefers to work standing up or if the patient cannot recline fully because of a general orthopedic problem.

142 Examiner standing and patient fully reclined
This horizontal positioning of the patient with the examiner standing is appropriate only if the clinician is of short stature. Otherwise it would be difficult to stabilize the patient’s head. Furthermore, a dental chair cannot normally be raised high enough for a taller clinician to examine the patient while maintaining an economically sound posture.
143 Examiner sitting and patient fully reclined
The most frequently used arrangement for a tissue-specific examination is with the patient reclined and first adjusts the height of his/her stool so that the thighs are parallel with the floor or are at an angle of approximately 95° from vertical. Finally the height of the dental chair is adjusted. During palpation of the temporomandibular joints the elbows should be bent at a 90Q angle.
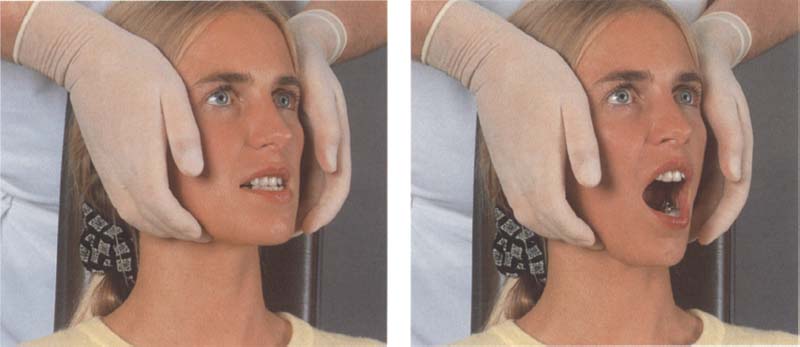
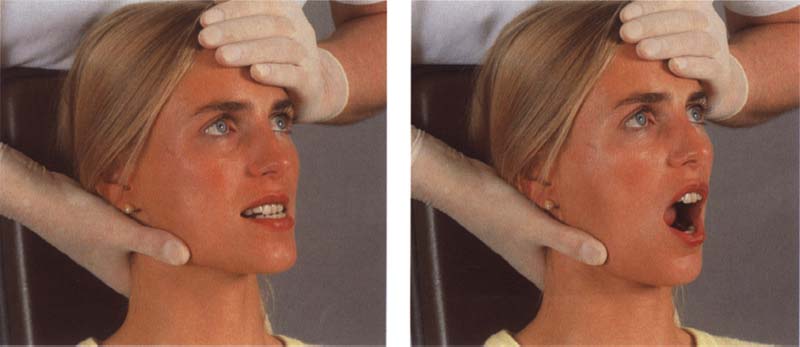
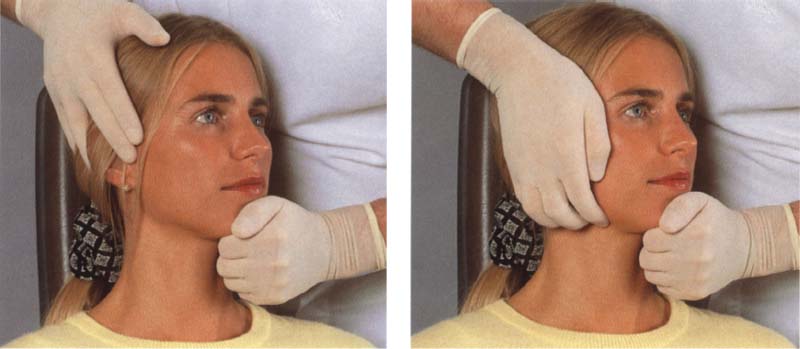
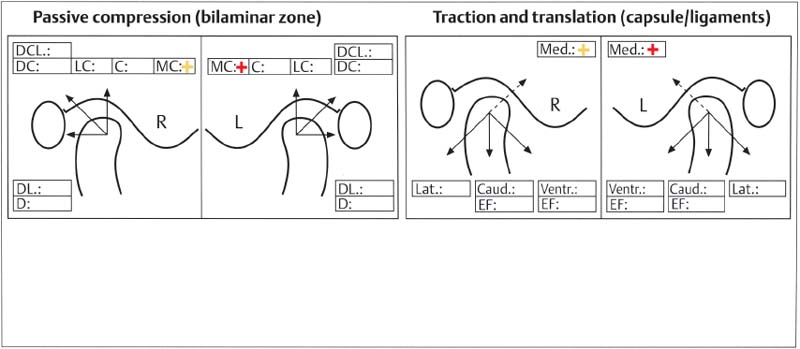
Manual Fixation of the Head
In addition to the correct positioning of the patient, optimal stabilization of the patient’s head is an important condition for achieving reproducible results during the examination. Regardless of the patient’s position, it is essential that the head of the patient be supported in all spatial dimensions at all times. A good examination technique requires that forces applied to the mandible in different directions cause no noticeable movements of the head. Not only does optimal stabilization have a positive effect on the patient’s opinion of the examination procedure but it also has solid medical grounds:
• Aggravation of a preexisting problem within the cervical spine must be absolutely avoided.
• Protection of the cervical spine of a patient with diffuse headache or tinnitus is of diagnostic importance. Placing stress on the cervical spine can in some cases precipitate tinnitus. The examiner, however, because he/she is performing a “temporomandibular joint examination” might mistakenly assume that the cause is arthrogenic.
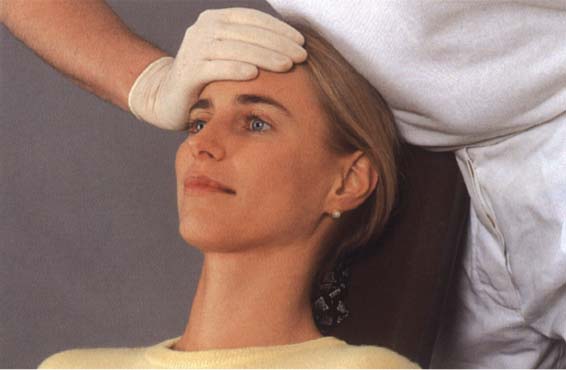
144 Clinician standing and patient semireclined
This combination allows the dynamic tests and the isometric contractions to be carried out quite reliably. However, optimal stabilization of the patient’s head is not always assured for the entire joint-play technique, and the clinician’s back is bent during a large part of the examination. For follow-up exams in which only a few manipulations are to be carried out, however, this position is ideal.
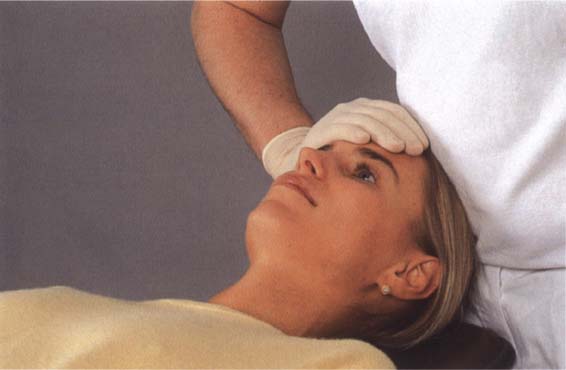
145 Clinician standing and patient fully reclined
Short clinicians who like to stand while working at the dental unit can achieve satisfactory stabilization for almost all examination techniques with this arrangement. If the examination is to take place on a treatment table with adjustable height, the headboard must be shortened to achieve adequate fixation of the head for the various techniques.
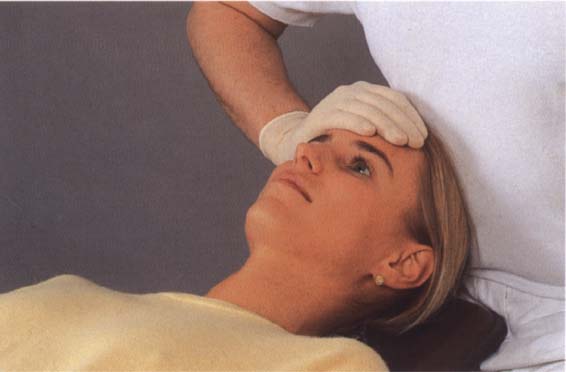
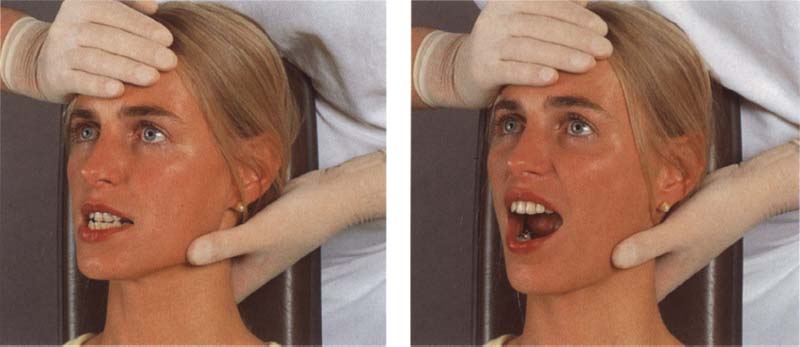
146 Clinician sitting and patient fully reclined
The ideal combination for reproducible examination results is a fully reclined patient and a seated examiner. All dynamic tests and isometric contractions can be performed from the 12 o’clock position. All joint-play tests are performed for the right joint from the 1 o’clock position and for the left joint from the 11 o’clock position. During almost all tests the patient’s head is stabilized in all three planes by the headrest, one of the clinician’s hands, and the clinician’s abdomen.
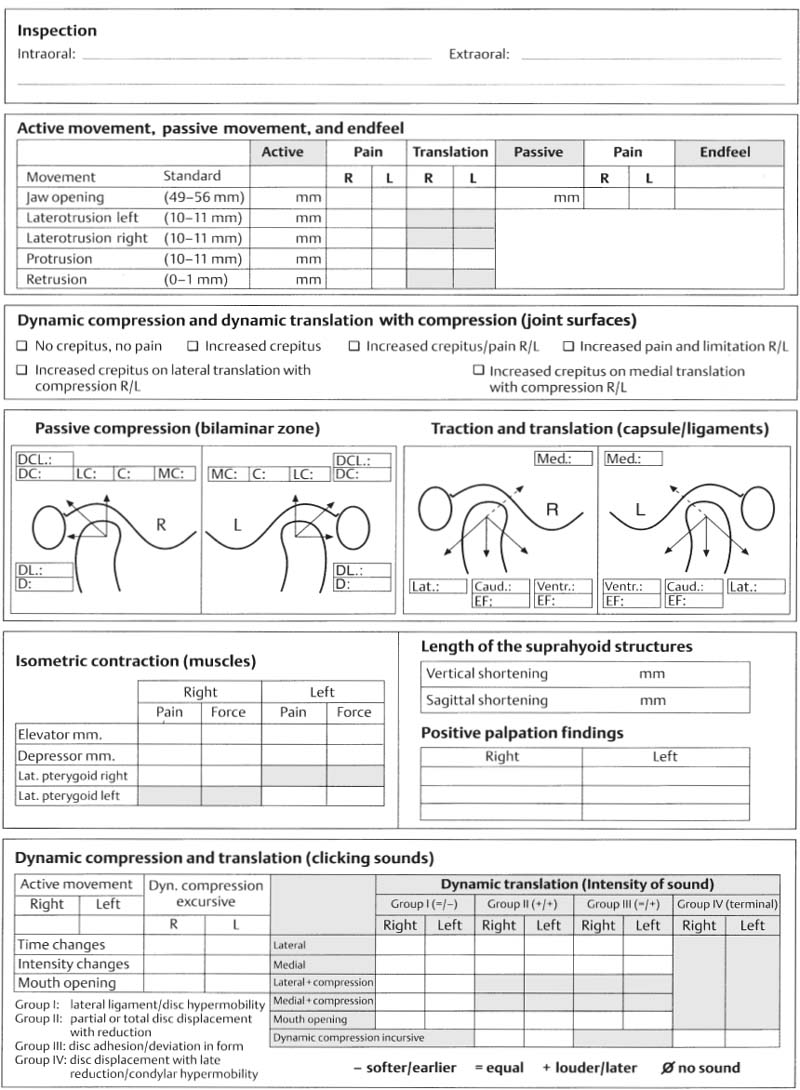
Active Movements and Passive Jaw Opening with Evaluation of the Endfeel
Examination of the extraoral portions of the masticatory system begins with observation of active jaw movements. Active movements do not contribute to the differential diagnosis (Szentpetery 1993), but serve only to document the initial conditions and to verify the symptoms described by the patient. Note is made of the extent of movements in millimeters and any accompanying pain and its location (right/left). None of this in any way supports a differential diagnosis but it does serve to test the conclusiveness of the reported symptoms.
Attention is given to any alteration in the path of movement of the incisal point (deviations and deflections) as has been recommended earlier (Wood 1979), but these are not documented. Because deflection to one side, for example, can have different arthrogenic causes (ipsilateral hypomobility or contralateral hypermobility), it makes more sense to determine the amount of condylar translation. This is done by palpating the lateral poles of the condyles during opening and protruding movements. Under normal conditions a condyle translates almost to the crest of the eminentia.
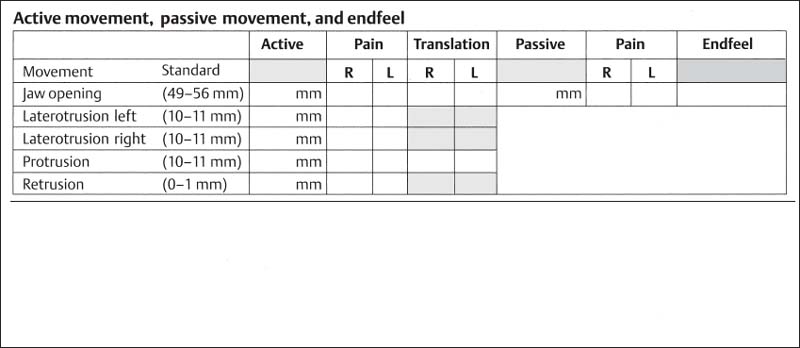
147 Chart for recording findings from active movements, passive jaw opening, and endfeel
Jaw opening is usually measured between the incisal edges of the incisors (Hesse 1996) and to this is added the overbite (anterior vertical overlap). This is especially meaningful in patients with a “deep bite” (large vertical overlap). The amount of “normal” jaw opening averages 53-58 mm (Ingervall 1970. Agerberg 1974, Wood 1979). Even 6-year-olds have jaw openings of 43-45 mm (Landtwing 1978, Vanderas 1992). Although women in general have more mobile joints (Beighton et al. 1973, Carter and Wilkinson 1964, Hesse 1996), men are able to open their jaws wider by 3-5 mm. According to Agerberg (1974a-d), jaw opening is directly related to body size. It decreases significantly with age and measures only 45-53 mm in 70-year-olds (Agerberg and Österberg 1974, Lysell 1984, Mezitis et al. 1989).
In a selected group of patients with temporomandibular joint problems average jaw openings were 45 mm in men and 39 mm in women (Carlsson and Swardstrom 1971). Contrary to the general clinical impression, a correlation between the extent of active mandibular movement and overall joint mobility is either nonexistent (Westling and Helkimo 1992) or is present only weakly in isolated cases (Dijkstra et al. 1994, Hesse 1996).
While there is little disagreement on the definition of a physiological jaw opening, views vary on what constitutes a limitation of jaw opening: Because only 1.2% of all (not selected) adults have a jaw opening of less than 40 mm(Bit-laretal. 1991), Okeson (1998) accepts this measurement as the boundary, whereas Ingervall (1970) considers a value of 41-42 as a reasonable boundary for limitation of opening. Clinically, however, the many deliberations over establishment of a cut-off value are of no relevance, because a patient may have a measurement of 48 mm, for example, and still be significantly limited because the value was 62 mm before some past event. Regardless of the “scientific boundary” (40-42 mm) a limitation of jaw opening always exists when a patient’s mandibular mobility is objectively found to be less than it was at a previous examination.
There are significantly fewer statements in the literature on the physiological extent of lateral movements. Ingerval (1970) gives average values of 9.8-10.5 mm, Agerberg and Österberg (1974) report 8.7-8.8 mm, and Hesse (1996) reports 10.0-10.5 mm. There is no significant difference between males and females. The ratio of jaw opening distance to lateral movement in a healthy system is approximately 6: 1 (Dijkstra et al. 1998). Lateral movements of less than 8 mm are generally classified as restricted (Ingervall 1970. Okeson 1998).
Protrusive movements are neglected in the literature and in the clinics even more than lateral movements. Still, the extent of protrusion (i.e. condylar translation) provides important information on the mobility of the joints, and therefore reveals over how broad a surface the forces are distributed (stress = force per unit of area). The reports range from 8.8 mm (Bergholz 1985) and 9.1 mm (Hesse 1996). Likewise, there is no sex-related difference in the extent of protrusion. Children give somewhat higher protrusive measurements than adults until the age of 10 years when their measurements are basically the same as those made on adults (Ingervall 1970).
Protrusive movements of less than 7 mm are considered to be restricted, although they are not always signs of pathology that urgently calls for treatment. It is especially important to test patients for restriction of lateral and protrusive movements following temporomandibular joint surgery and orthodontic or orthognathic surgery.
The determination of active movements is followed by an investigation of passive movements. This is to be done only on patients with limited but painless jaw opening, because painful joints will not permit the procedures needed for differential diagnosis of a limitation.
148 Endfeel during passive jaw opening
At the end of an active movement every healthy joint can be moved farther through a certain amount of space. This can occur only through the application of external force and is therefore referred to as passive movement (Kimberly 1979). In the early days of manual functional analysis all the mandibular movements were followed by tests of further passive movement. However, as 10 years of clinical experience has shown, this provided no additional diagnostic or therapeutic information so that passive tests are now applied only to the jaw-opening movement.
The extent of passive jaw opening, also referred to by some authors (Hesse et al. 1990) as the “endfeel distance,” has been reported in one study (Westling and Helkimo 1992) as 1.2 mm and in another (Agerberg and Österberg 1974) as 2.1 mm. Still more specific measurements can be found in the work of Hesse (1996), who reports an endfeel distance in men of 3.0 ± 1.1 mm under a force of 44.6 ± 7.2 N and in women, 3.8 ± 1.4 mm under 37.1 ± 2.1 N. The extent of mandibular movement is influenced by the ligaments, capsule, intra-articular structures, muscles, fascia, and the skin (Evjenth and Hamberg 1985, Hesse 1996).
Limitation of jaw opening is always accompanied by shortening one of more of the above-mentioned structures (Schneider et al. 1988). Therefore, at the end of passive jaw opening the so-called endfeel is recorded (Fig. 156ff).
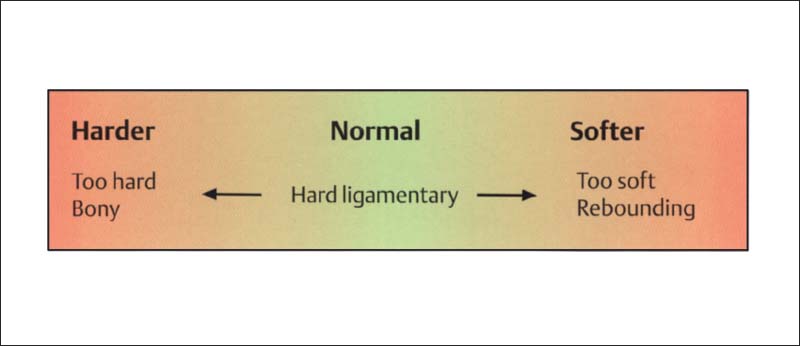
The endfeel is the feeling that the examiner detects at the end of a passive movement. It is always determined by the structures that are limiting the movement (Groot Landeweer and Bumann 1991). In healthy joints the endfeel is “hard ligamentary” and is not accompanied by pain (Cyriax 1979, Kaltenborn 1974, Janda 1974. Lewitt 1977, McCarroll et al. 1987, Hesse et al. 1990, Groot Landeweer and Bumann 1991, Bumann et al. 1993, Bumann and Groot Landeweer 1996b, Hesse 1996).
There are various classifications of the endfeel in the temporomandibular joint (Cyriax 1979, Evjenth and Hamberg 1985, Groot Landeweer and Bumann 1991, Hesse 1996). Clinically a distinction is made between physiological and structurally pathological endfeels (Figs. 148 and 161). Although there has been little inter-examiner agreement on the concept of the endfeel (Lobbezzoo-Scholte et al. 1994), Hesse (1996) could demonstrate a distinct correlation between the endfeel and the so-called “craniomandibular stiffness.” The evaluation of a combination of the extent of passive movement and the clinical endfeel is therefore a reliable parameter for the differential diagnosis of limitations of movement. Neither the endfeel nor the extent of passive movement helps to differentiate between myogenic and arthrogenic problems, as, for example, claimed by Fuhr and Reiber (1989).
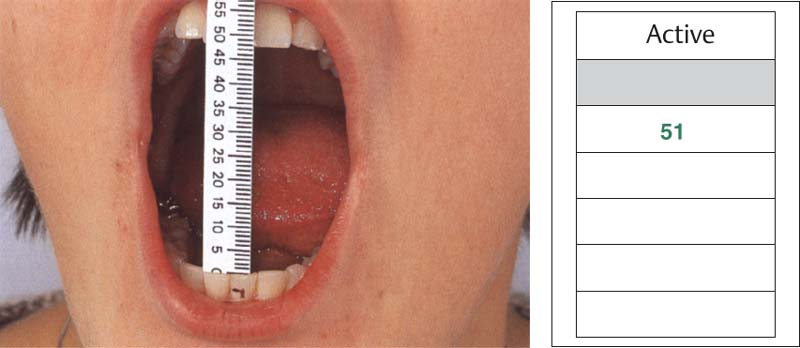
149 Active jaw opening
incisors at the level of the incisal edge of an upper incisor in maximal occlusion. Active jaw opening can be measured directly or by measuring the incisal edge distance as shown here and adding to it the anterior vertical overlap (“overbite”).
Right: In the record of findings, green ink is used to enter the amount of pain-free movement and red Is used for painful movements.

150 Active movement of the mandible to the left
To measure lateral mandibular movements the upper midline is first projected onto the labial surface of a lower incisor. Then the patient executes a maximal lateral movement and the distance between the upper midline and the mark on the lower tooth is measured.
Right: The measurement is entered in the chart in the same way as the jaw-opening distance. The “normal” range is 10.5 ± 2.7 mm.
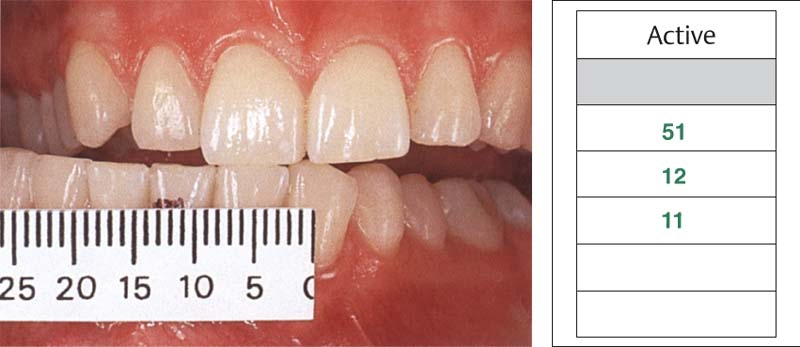
151 Active movement of the mandible to the right
After a maximal movement of the mandible to the right, the distance from the upper midline to the lower mark is measured.
Right: Again, the specific entry is the jaw-opening value. The norm for men is 10.2 ± 2.3 mm and for women 10.3 ± 3.4 mm. The normal values given here for the two sides are taken from studies by Hesse (1996).
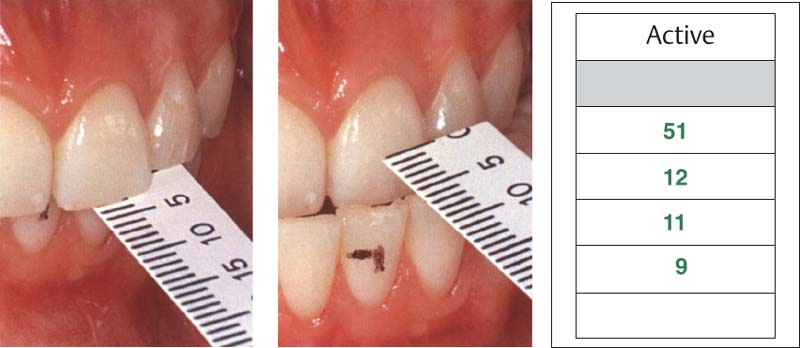
152 Active protrusive movement
To determine the extent of protrusion, the horizontal overlap ( over-jet”) is measured first and then added to the distance between the upper labial surface and the lower incisal edge after maximal protrusion. This can be done with either a simple ruler or with the back side of a commercial sliding caliper.
Right: Entry in the patient’s record is made in green or red. Normal values are 9.0 ± 2.8 mm for men and 9.1 ± 1.8 mm for women.
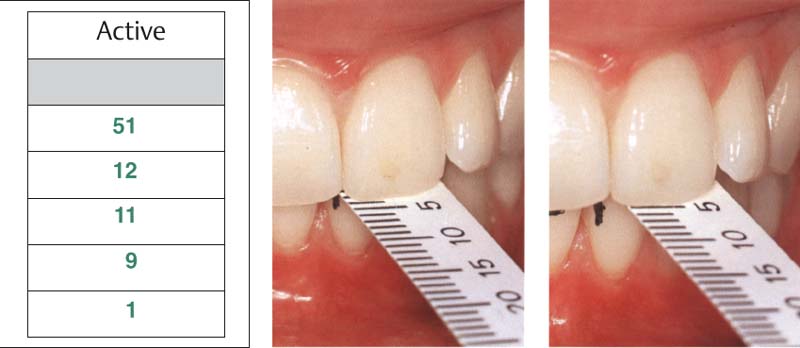
153 Active retrusive movement
First the horizontal overjet is measured in habitual occlusion with a ruler or sliding caliper. Then the patient is Instructed to “pull the lower jaw back” or -push the upper jaw forward” as far as possible. The read directly, although this is of no importance in making a differential diagnosis. Left: The chart entry is made in the usual manner. Values range from 0 to 2 mm.
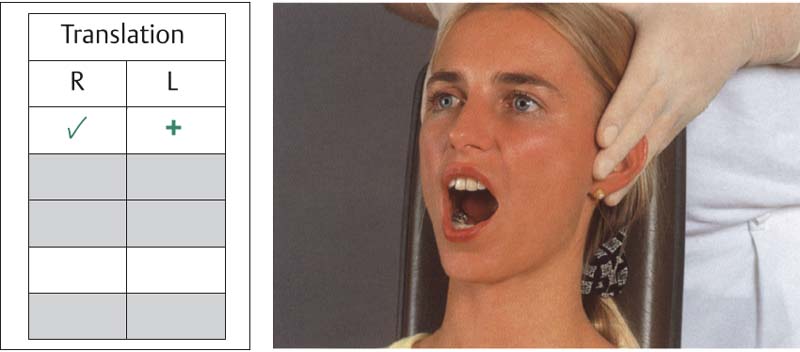
154 Translation of the condyles during active jaw opening
A qualitative evaluation of condylar translation can be made by palpation. Normally during jaw opening the condyles move only to the crest of the articular eminence. The mobility (✓), hypomobility (-), or hypermobility (+). Left: Example of chart notations using the corresponding symbols. Upon jaw opening, mobility of the right condyle was normal while there was hypermobility of the left condyle.
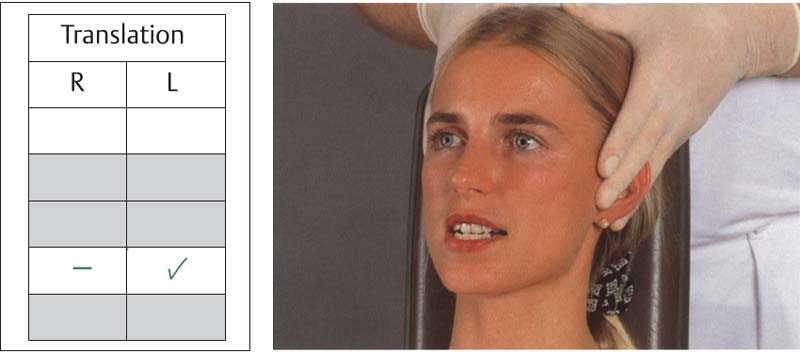
155 Translation of the condyles during active protrusion
The extent of condylar translation during protrusive movement is also determined. A movement that stops just short of the crest of the but a condyle that passes beyond the eminence is considered hypermobile. If the condyle moves out of the fossa only slightly or not at all, it is hypomobile.
Left: This entry in the examination form indicates that the right condyle was hypomobile and the left had normal mobility. This test replaces the documentation of deviation and deflection.
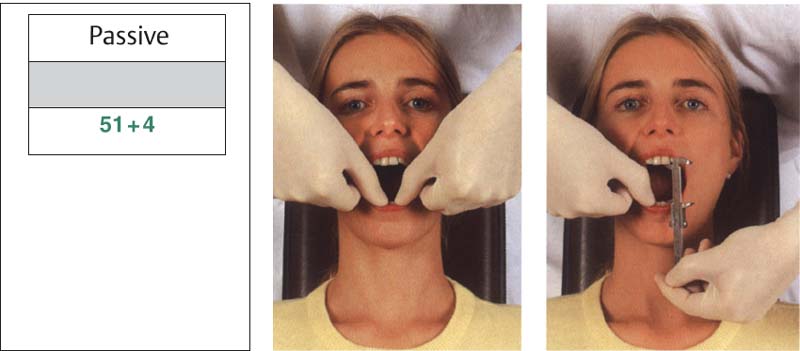
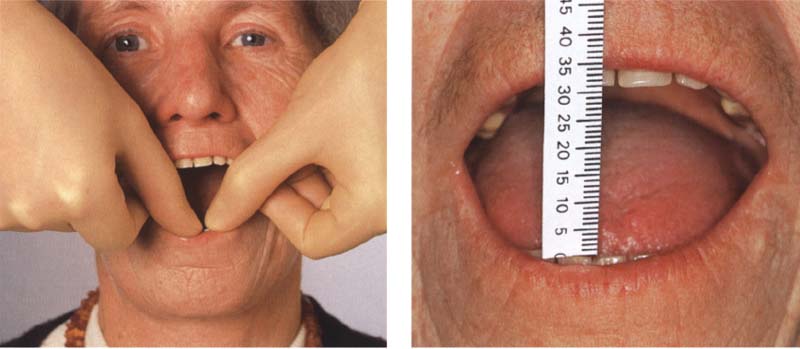
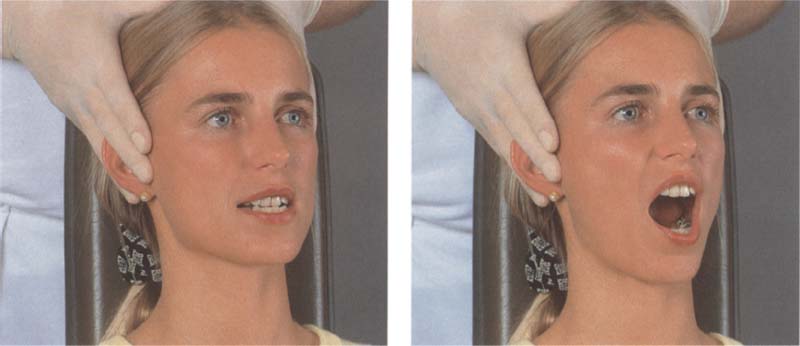
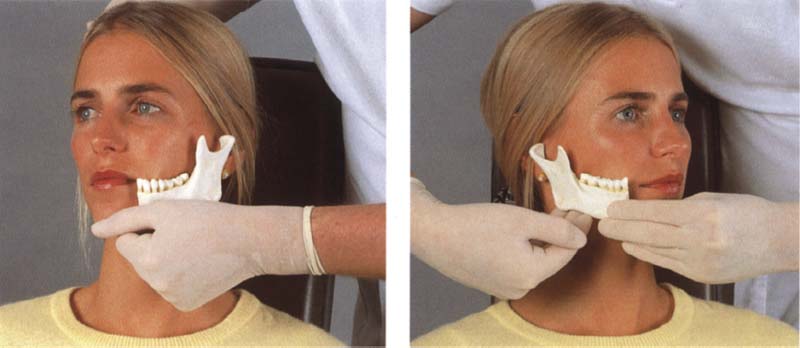
156 Further passive jaw opening beyond active opening
Passive jaw opening is usually executed with both hands. The index or middle fingers are placed on the upper premolars and the thumbs on the lower incisal edges. The patient opens the mouth as far as possible and at the end of the active movement the clinician assists further opening. The amount of passive movement is evaluated. If the one-handed technique is used the distance can be measured with the other hand.
Left: Chart entry.
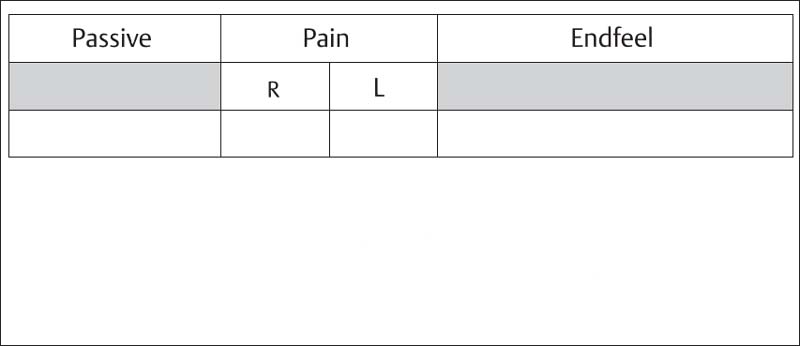
157 Section of examination form dealing with passive jaw opening
If there is pain upon passive jaw opening, the amount of movement is written in red. Then the amount of force needed to elicit pain is indicated by means of red plus signs (+, ++, +++) written in the box for the painful side. The endfeel is recorded only when jaw opening is painless, otherwise the patient will reflexively tense the muscles.
158 Limited jaw opening resulting from skin changes in scleroderma
Left: In a patient with scleroderma, taut cords form In the skin during passive jaw opening and the end-feel is “too hard.” Right: Sclerosing of the skin causes typical limitation of jaw opening to 30-35 mm. This must not be confused with a nonreducing disk displacement.
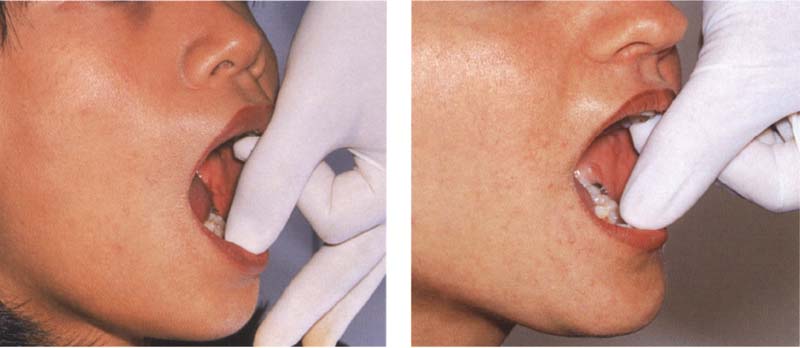
159 A “too soft endfeel” with passive jaw opening
Left An endfeel that is “too soft” accompanied by condylar hypermobility. The length of the jaw-closing muscles limits opening movements when there is lengthening or overstretching of the capsule and ligaments. Rigbt: A “too soft” endfeel accompanied by reduction of jaw opening. Tensed or shortened elevator muscles are limiting the extent of jaw opening.
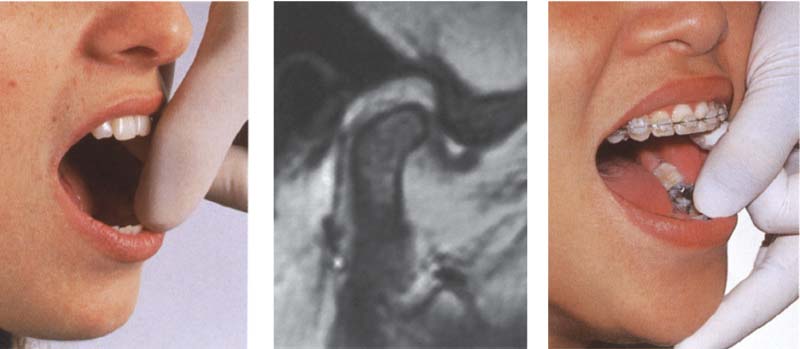
160 An endfeel that is “too hard” and “rebounding”
Left: A “too hard” endfeel with restricted jaw opening. The shortened capsule and ligaments are limiting jaw opening.
Center: MRI image of the nonreducing disk displacement at maximal jaw opening.
Right: Rebounding endfeel at the end of a restricted jaw-opening movement. The nonreducing anterior disk displacement limits jaw opening.
Differential Diagnosis of Restricted Movement
Nonpainful limitations of movement can be differentiated only by evaluating the endfeel after passive movement. The ability to make an exact determination of the endfeel requires practice and a little experience. This is the only method by which structural causes of restricted movement can be discovered. The elicited endfeel is merely verified secondarily through other methods such as the joint play technique, radiographs, or MRI. These, however, are not indicated for use as primary differential diagnostic procedures. During the passive jaw-opening procedure 92.5% of patients report a drawing sensation in the preauricular region (Hesse 1996). This false perception can be accounted for by the stretching of the joint capsule and the lateral ligament.
If passive jaw opening causes the patient pain, the endfeel cannot be used to aid in making a differential diagnosis of limited movement. Therefore, when the signs and symptoms include the combination “pain and restricted movement,” the pain must be treated first before an adequate differential diagnosis of the restricted movement can be made.
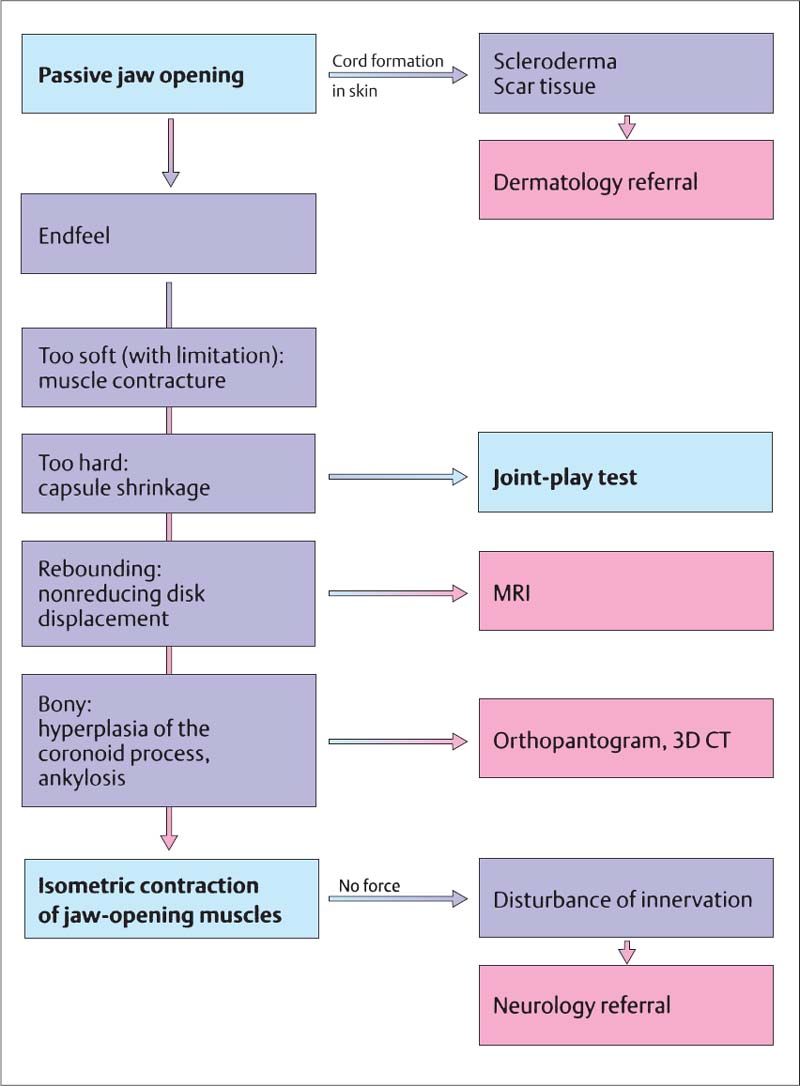
161 Examination sequence when there is a nonpainful limitation of jaw opening
The diagram shows the sequence in which the examination techniques are to be carried out. In a patient with scleroderma tight cords appear in the skin during passive jaw opening (Fig. 158). In these cases the dentist can prescribe mobilization exercises (“jawsercises,” Korn 1994) and refer the patient to a dermatologist if the disease is not already being treated. In patients with restricted jaw opening the endfeel may assume one of four characteristics: too soft, too hard, rebounding, or bony.
• Reduced jaw opening produced by shortening of the muscles gives a “too soft” endfeel during passive jaw opening (Groot Landeweer and Bumann 1991. Stengenge et al 1993).
• A “too hard” endfeel indicates a shortened capsule (Bumann et al. 1993). This finding can be corroborated by testing the endfeels from anterior translation and in ferior traction (Fig. 201ff).
• A “rebounding” endfeel is evidence of a nonreducing disk displacement (Fig. 160). This can be verified through MRI. However, a nonreducing disk displacement seen on a MRI is not necessarily the cause of restricted movement. Therefore the MRI cannot be relied upon as the primary diagnostic tool.
• A “bony” endfeel indicates osseous changes. Disrupted innervation can be ruled out through isometric contraction of the jaw-opening muscles.
Examination of the Joint Surfaces
The functional articulating surfaces of the temporomandibular joint are the fibrocartilaginous articular portions of the temporal bone and the condylar process of the mandible as well as the articular disk. Because the resultant force of the muscles of mastication is directed anterosuperiorly (Chen and Xu 1994), this is where the functional joint surfaces are found.
The proteoglycans in the fibrous cartilage are responsible for the disk’s resistance to compression (Kopp 1978, Axels-son et al. 1992). Although a reduced content of proteoglycan significantly alters the compressive characteristics of cartilage, it has no negative effect on its frictional properties (Pickard et al. 1998). The ability of the joint surfaces to deform serves to cushion and distribute peaks of stress. It also helps lubricate the contacting joint surfaces to minimize friction and wear (Mow et al. 1993, Murakami et al. 1998). The conformity of the joint surfaces plays a decisive role in the lubrication process (Nickel and McLachlan 1994b). The coefficient of friction of a healthy joint is 0.007. Lavage can cause this to increase three-fold, and following introduction of hyaluronic acid friction is reduced again by half(Mabuchi et al. 1994).
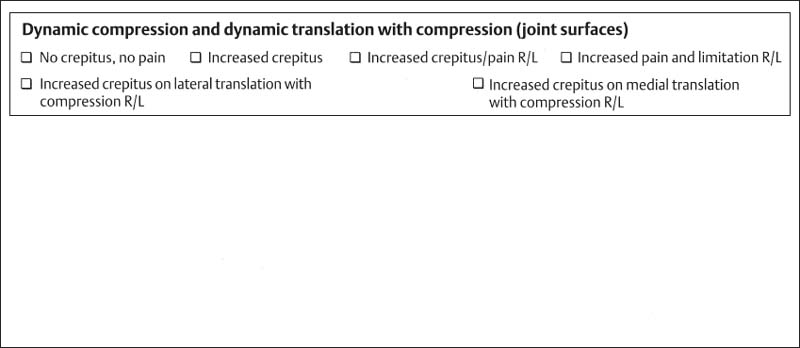
162 Form for recording signs and symptoms
Excerpt from the manual functional analysis examination form for recording the results of the dynamic compression and dynamic translation tests for the current degree of adaptation of the joint surfaces. The upper row is for the results of the dynamic compression test and the lower row is for the dynamic translation test. With these findings one can differentiate between osteoarthrosis, osteoarthritis, and capsulitis of the bilaminar zone with nonreducing disk displacement.
The joint surfaces in the temporomandibular joint become deformed when loaded (Moffet 1984). Destructive changes in the joint surfaces occur six to eight times more frequently in women than in men (Toller 1973, Rasmussen 1981, Tegelberg and Kopp 1987), which indicates that either the adaptability of women’s joints is less or the harmful influences are stronger. The effect of a force depends on its amplitude, frequency, and duration (Gradishar and Porterfield 1989, Bell 1990).
Motion reduces the deforming effects. Conversely, restrictions of movement intensify the deforming effects. As long as the adaptability of the tissue is not exceeded, the articulating surfaces of the temporal bone and condyle can become remodeled (adapted), but otherwise degenerative changes will occur in the joint surfaces (Moffet et al. 1964, Solberg 1986, Copray et al. 1988). The capacity for progressive and regressive adaptation of the osseous portions of the joints is present throughout life (Griffen et al. 1975). Surgical osteotomies on one or both jaws are followed by distinct adaptive changes of the condyle in approximately 23% of adult patients (Hoppenreijs et al 1998). Adaptive changes of the condyle and fossa could also be found in more than half the joints after mandibular midline osteodistraction treatment to stimulate osteogenesis (Harper et al. 1997). The disk, on the other hand, is not capable of cellular remodeling (Moffet 1984). Therefore, loading of the disk can produce only reversible (elastic) or irreversible (plastic) deformation.
Histologically, slightly elevated levels of functional loading lead to thickening of the cartilage on the joint surfaces (Muir 1977. Radin et al. 1978). A further increase in loading interferes with fluid exchange and disrupts the supply of nutrients (Gradishar and Porterfield 1989, Haskin et al. 1995), thereby causing increased tissue degeneration (Ateshian and Wang 1995). Short term loading (less than 2 minutes) of the articular cartilage lowers the coefficient of friction, whereas a load applied for 45 minutes causes a five-fold increase in friction! Cyclic short-term loads allow a high water content in the cartilage and are accompanied by reduced friction (Nickel and McLachlan 1994a). Neither occlusal attrition nor the thickness of the cortical layer of bone as seen in a radiograph provides any reliable indication of the current thickness of the fibrocartilaginous joint surfaces (Pullinger et al. 1990). Contours of the bone seen on the radiograph do not correspond to the actual contours of the joint surfaces!
A noninvasive determination of the stages of regressive adaptation of the joint surfaces can only be made clinically, not by imaging procedures. For this we use the so-called dynamic compression and dynamic medial and lateral translation (sometimes with compression). The fundamentals and clinical procedures are described on the following pages.
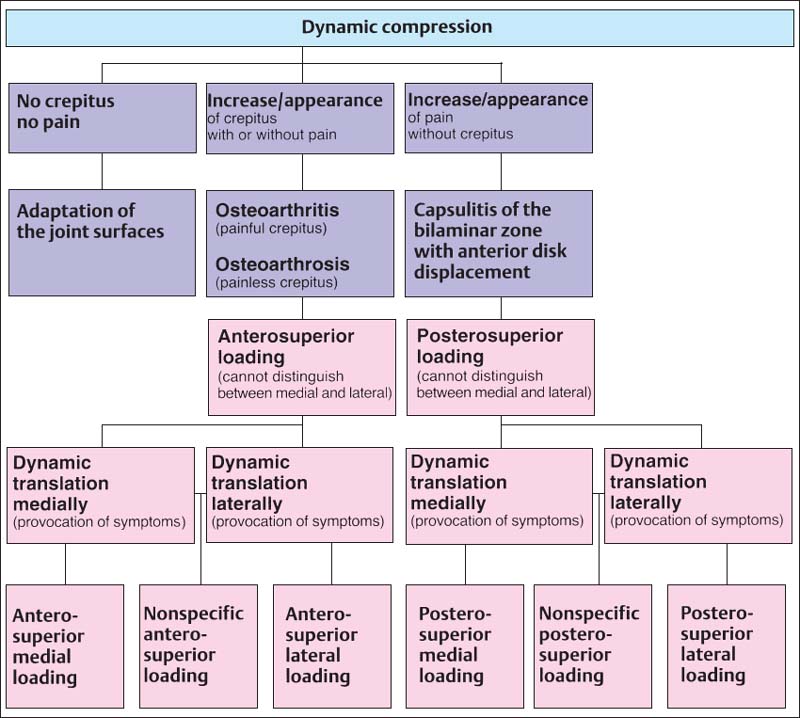
163 Examination techniques and their usefulness in differentiating between injuries/lesions of the joint surfaces
Active movements, dynamic compressions, and medial and lateral dynamic translations are all used to serve as nonmanipulated references for specific testing of the joint surfaces. Through the findings from the dynamic compression test it is possible to conclude whether there is an adapted joint surface, osteoarthrosis, osteoarthritis, or capsulitis of the bilaminar zone in the presence of a nonreducing disk displacement (pp. 70–74). Use of the dynamic translation test permits further determination of whether a regressive adaptation and its associated loading vector lie more medially or laterally. This knowledge is essential later during clinical testing of influences to determine whether or not there is a causal relation with occlusal disturbances.
Frequently temporomandibular joints with obvious radiographic changes in the bone show only insignificant clinical symptoms or none at all (Mejersjö and Hollender 1984). Because of this the purpose of a specific functional joint-surface test is only to determine whether or not the joint surfaces are adapted or not. Diagnostically and therapeutically, it is of minor importance how the structures are represented by imaging procedures.
There is a close correlation between regressive adaptations of the functional joint surfaces and crepitus (Boering 1994, Hansson and Nilner 1975, Bates 1993, Pereira et a!. 1994). Controlled studies indicate that crepitus is a reliable clinical sign of osteoarthritis (Holmlund and Axelsson 1996). Within a selected group of temporomandibular joint patients, 3-24% were found to exhibit rubbing sounds (Bates et al. 1994, Zarb and Carlsson 1994).
Sometimes the degeneratively altered joint surfaces are also painful. Even though in the 20th embryonic week the disk is supplied with numerous nerve endings, no innervating structures remain to be seen after birth (Ramieri et al. 1996). Therefore the disk can be excluded as a source of pain. As long as the temporal and condylar joint surfaces are still covered with cartilage, they too are unable to give rise to pain. It is only when subchondral bone is exposed that the nociceptors transmit corresponding pain sensations (Quinn 1989, Kamminishi and Davis 1989).
Conventional clinical examination methods can diagnose initial osteoarthrotic changes only with a low degree of specificity and sensitivity. Therefore manual functional analysis employs not only active protruding and opening movements, but also dynamic compressions and translations, which load the corresponding joint surfaces more heavily during movements. In this way even compensated joint surface changes can be discovered early by provoking a painful response.
Crepitus is a primary examination parameter. The examiner must determine whether at any given moment during manipulation the rubbing sound occurs more loudly and distinctly than during nonmanipulated active movements (protrusion and opening). In addition it should be determined if there is any pain produced by compression. Whenever there are painful alterations in the joint surfaces, the endfeel of inferior traction and anterior translation must be tested before any conclusions are formed about the effectiveness of a possible unloading of the joint. The results of the tests of the joint surfaces allow the following deductions to be made:
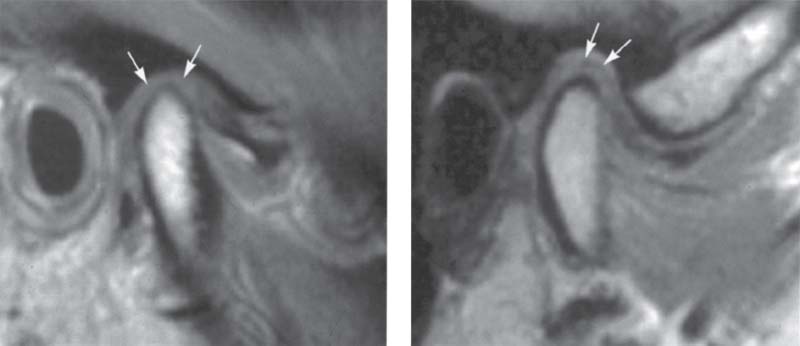
• Adaptation: no crepitus and/or no pain during active movements and dynamic tests
• Compensation: crepitus and/or pain only during the dynamic tests
• Decompensation: crepitus and/or pain during active movements and during dynamic tests.
Manifestations of Joint Surface Changes
Unlike other synovial joints the temporomandibular joint has joint surfaces of fibrous cartilage, a highly differentiated connective tissue with no blood vessels or nerve endings. Compared with hyaline cartilage, fibrous cartilage is less easily deformed because of its higher fiber content (Gay and Miller 1978). The mucopolysaccharide content of the synovial fluid is responsible for lubrication of the joint surfaces (Smith 1982). This is why there are normally no noises or pain during active movements and during dynamically influenced movements.
• An increase of crepitus during dynamic compression in the absence of pain indicates osteoarthrosis, a regressively adapted, noninflammatory stage of joint surface damage.
• If crepitus and pain are both provoked there is osteoarthritis, an inflammatory stage of joint surface damage.
The examiner must make certain that the provoked pain is intensified by application of compression and not by a nonspecific joint loading due to increasing jaw opening.
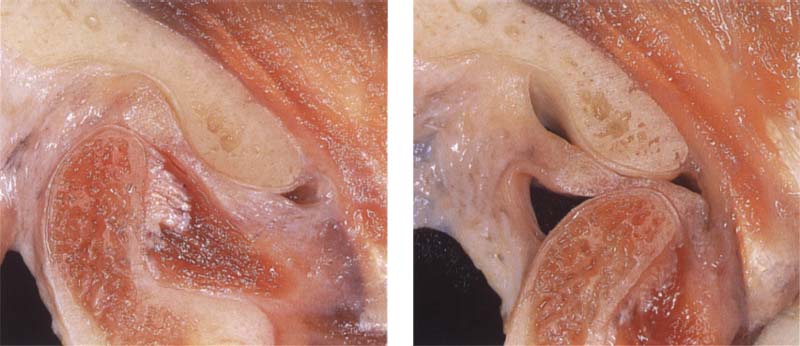
164 A healthy joint
Left: Anatomical preparation of a right temporomandibular joint with the jaws closed. The rounded condyle is covered by a uniform layer of fibrous cartilage. There is no fibrous cartilage on the superior and posterior portions of the fossa. Only the posterior slope and the crest of the articular eminence exhibit functional joint surfaces.
Right: During jaw opening there are no grating sounds or pain.
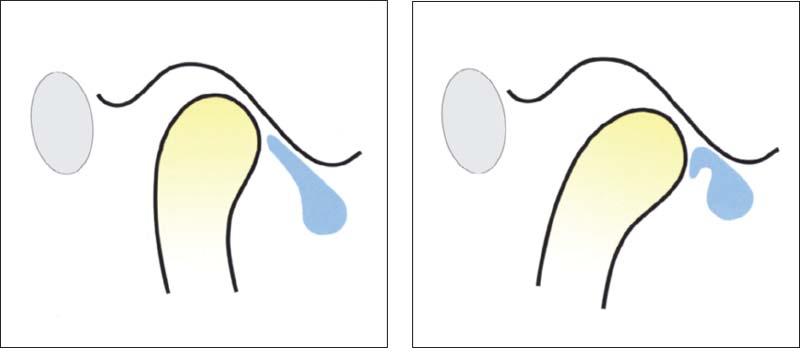
165 Nonreducing anterior disk displacement
If the disk is displaced anteriorly when the mouth is closed, the top of the condyle will be covered by part of the overstretched bilaminar zone, which at this time acts as the articulating surface. The compression test will intensify pain in this area.
Right: As the jaws are opened, the condyle pushes the disk ahead of itself, thus increasing pain and limitation of movement.
166 Adaptation of the bilaminar zone after anterior disk displacement
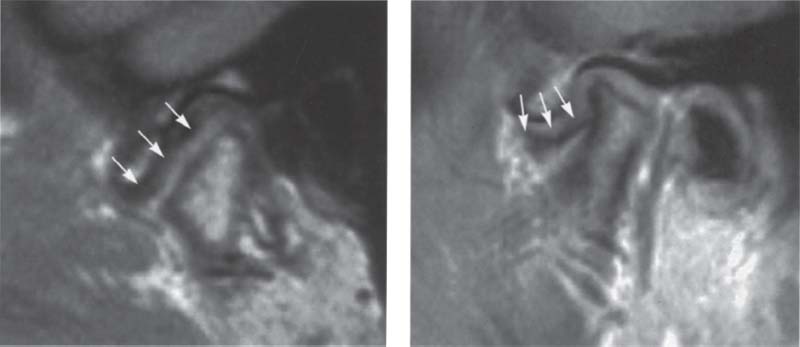
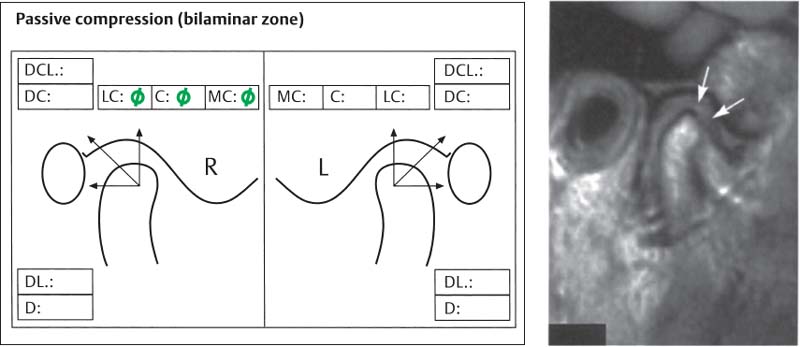
Left: Dynamic compressions are associated with pain and limitation of movement only if the bi laminar zone has not adapted as seen in this MRI (light gray, arrows).
Right: This MRI shows an adapted (fibrosed) bilaminar zone as dark gray (arrows). Under the right circum stances dynamic compression will provoke no pain and the joint will require no treatment.
In contrast with other definitions (Stegenga 1991), osteoarthritis is not a joint surface lesion with inflammation of the surrounding soft tissues, but rather a destruction of fibrous cartilage with painful exposed subchondral bone.
Osteoarthrosis and osteoarthritis can occur with or without disk displacement and, as previously stated, may accompany disk perforation. It cannot be differentiated clinically for each individual case, but this is not relevant to the treatment.
Nonreducing disk displacement represents a special case. If under dynamic compression there is no crepitus but pain and limitation of the jaw-opening movement, capsulitis of the bilaminar zone with nonreducing disk displacement should be suspected. In this situation the disk is anteriorly displaced and no repositioning occurs during jaw opening. A portion of the overstretched bilaminar zone lies over the top of the condyle. If this portion has not become adapted through fibrosis, it produces pain that is increased by dynamic compression. Protrusion or jaw opening will further increase the pain so that the clinical appearance of restricted jaw opening results. The clinical presumptive diagnosis can be reinforced through passive superior compressions and, if necessary, verified by imaging procedures.
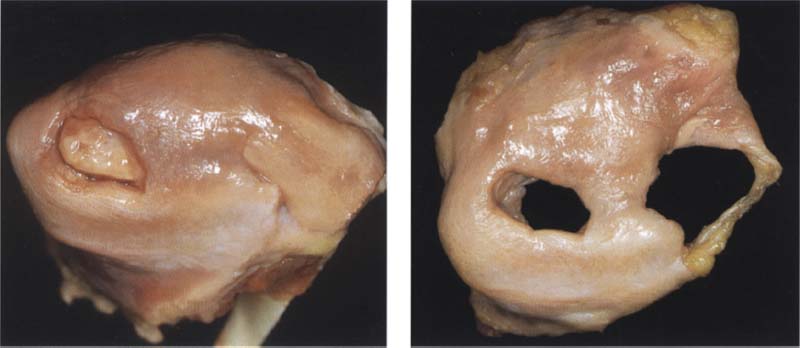
167 Perforation of the articular disk
Left: For diagnostic and therapeutic purposes, a disk perforation is regarded as a change in the temporal or the condylar joint surfaces. This type of joint surface damage usually has an anterosuperior loading vector. Treatment is always directed in the direction opposite the loading vector regardless of morphological relationships.
Right: For this reason, arthrography is not indicated for disk perforations
168 Osteoarthrosis/osteoarthritis and disk perforation
Left: Disk perforations in combination with degenerative changes in the joint surfaces occur frequently in the center of the disk or in the bilaminar zone.
Right: During jaw opening under compression there will be intensified rubbing sounds, possibly accompanied by increased pain. In many cases the disk perforation (blue) cannot be satisfactorily diagnosed. However, this is not necessary for treatment purposes.
169 Osteoarthrosis/osteoarthritis and disk displacement
Left: Condyles with degenerative changes can exhibit many different forms. In a few cases like this the areas of bone damage are not associated with significant changes in position and shape of the disk (arrows).
Right: Severely deformed joints, however, are usually accompanied by disk displacement (arrows) or perforation. Regardless of the position of the disk, the inferior surfaces of disks are affected by degenerative changes almost three times as frequently (57%) as the superior surfaces (Kondoh et al. 1998).
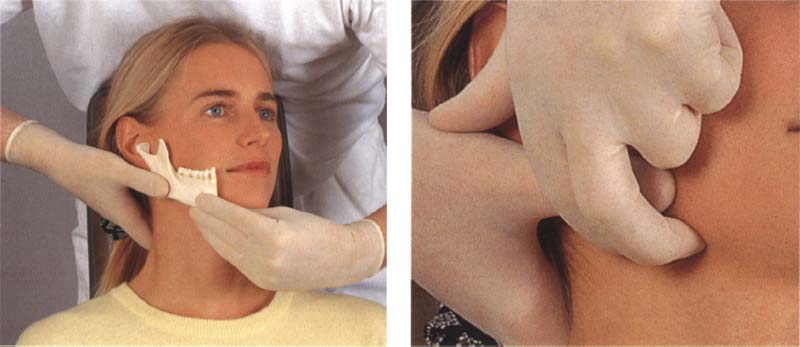
Conducting the Clinical Joint Surface Tests
Testing of the functional joint surfaces on the patient begins with active movements. For this the examiner, while either standing or sitting at the 12 o’clock position, places two fingers over each condyle and then instructs the patient to first protrude the lower jaw as far as possible and then make a maximal jaw-opening movement from the protruded position. During these movements both examiner and patient remain alert to any isolated grating sounds or grating sounds in combination with pain. As a rule, crepitus during protrusion comes from the temporal joint surfaces and crepitus during jaw opening from the condylar surfaces.
These active movements serve as a base of reference for the following tests.
For the dynamic compression test, the examiner places two or three fingers under the angle of the mandible on each side so that neither the facial blood vessels nor the medial pterygoid muscles are significantly disturbed. The examiner now exerts a superior or anterosuperior pressure while the patient again protrudes and then opens to the maximum. Under physiological conditions, neither rubbing sounds nor pain will occur during the movements.
170 Active protrusion followed by jaw opening
Left: Active movements serve as a reference (control) for the dynamic tests. As the examiner palpates the condyles, the patient executes a maximal protrusive movement
Right: From the position of maximal protrusion the jaws are then opened to the maximum. Both the examiner and the patient remain alert to any rubbing sensations that may arise, either with or without pain.
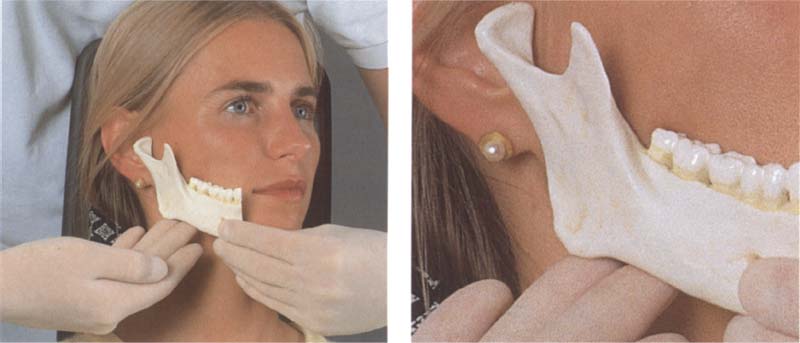
171 Positioning the middle and ring fingers at the angle of the jaw for performing dynamic compressions
Left: For dynamic compression two or three fingers are placed under the horizontal part of the angle of the mandible in such a way that the facial blood vessels and the insertion of the medial pterygoid muscle will be compressed as little as possible.
Right: Enlarged view showing the finger position at the angle of the jaw in greater detail.
172 Dynamic compression during protrusive and opening movement
Left: As the examiner presses superiorly or anterosuperiorly, the patient pushes the lower jaw forward as far as possible. Rubbing sounds that occur now usually arise from the temporal surface of the joint.
Right: Next, as the upward pressure is maintained, the patient opens the jaw as far as possible. Crepitus, pain, and any restrictions of movement that occur are recorded to help in making a differential diagnosis
Crepitus during the protrusive movement indicates osteoarthrotic changes in the temporal joint surface, while crepitus during the opening movement points to changes on the condyle.
If dynamic compression provokes crepitus with pain (osteoarthritis) or crepitus without pain (osteoarthrosis), the examination is continued with dynamic translations. These can be conducted with or without manual compression. In this section of the book dynamic translation without compression is depicted, while the technique with the addition of compression can be seen on page 105.
Dynamic translations in the lateral and medial directions are specific for evaluating the lateral and medial portions of the joint surfaces. This is especially important when there is incongruence of the joint surfaces in the frontal plane. The parameters that can be distinguished by the dynamic tests are summarized below.
• Osteoarthosis vs. osteoarthritis: the tests either proceed painlessly or they elicit pain
• Temporal vs. condylar: symptoms appear either during protrusion or during jaw opening
• Lateral vs. medial: symptoms appear either during lateral or during medial translation.
173 Hand position for dynamic translations
Left: To stabilize the head, one hand is placed flat against the back of the patient’s neck. This also stabilizes the cervical spine. The thumb is placed at the level of the angle of the mandible.
Right: The other hand braces the forehead from the opposite side. Now a force can be applied by the thumb medially toward the contralateral jaw angle. The result is a medial translation of the left condyle and a lateral translation of the right condyle.
174 Dynamic translation of the mandible to the right
Left The transitional force is continued as the patient moves the mandible forward as far as possible, peat the movement until a clear determination can be made. This tests the integrity of the lateral joint surfaces in the right joint and the medial surfaces of the left joint.
Right: from the position of maximal protrusion the patient makes a maximal opening movement, and any rubbing sounds that occur are recorded.
175 Dynamic translation of the mandible to the left
Left: The examination procedure is repeated in a similar manner for the opposite side. After the head is stabilized at the neck and forehead, pressure is applied to move the mandible bodily to the left. The protrusive movement tests the medial joint surfaces on the right side and the lateral joint surfaces on the left.
Right: Finally the patient makes a maximal active opening movement from the maximal protrusive position.
Examination of the Joint Capsule and Ligaments
Following the joint surface tests, those patients who have been experiencing pain are always examined Further using joint manipulation techniques. Like all orthopedic examination techniques, these can be traced back to the fathers of manipulative medicine, J Cyriax, F Kaltenborn, G Maitland, and J Mennell (Cookson and Kent 1979). The specific joint manipulation techniques for orthopedics were first described by Mennell (1970). Hansson et al. (1980) were the first to recommend their use on the temporomandibular joint in dentistry.
The joint manipulation techniques consist of:
• passive compression,
• translation, and
• caudal traction.
In perspective, these are the most important clinical tests for the differential diagnosis of inflammatory changes in the joint region (Friedman and Weisberg 1982, 1984; Palla 1992; Riddle 1992; Bumann et al. 1993; Bumann and Groot Landeweer 1996b; Hesse 1996). Because there is no “gold standard” against which to measure results, their precise scientific verification is difficult (Hesse 1996).
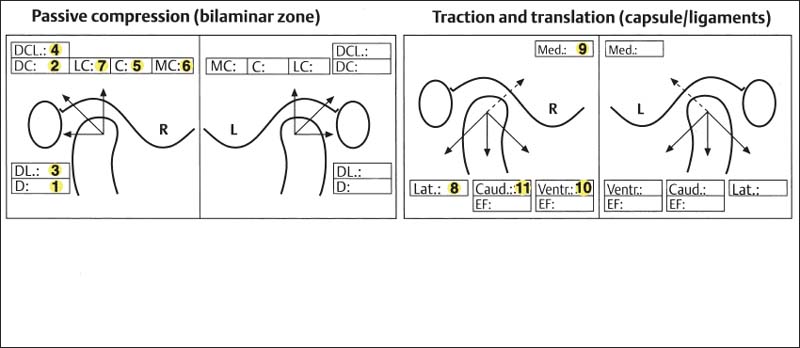
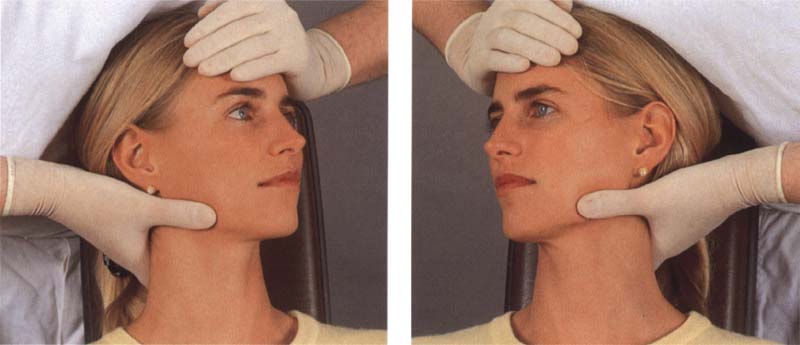
176 Form for recording the findings of the joint-play tests
Passive compression, translation, and traction are all included under the concept of joint-play techniques. Pain that can be repeatedly provoked is recorded with color coding In the appropriate box on the form. The various sections will be explained more fully on the following pages. The numbers indicate the sequence in which the steps are carried out.
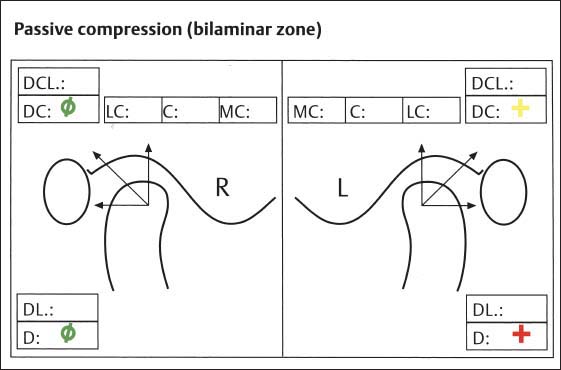
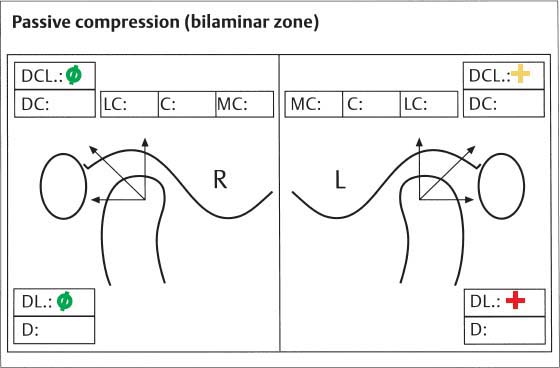
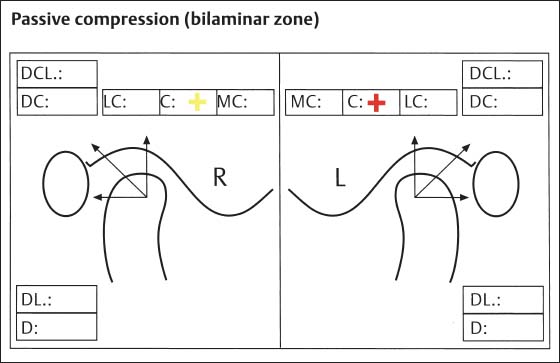
With passive compression the bilaminar zone is examined for poorly adapted areas. Translation and traction serve to test the capsule and ligaments.
The examination always begins with passive compression (Bumann and Groot Landeweer 1996b). The rationale of the examination is based upon elicitating pain by loading various joint structures in different directions. In healthy joints, these manipulations are never painful (Palla 1986, Bumann and Groot Landeweer 1992, Curl and Stanwood 1993, McNeill 1993, Hesse 1996), because under physiological conditions the lateral ligament, acting as a motion-limiting structure, prevents injury to the bilaminar zone.
However, if the lateral ligament becomes overextended, pain sensations can emanate from the bilaminar zone because of its rich innervation (Scapino 1991a, b) or from various parts of the capsule. During passive compression the muscles of mastication are not active and are not loaded. Because the disk and the joint surfaces are not innervated, they can be ruled out as sources of pain that can be repeatedly provoked. Therefore pain that can be provoked through posterior (retrusive) and/or posterosuperior compression is evidence of inflammation in one or more areas of the temporomandibular joint (Palla 1992, McNeill 1993, Bumann and Groot Landeweer 1996b). The high level of diagnostic reliability of passive compression has been demonstrated in clinical studies (Lobbezoo-Scholte et al. 1994, de Wijer et al. 1995).
If the dynamic tests for evaluating a patient’s joint surfaces produce pain, then no diagnostically useful information can be gained through applying superiorly directed pressure during the same appointment.
Pain patients are able to report current pain with relative exactness (Cousins 1989. Bell 1991, Stacey 1991. Hewlett et al. 1995) and their reports can be useful in making a differential diagnosis. Seven passive compression tests are available and these are carried out in a definite sequence for ergonomic efficiency. Following each manipulation the patient is asked if pain occurred and if so, whether it was the same as that previously experienced or if it was elicited only by the momentary loading. In this way, as with the joint surface problems, three conditions of the bilaminar zone can be described:
• Adaptation (condition green): no history of pain and no pain evoked by compression.
• Compensation (condition yellow): no history of pain, but pain can be provoked repeatedly by passive compressions.
• Decompensation (condition red): history of pain, and individual pains can be provoked by compressions.
The three possible conditions of the tissues are noted in the patient’s chart with color coding:
• All painful symptoms fall under the term capsulitis in the tissue-specific diagnosis.
• “Conditions yellow” are designated as compensated capsulitis
• “Conditions red” are designated as decompensated capsulitis.
Finally, the exact loading vector, which indicates the direction of compression, is added to the diagnosis. For example, a finding of “condition yellow” pain resulting from posterolateral compression would give the diagnosis: decompensated capsulitis with a posterolateral loading vector. In this case, during clarification of the contributing factors (see p. 124) we would look for one or more causes for the posterolateral force on the involved condyle.
• “Condition green” indicates either that the relationships in the bilaminar zone are physiological or that there is perfect adaptation to nonideal conditions. Even if the morphology is completely different from normal, there is no pressing medical indication for treatment. This has been confirmed over the long term through a series of basic studies (Pereira et al. 1996a, b).
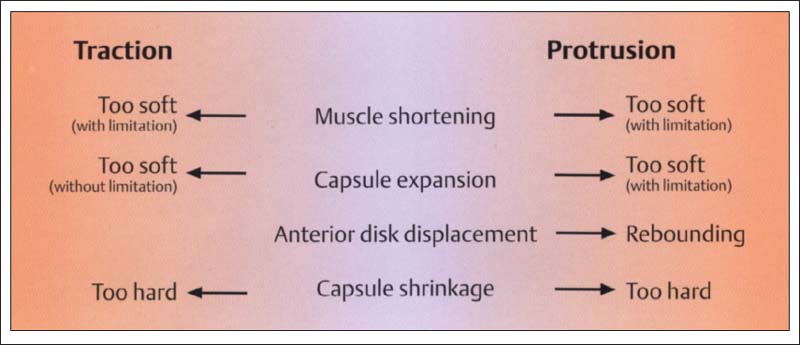
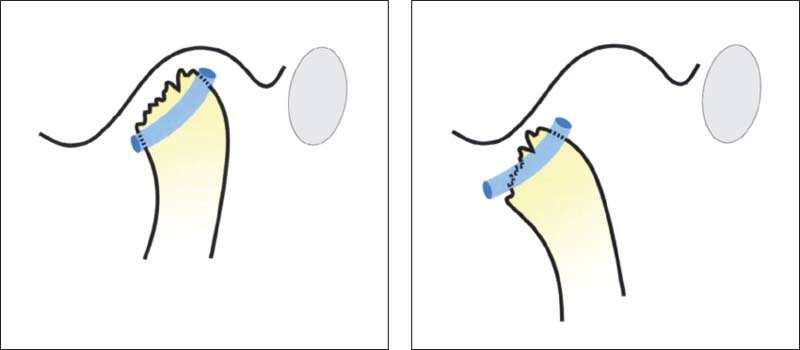
177 Possible endfeels with traction and protrusion
Under physiological conditions the movements of the temporomandibular joint, with the exception of jaw closure, are limited by ligaments and therefore produce a “hard ligamentary endfeel.” A number of structural changes can be responsible for different pathological endfeels. Above all else, muscle shortening and capsule shrinkage have the greatest therapeutic relevance because they can impose restrictions on the treatment.
After the bilaminar zone, the joint capsule and ligaments are tested specifically by means of translation and traction manipulations (Bumann and Groot Landeweer 1996b). These techniques serve on the one hand to determine if pain can be provoked, and on the other hand to evaluate the so-called “endfeel.” There is a relatively high correlation between the findings by various examiners (de Wijer et al. 1995).
The specialized structure of the ligaments with their dense connective tissue and parallel collagen fibers provides high tensile strength (Gay and Miller 1978). Ligaments can be stretched by approximately 5-8% of their original length. This slight elasticity prevents irreversible damage to the ligaments themselves while still effectively limiting condylar movements and thereby protecting much more sensitive structures (Griffin et al. 1975. Sato et al. 1996).
The joint capsule exhibits fewer parallel fibers and is composed of different types of collagen. It is more elastic than the ligaments. The principle of collecting, documenting, and interpreting the signs and symptoms is exactly the same as for the passive compression tests. Pain within the joint capsule occurs only with inflammatory changes and is transmitted to the central nervous system by type-IV receptors (Wyke 1972, 1979; Clark and Wyke 1974). Various neuropeptides such as NA and SP effect the release of prostaglandins, which in turn elevate the sensitivity of the pain receptors (Levine et al. 1986, Lotz et al. 1987).
The endfeel is always tested in anterolateral translation and inferior traction when pain can be elicited in the opposite direction or when the mandible is to be therapeutically repositioned. The endfeel is the tissue resistance that the examiner perceives at the end of a movement. It depends exclusively upon the limiting structures. The physiological endfeel is “hard ligamentary” (Bumann et al. 1993). The possible pathological endfeels and their structural correlations will be discussed in greater detail on the following pages.
The capsule and ligaments can become shortened as the result of recurring inflammation or specific compressive functions (Haldeman 1989). Osteoarthrosis and osteoarthritis are frequently associated with shrinkage and reduced elasticity of the capsule (Stegenga et al. 1993). Hypomobility of the joint capsule, also called functional joint compression, may restrict treatment possibilities. Failure to consider such restrictions makes treatment more difficult and often leads to an unstable result. Capsule hypomobility can also increase muscle activity through the mechanoreceptors within the capsule, and therefore should be ruled out before any prosthetic treatment (Kraus 1994a).
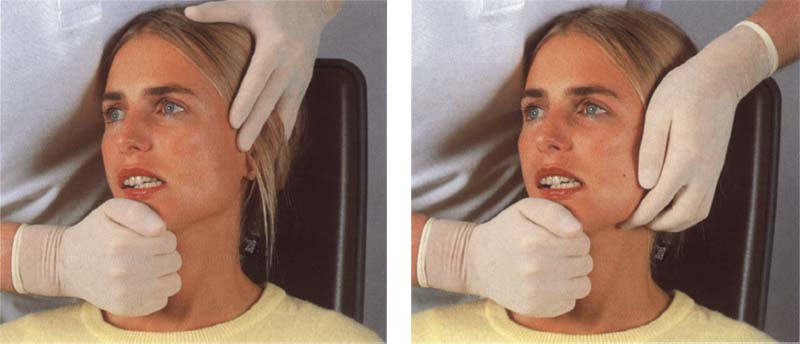
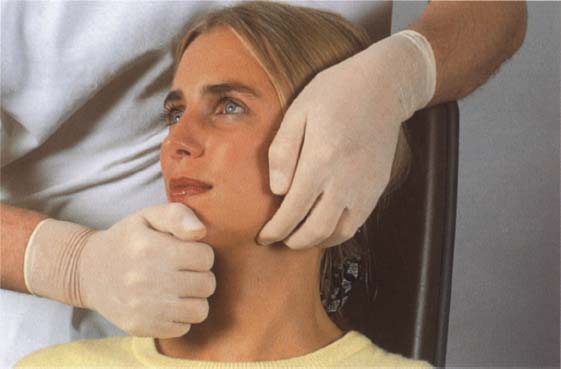
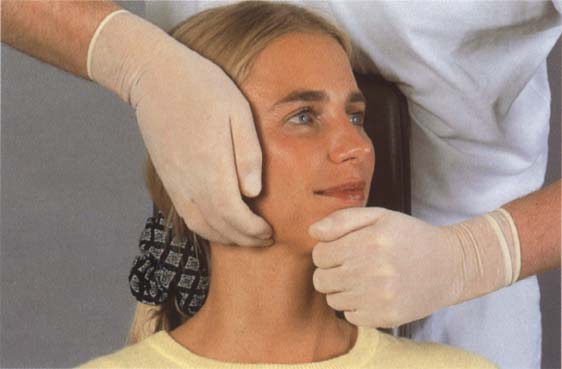
178 Hand grasp for passive compression
Left: The most frequently applied forces during passive compressions have a posteriorly directed component. To test the right temporomandibulcir joint the examiner applies a gradually increasing continuous pressure on the left side of the mental protuberance directed toward the right joint.
Right: To apply a superiorly directed component of force the fingers of the other hand are placed under the horizontal portion of the angle of the jaw.
179 Posterior and posterosuperior compression of the left joint
Left: Application of posterior compression. Even with heavy pressure, this maneuver should not cause pain in a healthy patient. It can reliably demonstrate only inflammatory changes in the posterior direction
Right: For posterosuperior compression the action of the right hand is the same. The addition of an upward component by the left hand results in a posterosuperior loading of the joint.
180 Posterior and posterosuperior compression of the right joint
Left: The left hand is used for posterior compression of the right joint. If the condyle is pushed back too quickly the lateral pterygoid muscle will contract (Gardener 1963). This reflex action is a mechanism to protect the sensitive joint structures.
Right: Posterosuperior compression of the right temporomandibular joint through simultaneous application of force with both hands.
181 Examination form entries for posteriorly directed passive compressions
Right joint: Example of findings In a physiological or fully adapted condition. Left joint: Compensated capsulitis with a posterosuperior loading vector and decompensated capsulitis with a posterior loading vector are recorded. Because of their greater elasticity, joints of females can withstand greater loading than those of males (Loughner et al. 1997).

182 Starting jaw positions for posterior and posterolateral compressions
Left: The starting position for the previous passive compressions was with the mandible retruded and no tooth contact.
Right: For the following two compressions the patient assumes a position of maximal laterotrusion. This movement takes place with no forced guidance by the examiner. Force is applied only after the patient’s jaw is in the starting position
183 Posterolateral and posterosuperior compression of the left joint
Left: On the part of the examiner the same technique is used for the posterolateral compression as was used for the posterior compression. But because of the different starting position, the posterolateral portion of the joint is now being tested.
Right: During the posterosuperolateral compression the patient is responsible for the lateral starting position and the examiner for the posterior and superior components of force.
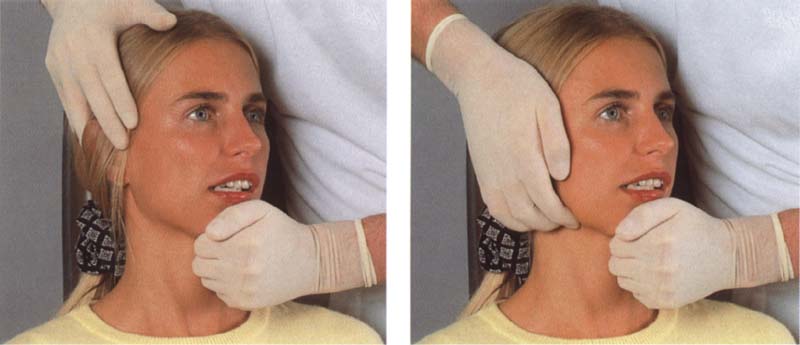
184 Posterolateral and posterosuperolateral compression of the right joint
Left: The right temporomandibular joint is examined in a similar manner, except that the posterior force is now exerted by the left hand while the patient holds the mandible in the maximal laterotrusive position for the right condyle.
Right: Posterosuperior compression of the right joint to evaluate the state of adaptation of the structures in this loading direction.
185 Chart entries for passive posterolateral and posterosuperolateral compressions
These sample entries indicate that the right joint is in either a normal or a completely adapted condition, in the left joint a compensated capsulitis with a posterosuperolateral loading vector has been diagnosed.
Clinical Significance of Compressions in the Superior Direction
The passive superiorly directed compressions (superior, laterosuperior, and mediosuperior) are especially important, not only for routine examinations but also for patients in pain, as they test the state of adaptation of the bilaminar zone in the superior portion of the joint. Positive findings always indicate a nonphysiological disk position. Because normally the pars posterior of the disk lies on the superior part of the condyle, which is not innervated, a correctly performed superior compression should not produce pain. But in cases with anterior disk displacement, the structures of the bilaminar zone lie over the superior part of the condyle when the teeth are in habitual occlusion. Unless the bilaminar zone is adapted (= fibrosed), superior compressions will provoke a painful response. Long-term clinical studies (de Leeuw 1994) plainly show that nonsurgical treatment is quite successful if the tissues are sufficiently adaptable. Therefore, clinical testing of the capacity of the individual patient’s bilaminar zone to adapt is especially important in cases of disk displacement. The results of these tests carry a great deal of weight in deciding which therapeutic measures are indicated.
186 Reducing disk displacement with an adapted bilaminar zone
When the results of the superior compression tests are “green,” either conditions in the superior portion of the joint are physiological or the bilaminar zone is well adapted. In either case there is no pressing need for treatment.
Right: MRI of a 17-year-old with anterior disk displacement and good adaptation in the cranial portion of the bilaminar zone, seen here as a dark gray signal (arrows).
187 Tendency for anterior disk displacement
When there is a tendency for anterior disk displacement there will still be contact between the pars posterior of the disk and the anterior contour of the condyle. At this stage no clicking sounds can yet be detected. The superior portion of the bilaminarzone may be adapted, compensated, or decompensated. This example indicates laterosuperior (LS) and superior (S) decompensation and mediosuperior (MS) adaptation.
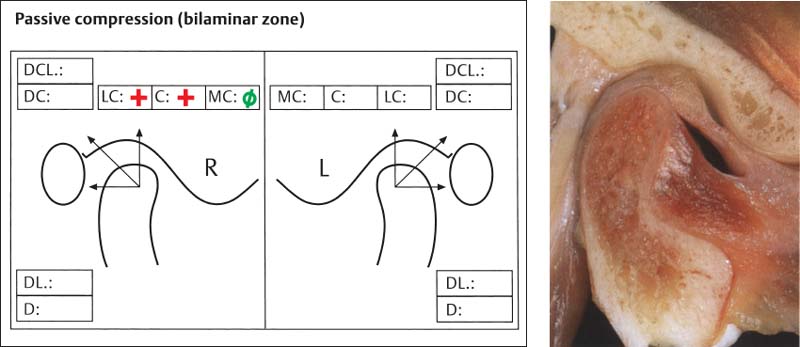
Right: Macroscopic view of a joint with a tendency for anterior disk displacement.
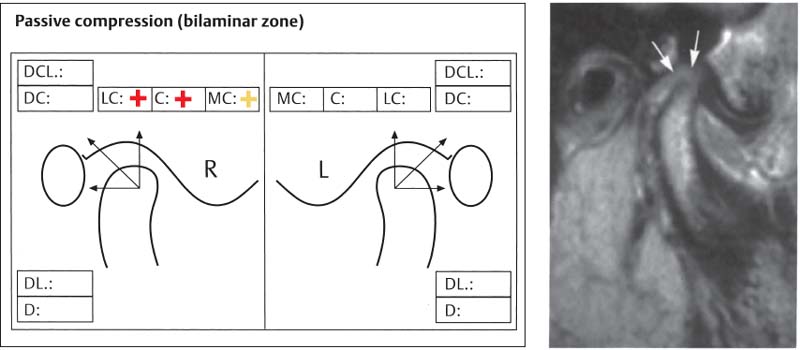
188 Nonreducing disk displacement
Findings in the superior portion of the joint of a 22-year-old patient with nonreducing disk displacement. The bilaminar zone has not adapted in any of the three directions. There is a compensated capsulitis with a mediosuperior loading vector and a decompensated capsulitis with superior and laterasuperior loading vectors.
Right: Anterior disk displacement in a MRI. The light-gray region indicates that there is no adaptation of the bilaminarzone (arrows).
189 Hand grasp for superior compression
One hand is again placed under the horizontal part of the angle of the mandible. Great care must be taken to ensure that the force is applied exactly in the superior direction. Otherwise, false positive results could be obtained.
Left: An important condition for an efficient superior compression is the maintenance of an interocclusal distance. For this reason the examiner exerts a light downward pressure on the patient’s chin with a thumb.
190 Superior compression of the left joint
The examiner’s right hand helps prevent tooth contact while the left applies superiorly directed compression with a steadily increasing force. This test is never painful if the joint surfaces are healthy. If there is a painful response the technique should be repeated in a slightly protruded position. Only if pain can be repeatedly provoked in both positions is the code “yellow” or “red” entered in the chart.
191 Superior compression of the right joint
During superior compression of the right joint the examiner’s left hand prevents tooth contact while the right hand applies a superiorly directed pressure. Pain indicates a nonadapted part of the bilaminar zone and a nonphysiological spatial relationship between disk and condyle. The possible diagnoses (tendency for disk displacement, reducing disk displacement, nonreducing disk displacement) have far-reaching implications for the treatment
192 Examination form
An example of entries of findings from superior compression. In different jaw positions a diagnosis was made of a compensated capsulitis with superior loading vector on the right side and a decompensated capsulitis with superior loading vector on the left side. In these cases the endfeel of inferior traction must always be tested to determine whether a constricted capsule is also present. If so, this would intensify the loading vector and make any relaxation therapy more difficult.
193 Hand grasp for medial and mediosuperior loading
Left: To apply the medial component of force the examiner places one hand flat against the back of the patient’s neck and, with the thumb of the same hand, exerts a medially directed pressure against a broad area over the angle of the jaw. Here this results in medial translation of the right condyle and lateral translation of the left.
Right: To produce mediosuperior compression a superior component of force is added with the other hand.
194 Mediosuperior compression right and left
Left: For mediosuperior compression of the right joint the medial component of force is provided by the examiner’s right hand and the superior component by the left hand. This allows evaluation of the medial portion of the bilaminar zone.
Right: Mediosuperior compression of the left joint is accomplished by reversing the procedure, in this way the medial portion of the bilaminar zone in the left joint is tested.
195 Medial translation of the right and left condyles
Left: The superior component of force is omitted for medial translation. This technique produces bodily movement of the right condyle directly toward the median plane with no mediotrusive movement! Only responses from the joint on the same side are recorded as no conclusions can be made about the contralateral side.
Right: Medial translation of the left condyle is accomplished by the examiner’s left hand. Pressure is exerted by the thumb over a broad area of the angle of the jaw.
196 Examination form
The results of the mediosuperior compression tests are entered under the heading “Passive compresston” and those of the medial translation tests under “Traction and translation.” The sample record form indicates a compensated capsulitis with a mediosuperior loading vector on the right and a decompensated capsulitis with a mediosuperior loading vector on the left. In addition there is a compensated capsulitis with a medial loading vector on the right and a decompensated capsulitis with a medial loading vector on the left.
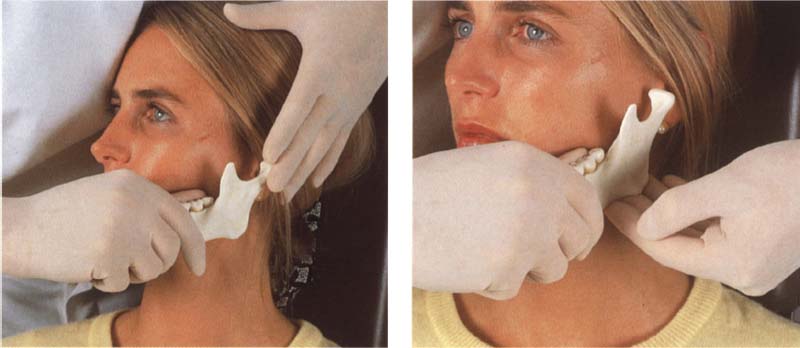
197 Hand grasp for lateral and laterosuperior loading
Left: The lateral component of force can be provided either by pressing inward on the angle of the jaw on the opposite side or by pressing laterally against the lingual surfaces of the molars on the side being tested. The latter method is more effective for monitoring the amount of translating movement through tactile sensation.
Right: The superior component of force is again maintained by pressure under the angle of the mandible.
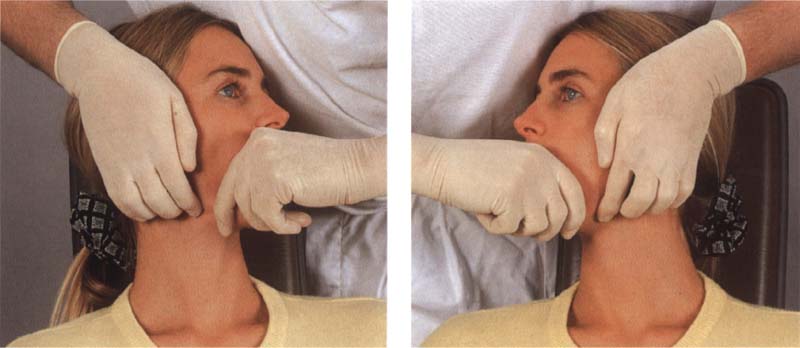
198 Laterosuperior compression right and left
Left: During laterosuperior compression of the right joint the lateral component of force is exerted by the examiner’s left hand and the superior component by the right hand. In this way the lateral portions of the bilaminar zone can be examined.
Right: The procedure is fully reversed for laterosuperior compression of the left joint. This allows evaluation of the lateral portions of the bilaminar zone in the left joint.
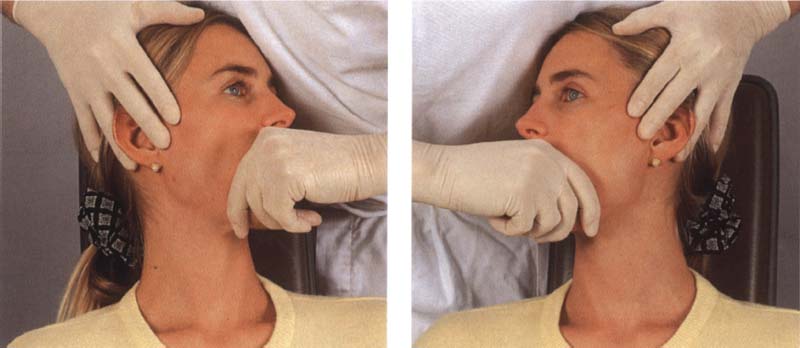
199 Lateral translation right and left
Left: For the lateral translations the superior component of force is omitted. With this technique there is movement of the right condyle toward the right side with no laterotrusive movement! Results are noted for the right side only and no conclusions can be formed about the contralateral side.
Right: The mandible is moved bodily to the left by the examiner’s right hand.
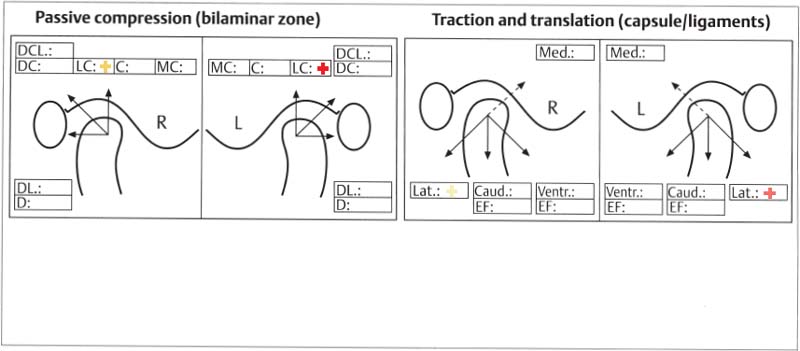
200 Examination form
This example of a record form shows a compensated capsulitis with a laterosuperior loading vector on the right side and a decompensated capsulitis with a laterosuperior loading vector on the left. Under traction and translation there is also a compensated capsulitis with a lateral loading vector on the right and a decompensated capsulitis with a lateral loading vector on the left. An examination is always completed on one of the joints before the other side is examined.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


