Treatment of the mandible fracture is basic to the treatment of maxillofacial trauma. Successful treatment of the mandible fracture results in an anatomic bony union with restoration of normal occlusion and function. Although there is universal agreement as to the basic therapeutic principles of reduction and stabilization, a plethora of currently accepted treatment modalities indicates a lack of consensus.
History
Suggested treatment of mandible fractures has evolved significantly over the last three decades. Two open reduction techniques, rigid internal fixation (RIF) and adaptive miniplate fixation, have replaced the use of wire osteosynthesis and prolonged maxillomandibular fixation (MMF). The advantages of both RIF and miniplate fixation with minimum periods of MMF include early mobilization and restoration of jaw function, airway control, nutritional status, improved speech, better oral hygiene, patient comfort, and an earlier return to work.
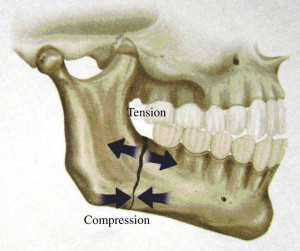
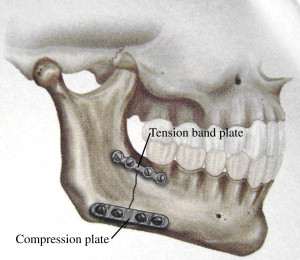
Principles and techniques of RIF were developed and popularized as a result of the research conducted by the Arbeitsgemeinschaft fur Osteosynthesefragen (AO/ASIF) in Europe in the 1970s. The basic principles of the AO were outlined by Spiessl and call for primary bone healing under conditions of absolute stability. Rigid internal fixation must neutralize all forces—tension, compression, torsion, shearing—developed during functional loading of the mandible to allow for immediate function without MMF ( Fig. 1 ). This is accomplished by interfragmentary compression at the mandibular angle by application of a dynamic compression plate (DCP) or reconstruction plate to counter compression at the inferior border, and a smaller tension band plate at the superior border of the mandible to counter tensile forces ( Fig. 2 ).
There are several disadvantages to this method of open reduction, internal fixation (ORIF) of mandible fractures that is usually performed transcutaneously, including increased operating room time, risk of facial nerve paresis, and risk of hypertrophic scar formation. Of perhaps greater significance is the reported high infection rate, ranging from 6% to 32%, associated with this technique. That RIF of mandible fractures is highly technique-sensitive and demanding is confirmed by Assael’s report of a 24% complication rate during in vitro application of plates in a RIF laboratory study.
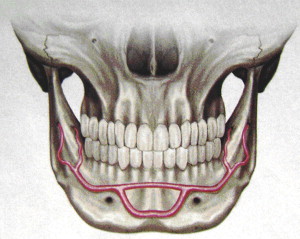
At approximately the same time that Spiessl was expounding the AO doctrine, Michelet and colleagues and Champy and colleagues in France were developing the concept of adaptive miniplate osteosynthesis. Champy advocated transoral placement of small, thin, malleable stainless steel miniplates with monocortical screws along an ideal osteosynthesis line of the mandible ( Fig. 3 ). Champy and Lodde and colleagues presented biomechanical investigations that sought to confirm the concept of a functionally oriented miniplate adaptation and fixation. Miniplates achieve the goal of osteosynthesis by neutralizing undesirable tensile forces while retaining favorable compression forces during function. Champy believed that compression plates were unnecessary because of masticatory forces that produced a natural strain of compression along the inferior border of the mandible.
The advantages of adaptive miniplate fixation of mandible fractures are numerous: transoral procedure without risk of facial nerve paresis or hypertrophic scar, decreased operating time, ease of adaptation of miniplates, ability to confirm occlusion during the procedure, and early mobilization of the patient. Miniplates are less palpable because of their lower profile than DCPs, and less thermal sensitivity is reported by the patient.
There are limitations to the use of miniplates in the treatment of mandible fractures. They are not as rigid as DCP or reconstruction plates, which may lead to torsional movements of the fracture segments under functional loading. Therefore, miniplate fixation should be avoided in comminuted or infected fractures, or those fractures without adequate bone buttressing. In these cases, a load-bearing fixation device (DCP or reconstruction plate) is indicated, rather than the load-sharing miniplate.
Several studies have been conducted by Ellis and others in the use of adaptive miniplate fixation of mandible fractures without postoperative MMF. Complication rates range from 16% to 28%. Therefore, a brief period of postoperative MMF is recommended to reinforce the tension band, allow reattachment of the soft tissue drape, and stabilize the occlusion.
Evolution of Kings County Hospital fracture protocol
In the 15 years from 1992 to 2007, the Oral and Maxillofacial Surgery Service at Kings County Hospital/SUNY Brooklyn has treated 2,311 mandible fractures in 1,490 patients. Of these, 54 cases required reoperation or readmission, for an overall complication rate of 2.4%. Bone healing was satisfactory in 99% of cases. The hospital continues to evolve our mandible fracture protocol to remain efficient and cost effective.
From 1993 to 1998, four prospective DCP clinical trials were conducted at Kings County Hospital/SUNY Brooklyn. All four trials involved a transcutaneous extraoral approach for ORIF of mandible fractures. Results of all four clinical trials were presented at successive Poster Sessions of the American Association of Oral and Maxillofacial Surgeons Annual Meetings. In 1993, a 2.7-mm DCP system with 3 weeks of MMF was studied; a 1% infection rate that required plate removal and a 99% satisfactory bone healing was cited. In the second study in 1994, a 2.7-mm DCP with 2 weeks of MMF yielded a 1.8% infection rate and 98.2% bone healing. In the third study in 1995, a lower profile 2.3-mm DCP with 2 weeks of MMF was used; one complication of a fibrous union (3.3%) and 96.7% bone healing were noted. In 1998, the fourth study investigated the 2.3-mm DCP with 1 week of MMF; four complications (12%) and a 96.7% bone healing rate were documented.
With the increasing interest in adaptive miniplate fixation of mandible fractures, investigators at Kings County Hospital/SUNY Brooklyn conducted a prospective clinical trial of transoral 2.0-mm miniplate fixation of mandible fractures plus 2 weeks MMF. The results of this miniplate study were published in the Journal of Oral and Maxillofacial Surgery (JOMS), 2002. In this study, 44 mandible fractures in 31 subjects were treated via a transoral 2.0-mm nonlocking miniplate placed along Champy’s line of ideal osteosynthesis plus 2 weeks of MMF. The results of this data showed two minor complications of intraoral wound dehiscence(4.52%) and 100% satisfactory bone healing.
With the advancement of the more stable construct of the 2.0-mm locking miniplate (LMP) system (Synthes Maxillofacial, Paoli, PA) ( Fig. 4 ), the authors postulated that they could reduce the period of postoperative MMF from 2 weeks to 1 week. From 2002 to 2004, the authors treated 50 mandible fractures in 34 patients with the 2.0-mm LMP plus 1 week MMF (published in JOMS, 2005). Three complications (6%) were observed: a wound dehiscence that required local wound care and oral antibiotics, a minor malocclusion that required occlusal adjustment, and a fibrous nonunion that required three additional weeks of MMF. Primary bone healing was achieved in 98% of cases. The fibrous nonunion was a result of poor case selection in a bilateral flailed mandible fracture without adequate bone buttressing. This complication could have been prevented by the use of a load-bearing fixation device (DCP or reconstruction plate) rather than the load-sharing LMP.
At Kings County Hospital/SUNY Brooklyn the authors have continued their transoral 2.0-mm LMP plus 1 week MMF prospective clinical trial from 2004 to 2008 ( Table 1 ). In this secondary phase of the study, the authors have treated 159 mandible fractures in 93 subjects; 92 angle fractures were included in this cohort. Exclusions included condylar fractures that required 2 weeks MMF, comminuted or infected fractures, and subjects in whom a brief period of MMF was medically contraindicated (epilepsy, severe asthma, psychiatric condition). Subjects were observed for complications: plate dehiscence, soft tissue infection, nonunion, malunion, malocclusion, osteomyelitis, osteolysis of plate or screws, iatrogenic nerve injury, tooth damage. All subjects were followed for at least 6 weeks until removal of arch bars with biweekly panoramic radiographs.



