Edentulous or atrophic mandible fractures are rare and potentially problematic for the oral and maxillofacial surgeon. With the loss of teeth, atrophy of the alveolar bony apparatus ensues, creating a mandible more prone to fracture. This article describes the management of edentulous/atrophic mandibular fractures.
Edentulous or atrophic mandible fractures are rare and potentially problematic for the oral and maxillofacial surgeon. With the loss of teeth, atrophy of the alveolar bony apparatus ensues, creating a mandible more prone to fracture. Approximately 8% of the American population is considered completely edentulous . Most of these patients are elderly, although in certain states (Kentucky, Louisiana, and West Virginia) the incidence of edentulism is significantly higher (West Virginia has a 40% edentulism rate) . As a result, edentulous/atrophic mandible fractures may be seen in the nonelderly as well. In addition, the American population is growing older—US Census data noted that people older than 65 years will represent 13.6% of the American population; people older than 80 will represent 6.2% of the population in 2004 .
Tooth-bearing alveolar bone is stimulated to maintain its quality and quantity of bone secondary to the occlusal forces/load generated by the teeth. Loss of teeth results in a loss of this stimulus, leading to a loss of bone volume—atrophy. It is this decrease in bone volume that makes the atrophic mandible less resistant to traumatic forces, and more prone to fracture.
Overall, the incidence of atrophic mandible fractures is rare compared with other types of facial fractures. A recent study of mandible fractures over a 17-year period at an urban level-one trauma center revealed an average of 2 atrophic mandible fractures per year out of 200 total mandible fractures, or 1% . Another study by Mugino and colleagues noted 11 (3%) of 335 fractures were edentulous/atrophic. In addition, most of these patients were elderly with comorbid diseases, most commonly hypertension, diabetes, and coronary artery disease, which in turn made medical and surgical management more complicated. The elderly also have delayed bone regeneration, and atrophic bone is often sclerotic with a compromised blood supply.
Luhr and colleagues developed a classification for fractured atrophic mandibles, based on bone height at the fracture site. A fracture in bone of less than 20 mm of height is considered atrophic. Class I fractures are those fractures in which the bone height is 16 to 20 mm, Class II fractures are 11 to 15 mm in height, and Class III fractures are less than 10 mm in height ( Table 1 ).
| Class | Mandible height at fracture site |
|---|---|
| I | 16–20 mm |
| II | 11–15 mm |
| III | <10 mm |
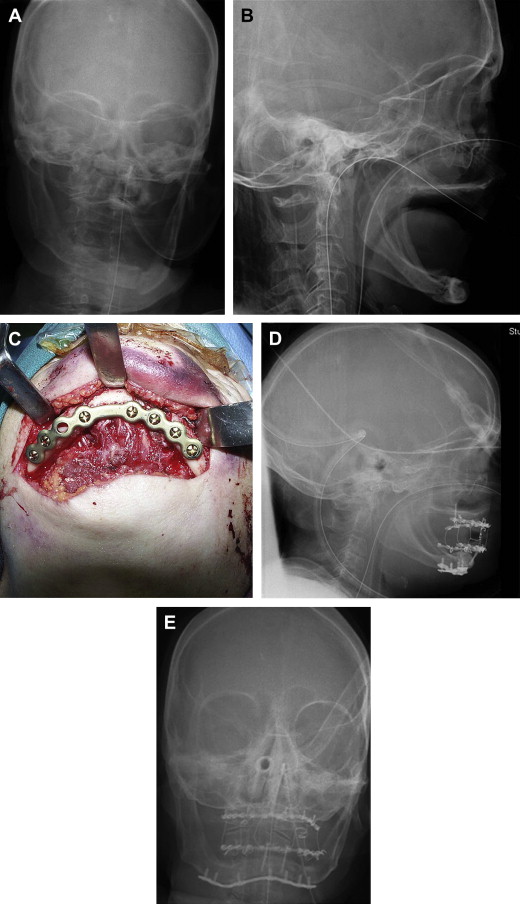
There remains some controversy in treating the edentulous/atrophic mandible fracture. Many surgeons advocate conservative closed treatment, while others advocate more aggressive open reduction of these fractures. The crux of this debate centers on the concerns over comorbid disease in the elderly patient resulting in an increased general anesthesia risk as well as the compromised vascular supply of the atrophic jaw bone . Obviously, patients who are deemed by an anesthesiologist to be a poor candidate for general anesthesia require closed reduction of the fracture via the use of existing dentures or Gunning splints; in situations where the patient is too unstable and the fracture posses no airway threat, no treatment may be an option. On the other hand, advances in trauma care and anesthetic management have decreased the risk of surgery in the elderly ( Fig. 1 ).
The controversy regarding the quality of blood supply to the atrophic mandible stems from a 1975 article by Bradley . Using angiography, he documented that the inferior alveolar artery provided inconsistent supply to the atrophic mandible. As such, he felt that the primary blood supply in the atrophic mandible arises from the periosteum. He wrote that “elevation of the periosteum … may seriously impair the vascular supply to the bone resulting in nonunion of fractures treated by open reduction and direct osseous fixation .” Multiple studies in the past 15 years, however, have shown that open reduction does not increase the incidence of nonunion in atrophic fractures. In fact, many authors have advocated open reduction of atrophic mandible fractures as superior to closed techniques, because open reduction provides direct visualization and rigid fixation provides stability. In addition, these same studies have shown that a supraperiosteal dissection provides no significant advantage in healing compared with subperiosteal dissection.
There has been further discussion in the literature about an intraoral versus extraoral approach to open reduction. Advantages of an intraoral approach primarily focus on the ease and speed of dissection and closure. Disadvantages of the intraoral approach include salivary contamination and visualization difficulties. In addition, in some cases, the mandibular neurovascular bundle/mental foramen may actually lie close to the crest of the alveolar ridge in a severely atrophic fracture; an intraoral incision may inadvertently traumatize this nerve.
An extraoral route has the advantage of providing for excellent visualization and manipulation of the fracture as well as ease of hardware application. Disadvantages include a facial scar and risk to the facial nerve; however, often in the elderly the scar can be hidden in a well-placed incision in a facial rhytid. Ultimately, the approach to access the fracture must be tailored to the patient’s case. The approach selected must allow the surgeon to adequately visualize the fracture easily and allow for easy hardware application. Although this is true in all facial fracture open reductions, this principle is more important in treating the edentulous/atrophic mandible fracture. Stabilizing the occlusion via maxillo-mandibular fixation often reduces the fracture before placing rigid fixation plates. In the edentulous fracture, an anatomic reduction is necessary, as there is no occlusal guidance. This requires the surgeon to reduce the fracture manually, which requires excellent unhampered access.
As rigid fixation has evolved over the past several years, multiple authors have suggested different protocols for rigid fixation of the edentulous/atrophic mandible. Wittwer and colleagues noted in a recent study that the treatment of atrophic mandibular fractures should be based on the degree of atrophy. They found that Luhr Class I and Class II mandibles had a much higher incidence of complications, including hardware failure, infection, or nonunion. In their review of 36 atrophic fracture patients, they concluded that more rigid fixation is indicated in mandibles with atrophy of 15 mm on bone height or less. In addition, whereas some studies have advocated using the smallest plate available in treating these fractures , the current recommendations include using larger plates. Ellis noted that rigid fixation bone plates in edentulous mandibles are subjected to repeated muscle loading as well as deformation . As a result, these plates will often fracture. In addition, the bone along the fracture line in an atrophic mandible does not share any of the occlusal load; most of the load is placed on the bone plate.
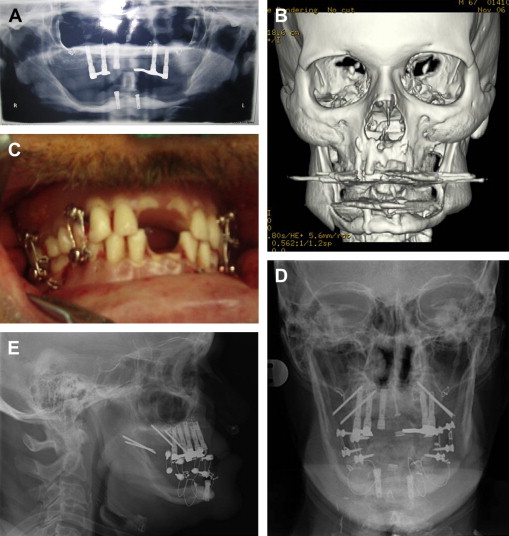
As such, larger bone plates are advocated. Locking plating systems provided plates with greater stability as well as easier plate adaptation. Currently available are 2.0-mm, 2.3-mm, 2.4-mm, and 2.7-mm locking plate systems. The 2.0 locking system is an excellent option in rigidly fixating the atrophic fracture: it is easily adapted, provides excellent stability across the fracture, and has significant increased strength compared with a conventional 2.0 miniplate. Ellis recommended this plate with six holes, three bicortical screws on either side of the fracture, located at the inferior border of the jaw, to provide strong and stable reduction . Although this plate is exceedingly small, another advantage is its lower profile, compared with larger-caliber plates, allowing for easier closure and more comfort in wearing dentures ( Fig. 2 ). Immediate bone grafting at time of repair of the atrophic mandible fracture has historically been advocated in the literature, often in situations where there was a nonunion of the fracture and the bone was used as a method of fixation. This provided the fracture with fixation as well as promoted fracture healing by providing osteocompetent cells to the fracture site. With the advent of rigid fixation, bone grafting is often not indicated. However, bone grafting is still used in the situation of continuity defects or to add alveolar height to a severely atrophic fracture. This additional bone height is hoped to facilitate dental reconstruction post fracture repair. Ultimately, bone grafting as part of the repair of the atrophic fracture should be limited to situations in which a continuity defect requires reconstruction, there is a possibility of prosthetic rehabilitation, and the donor site (rib or ileum) has minimal morbidity associated in an elderly patient ( Fig. 3 ).