Dental implant surgery has become the standard of care for reconstruction of simple and complex edentulous areas of the maxilla and mandible. The risks of injury to the branches of the mandibular division (MdN) of the trigeminal nerve (inferior alveolar nerve [IAN], lingual nerve [LN], and mental nerve [MN]) are known complications of implant restoration of the posterior mandible. The use of advanced imaging modalities such as cone beam computed tomography (CT) scans and high-definition panoramic radiographs can assist in localization of the inferior alveolar canal (IAC). However, despite correct planning, the possibility of injury to the MdN is not entirely eliminated. Sensory dysfunction, especially if persistent or painful, can be distressing to both the patient and the clinician. Altered sensation after implant surgery continues to bear medicolegal implications that further warrant the implantologist’s attention. In the treatment of nerve injuries associated with dental implant surgery it is most important that there be prompt recognition and acknowledgment of the patient’s sensory complaints and timely decisions regarding management to maximize the recovery of nerve function. The clinician is faced with 2 problems: (1) treatment of the neurosensory disturbance (NSD) of the affected region, and (2) how best to proceed with dental restoration of the affected area. Such patients are frequently distressed and disappointed in their treatment outcome. Their concerns are best addressed by a continuing supportive relationship with, and appropriate recommendations for further treatment from, their implantologist.
This article presents the causes and management of injuries to the MdN of the trigeminal nerve from dental implant surgery.
Causes and pathogenesis
The 4 most frequent causes of injury to the MdN related to dental implant surgery are errors in evaluation and planning, the injection of local anesthetic for the implant procedure, the bone preparation (drilling), and placement of the implant. Other reasons for nerve injury are also discussed.
Errors in Radiographic Planning
The panoramic radiograph is useful as the primary imaging study to assess the vertical distance from the crest of the mandibular alveolar ridge to the superior aspect of the IAC. The panoramic machine should be calibrated for distortion or magnification to allow accurate determination of dimensions from panoramic films. If the panoramic film shows inadequate distance from the alveolar crest to the IAC to support an implant cylinder, the mediolateral position of the IAC needs to be determined to decide whether an implant can be placed without repositioning of the IAN or MN (see later discussion). In such patients, a CT scan is a necessary part of the evaluation.
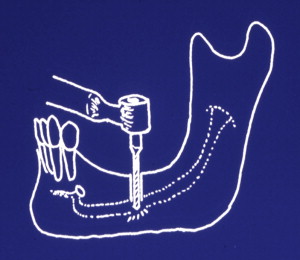
Regardless of the radiographic modality (CT or panoramic radiograph) used for implant planning, errors in interpretation and application of the radiograph can lead to unplanned implant positioning. The CT scans have improved resolution and allow visualization of the nerve in 3 dimensions. However, errors of software planning can be translated into the surgical procedure. Attention should be given to the accuracy of the surgical guides and their seating onto the alveolar ridge. Placement of the surgical guide on a totally edentulous mandible will have a significant inherent margin of error related to the soft tissue despite correct planning. It is important to allow an additional reasonable distance (ie, 2–3 mm) from the nerve during the CT planning to accommodate this margin of error. Although the use of flap-less surgery ( Fig. 1 ) for implant placement using navigation guides is becoming popular, the surgeon should not hesitate to raise a mucoperiosteal flap to better visualize and confirm anatomic landmarks as needed.

Injection of Local Anesthetic
The IAN or LN can be injured secondary to the injection of a local anesthetic into the pterygomandibular space or the MN when injecting in the area of the mental foramen. Although the exact pathophysiology of this injury remains unknown, there are 3 possible causes: (1) direct intraneural injection with mechanical injury to the nerve (ie, severance of axons, partial or total, scar tissue or neuroma formation, Wallerian degeneration, and so forth), (2) interruption of vessels of the mesoneurium with peri- and intraneural hemorrhage and secondary scar formation, and (3) chemical toxicity of the anesthetic solution from a contaminant (sterilizing solution) in a leaky carpule. Regardless of its cause, it is recommended that aspiration be done before all local anesthetic injections. If there is a bloody aspirate or the patient complains of a paresthesia (typically, an electric shock-like sensation), the needle is withdrawn a few millimeters and aspiration is repeated. If there is now no bloody aspirate, it can be assumed that the needle tip is no longer in contact with a blood vessel or nerve, and the injection is completed. A note of such an occurrence should be routinely entered in the patient’s chart. This technique may prevent direct injection into a vascular space, but does not necessarily prevent deposition of the anesthetic within the epineurium (the diameter of the IAN is 4–5 times greater than the associated inferior alveolar artery or vein). Nerve injury secondary to local anesthetic injection, although uncommon, has a reported incidence of 1:26,762 to 1:160,571. It can be difficult to differentiate from injury related to the placement of the dental implants, especially if the patient was under sedation or general anesthesia and, therefore, unable to report a paresthesia at the time of the injection(s). Without obvious clinical or radiographic signs of injury to the nerve, the possibility of needle injection injury cannot be eliminated. Unfortunately, a very small percentage of patients who have suffered an injection-related injury can be misdiagnosed with injury related to the dental implant surgery, and subsequently undergo diagnostic or exploratory surgical procedures that reveal no visible nerve injury at the implant location.
Bone Preparation
Injury to the IAN as a consequence of bone preparation or implant placement can be caused by errors in radiographic planning, drilling, or direct contact of the implant with the nerve.
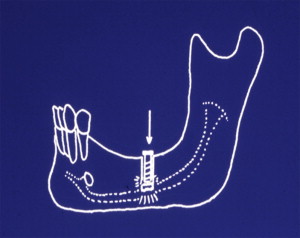
Drill injuries to the IAN can be difficult to diagnose. Despite correct position of the implant vis-à-vis the IAC on the postoperative radiograph appearance of the implant, osseous preparation with the drill may have been performed beyond the planned implant depth causing injury to the nerve ( Fig. 2 ). This error can be prevented by correct radiographic measurement of the distance from the alveolar ridge crest to the superior aspect of the IAC, the use of drilling equipment with predetermined depth stops, and careful technique to prevent drilling beyond the planned depth. Irrigation with adequate coolant to dispel heat generated by bone drilling may also prevent a thermal injury in the absence of direct contact with the nerve. Frequent intraoperative reverification of the drill dimensions (diameter and length) is also helpful.
Implant Placement (Direct Implant Injury)
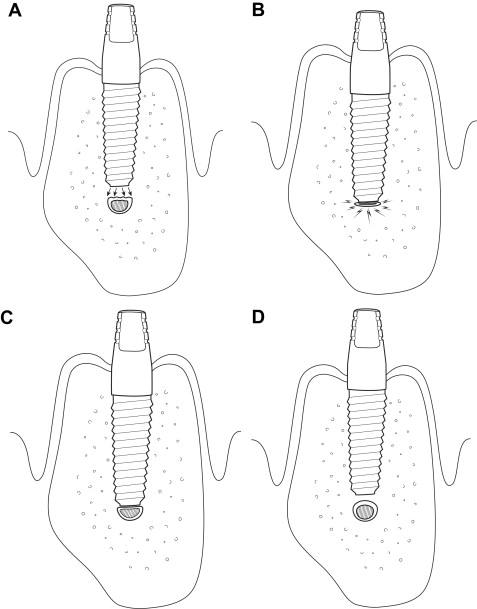
In addition to injury caused by drilling, the extent of injury of the IAN caused by the implant itself is related to the degree of encroachment of the implant into the IAC or its direct contact with the IAN ( Fig. 3 ). Nerve injury caused by implant placement may occur, despite correct osseous preparation, when the implant is inserted beyond the vertical confines of the prepared bone, compressing or breaching the superior wall of the IAC and forcing bone into the canal ( Fig. 4 A). Alternately, extension of drilling into the IAC may facilitate over insertion of the implant cylinder beyond its intended depth and into the IAC, making direct contact with the IAN (see Fig. 4 B, C). Delayed osseous healing and remodeling from localized injury can cause excess bone formation and compromise of the IAC cross-sectional diameter (see Fig. 4 D).
Other Causes of Injury
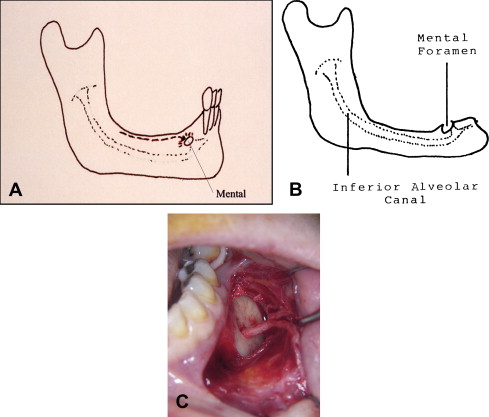
The MN lies in the mandibular buccal soft tissue and is at risk of injury during incisions. Recognition of the changing anatomy of the edentulous mandible is particularly helpful in minimizing risk of injury to the MN. As the patient ages, the alveolar bone in an edentulous area resorbs, and the position of the mental foramen becomes closer to the crest of the alveolar ridge ( Fig. 5 A). In some patients there is actual dehiscence of the IAC, and the IAN and the MN come to lie on the alveolar ridge crest (see Fig. 5 B). Placement of an incision must, therefore, take these anatomic changes into consideration. During the retraction of a mucoperiosteal flap it is possible to exert continuous undue pressure on the underlying MN. Gentle soft tissue retraction with frequent brief relaxation of retraction pressure is suggested (see Fig. 5 C).
Less common causes of nerve injury are related to placement of bone grafts (autologous, allogenic, xenogenic) during simultaneous implant placement. In cases of complex implant reconstruction, the bone graft material may be placed into the donor site with excessive force, thus severely compressing or even crushing the IAN. The authors have encountered several cases of particulate bone graft material within the IAC that caused significant nerve compression, and other cases of severe scarring, similar in clinical appearance to a chemical burn, when calcium hydroxyapatite came in direct contact with the nerve.
Evaluation of nerve injuries
Neurosensory disturbances are evaluated and documented in a standard fashion using the Medical Research Council Scale (MRCS) guidelines, as modified for the oral and maxillofacial regions, regardless of the cause of the sensory nerve injury. The evaluation of nerve injuries is discussed in a separate article by Meyer and Bagheri elsewhere in this issue.
Evaluation of nerve injuries
Neurosensory disturbances are evaluated and documented in a standard fashion using the Medical Research Council Scale (MRCS) guidelines, as modified for the oral and maxillofacial regions, regardless of the cause of the sensory nerve injury. The evaluation of nerve injuries is discussed in a separate article by Meyer and Bagheri elsewhere in this issue.
Treatment
Timely repair of peripheral nerve injuries has always been the sine qua non for successful recovery of nerve function, especially since Seddon’s extensive experience with treatment of missile injuries to extremities during and after World War II. His comment, “If a purely expectant policy is pursued, the most favorable time for operative intervention will always be missed…” is as pertinent today as it was more than 60 years ago. As in all other causes of nerve injury, treatment of the patient with a dental implant-associated nerve injury is dependent on the correct diagnosis of the injury and its timely management.
The perioperative administration of supportive medications has been advocated for patients undergoing procedures such as dental implants, mandibular osteotomies, and removal of lower third molars, which are associated with a risk of nerve injury. There is conflict in the literature between those who recommend beginning corticosteroids preoperatively and others who advise waiting postoperatively for several days before initiating administration. Many surgeons routinely give a single preoperative intravenous dose of a steroid (dexamethasone or hydrocortisone). Whether or not it is beneficial to initiate corticosteroid or antiinflammatory medications after a nerve injury has occurred is questionable. Previous studies have documented the lack of benefit of corticosteroids administered to reduce cerebral edema in patients who have sustained head injuries. That the IAN, in a similar closed box situation, confined within the IAC, could benefit from retroactively administered corticosteroid seems unlikely.
Our algorithm for the management of nerve injuries from dental implant surgery is shown in Fig. 6 . The patient who complains of decreased or painful sensation following placement of dental implants should be requested to return to the office for evaluation. In some patients a nerve injury might have been suspected, if the patient complained of paresthesia during local anesthetic injection or during the bone drilling preparation for implant placement. In most cases, however, the patient is under intravenous sedation, and there is no indication during the procedure of a nerve injury. It is recommended that the patient be seen as soon as is convenient, preferably within 24 hours or the same day, if painful sensation is the chief complaint, so that adequate pain control can be established and rapport with the patient maintained. The exact nature of the patient’s complaints should be ascertained (see article on evaluation by Meyer and Bagheri elsewhere in this issue). A general oral examination is performed to assess the healing status of the surgical site. Neurosensory testing (NST) is done to establish an objective baseline determination of the level of sensory dysfunction for further follow-up, as indicated.




