
Fig. 26.1a,b.
In the area of the anterior nasal spine, sufficient space must be created underneath the pontics. This bone area is quite resistant to resorption, and in the event that the bridge as a whole intrudes, the pontics will touch there, creating a hypomochlion and limiting the free movement of the bridge. a The area before grinding the base area of a“Brosamle” bridge (see Chapter 11.2). b The result of the procedure
9.
Inform the patient of the necessity of regular recall appointments. Give additional instructions in oral hygiene if necessary. Ask the patient if he still has the folder with the instructions for oral hygiene and the emergency numbers. Should that not be the case, the patient should be handed a new folder (Form 5a) immediately. Note the version number of the folder on the patient chart.
10.
If required: Fill in the check-up report and file it while handing one copy to the patient to take home.
26.1.3 Indication for Radiographs
In crestal implantology, the literature always calls for “control radiographs” to be taken immediately after the implants have been inserted. We do not think that this is necessary in the case of BOI implants, because these implants are inserted with a fully open line of sight and because it is not possible anyway to verify the correct bicortical position using conventional radiological systems. It may be helpful to check the seating of the bridge radiologically or to detect excess cement during the postoperative phase, where the view is often obstructed (swellings, minor bleeding). Once the superstructure has been inserted, radiographs will document the number of crowns, pontics, and implant-supported attachments for subsequent billing.
After that point, we recommend taking radiographs at 6-month intervals. The last routine radiograph of this series is taken after 2 years. After that, radiographs will usually only be required if problems arise or if there are natural teeth left in the jaw whose status must be inspected radiologically.
If extensive areas have been restored, a panorama radiograph (orthopantomograph, OPG) can be useful because it visualizes and documents changes in bone structure, such as new trajectorial alignments.
In the event that individual implants are not clearly visible on the OPG, a smaller radiograph of the respective area can be taken. Occasionally it may be necessary to take a tomograph in order to verify bicortical anchorage.
26.1.4 Safeguard Information and Therapeutic Information During Recall
In order to be able to prove – in the event of any disagreements or lawsuits – that the patient had been informed of developing problems, deficiencies in oral hygiene and additional treatment needs in a timely manner, it will often be useful to give recommendations and instructions to the patient in written form. Many patients are afraid and insecure during their visit to the dental office and may not be able to remember all the information they received once they have left there.
The patient carries the burden of proof with regard to the first part of the check-up report (safeguard information); with regard to the second part (therapeutic information), the burden of proof rests with the treatment provider.
It is important to inform the patient of the time of the next routine appointment and to instruct the patient to contact the dental office for an immediate appointment in the event that pain or discomfort occurs or that any changes manifest themselves.
Having the patient sign the recommendation and keeping a copy makes sense if the treatment provider carries the burden of proof or if he knows or has reason to assume that the patient is unwilling to follow the instructions and treatment recommendations. This may occur, for example, when other dentists have made other, unfortunately usually incorrect, treatment recommendations – especially if these incorrect treatment recommendations are made by university dentists or other “specialists”. In this case, the patient may be extremely, and sometimes irreversibly, confused.
26.1.5 Occlusal Adjustments and Compensation of Changes in the Bone Morphology
With dentures, it is obvious that changes on the occlusal face height are to be expected (Smith 1975). The same applies to implant treatments in many cases. If integrated screw implants are used, the phase of bone remodelling will mainly have taken place in the unloaded period. Hence, when the bridges or dentures are installed on the implants, few further vertical changes are observed. In this respect, treatment with BOI implant under immediate load conditions shows a different development. Typical changes in anterior or posterior face height are shown in Figs. 26.4 and 26.5.
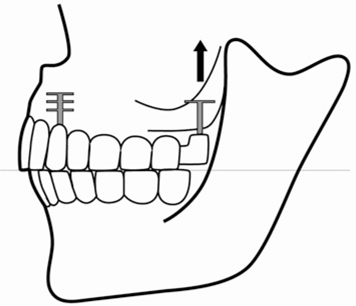
Fig. 26.2.
After placement of the upper bridge in immediate load, the mastication and the relationship between the two arches will be regular. However, in the case shown here, the distal bone area has a tendency to shrink in a cranial direction. This can be observed quite frequently. An alternative development is described in Fig. 18.7
There are numerous reasons why it may be necessary to make subtractive or additive corrections to implant-supported bridges:
-
The vertical bone level changes in both jaws (see Chapters 9.3 and 18). These modifications are much more extensive than one might expect. If, for example, the disks in complete mandibular restorations are raised by 1–2 mm and, at the same times, the distal disks in the maxilla are lowered by 1–2 mm, a reduction of the bridge construction of 2–4 mm in all is required in the distal area in order to once again ensure uninhibited masticatory function. This will certainly require a reduction in the area of the bridge framework. Another aspect to consider is that the development of a preferred chewing side requires an unequal amount of adaptation on both sides.
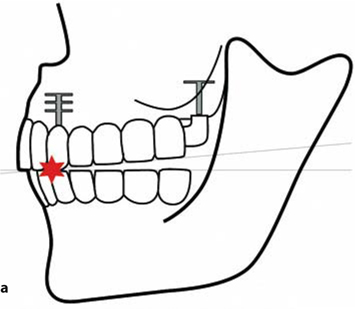
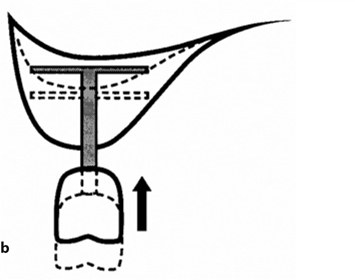 Fig. 26.3.a Following intrusion of the maxillary distal BOI implant, premature contacts in the anterior part of the arches are found. This may trigger an unwanted anterior chewing pattern. In this situation, there is no chance of any equilibrated masticatory function developing, since the vestibular cusps cannot touch in the enter phase (cf. Fig. 10.9). The dentist will often be unable to recognize the situation immediately, e.g. if the increased resilience of the temporomandibular joint barely allows distal functional contact. It is necessary to observe the masticatory pattern in a realistic situation (e.g. using sufficiently thick bite registration paper), b The change in position of the distal implant is shown from distally. As the width of the maxilla increases, the further up you go, the BOI implant must be chosen to be wide enough. The additional insertion of a tuberopterygoid screw implant may help stabilize the vertical dimensions
Fig. 26.3.a Following intrusion of the maxillary distal BOI implant, premature contacts in the anterior part of the arches are found. This may trigger an unwanted anterior chewing pattern. In this situation, there is no chance of any equilibrated masticatory function developing, since the vestibular cusps cannot touch in the enter phase (cf. Fig. 10.9). The dentist will often be unable to recognize the situation immediately, e.g. if the increased resilience of the temporomandibular joint barely allows distal functional contact. It is necessary to observe the masticatory pattern in a realistic situation (e.g. using sufficiently thick bite registration paper), b The change in position of the distal implant is shown from distally. As the width of the maxilla increases, the further up you go, the BOI implant must be chosen to be wide enough. The additional insertion of a tuberopterygoid screw implant may help stabilize the vertical dimensions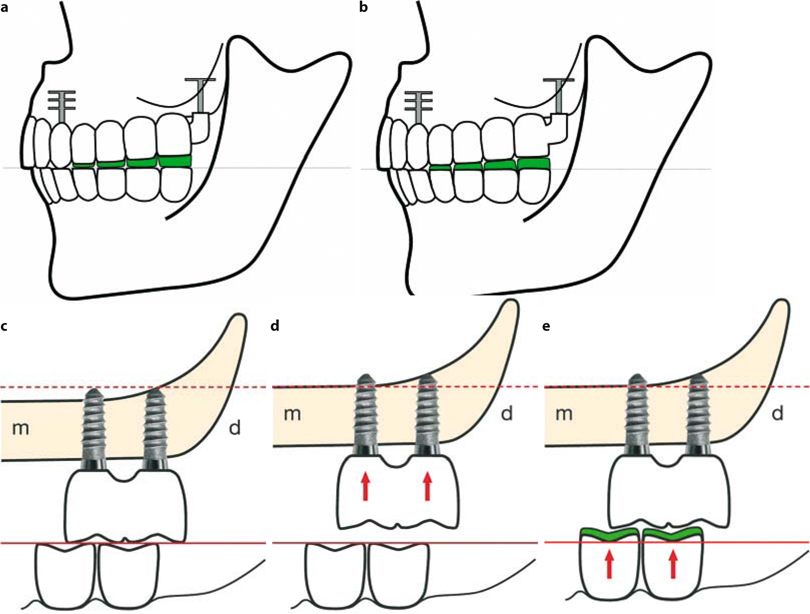 Fig. 26.4.a If adjusting the anterior teeth is not an option, the buildup of the distal pontics must be considered. This picture shows the buildup of the maxillary bridge – a procedure that is rarely required. b Whether the upper or lower arch has to be built up depends on the occlusal plane: all adjustments must be made with respect to the established curves of Spee and Wilson and the horizontal plane. The mandibular teeth must be built up more frequently than the maxillary bridge, so this is the first option in the treatment of lateral non-occlusion, c–e Resorption of bone in the distal maxilla is also a usual development with crestal implants. The decrease in the distal vertical dimension is compensated by extrusion of the molars of the lower jaw, or by a gradual adjustment of the joints. In many cases, however, build-ups are necessary in order to re-establish the distal vertical dimensions and prevent destructions in the area of the joint
Fig. 26.4.a If adjusting the anterior teeth is not an option, the buildup of the distal pontics must be considered. This picture shows the buildup of the maxillary bridge – a procedure that is rarely required. b Whether the upper or lower arch has to be built up depends on the occlusal plane: all adjustments must be made with respect to the established curves of Spee and Wilson and the horizontal plane. The mandibular teeth must be built up more frequently than the maxillary bridge, so this is the first option in the treatment of lateral non-occlusion, c–e Resorption of bone in the distal maxilla is also a usual development with crestal implants. The decrease in the distal vertical dimension is compensated by extrusion of the molars of the lower jaw, or by a gradual adjustment of the joints. In many cases, however, build-ups are necessary in order to re-establish the distal vertical dimensions and prevent destructions in the area of the joint -
Masticatory forces and masticatory functions increase, which may also lead to changes in the positions of the temporomandibular joints.
-
The mastication pattern changes, which automatically changes the shape of the jawbones as well.
-
Following changes in vertical dimension, leverage and tension between the bones and the muscles will change as well, creating new trajectories in the bone. This, too, will lead to morphological changes. The extent of these changes is smaller if no changes in vertical dimension had been necessary.
-
Each recall session will show differences in muscular state and differences in jaw morphology. The dentist will have to assess whether or not to respond to these changes by adjusting the occlusal structures. The occlusion can never be finalized, i. e. occlusal adjustment is never complete, when a restoration is first inserted.
-
Periodontally involved dentitions will cause significant changes in muscular function if the masticatory forces had previously been reduced due to pain-related feedback reactions. In addition, more pronounced and faster remodelling must be expected in these dentitions, which cannot be considered stable preoperatively.
-
By contrast with complete denture treatment, repositioning a bridge on BOI implants is not usually possible, since the bridge will be firmly cemented in place.
-
Antagonists may continue to move or shift, even if a fixed bridge supported by BOI implants is present in the treated jaw.
-
Increased masticatory forces will cause the muscles to shorten noticeably, which may lead to premature contacts, especially on the posterior region. The need for occlusal adjustments in this region will be frequent and extensive. Adjustments are best made to the maxilla in order to have the bite plane more closely approach Camper’s plane and to maintain a favourable distribution of forces (Katona 1989).
-
The jawbone-resting systems of secondary osteons is disturbed, and the externally visible morphology changes during repair (compare to Fig. 9.6 showing a possible alternative development with no changes visible from outside).
The general rules are:
1.
The first adjustment is extremely important, but never possibly correct or final.
2.
Subsequent adjustments are more important.
3.
Vertical dimension must be rebuilt after a series of grinding adjustment in order to maintain an equilibrium. Adjusting therefore means building up the curves of Spee and Wilson.
4.
Even without any adjustments, the vertical dimension may be lost only by changes in the morphology of the bone which follow functional changes. Therefore regular monitoring of the situation is necessary.
Since the above mentioned changes take place gradually or suddenly, it is usually not possible to decide already after months, whether or not the masticatory function was installed correctly in the beginning. This fact has to be remembered, whenever this question is raised in court cases. Usually it can only be stated, that either the maintenance (or compliance) may have been insufficient or that functional problems have not been discovered or that it may have been impossible to discover functional changes or that functional changes have occurred rapidly. As explained in Chapter 17, CMD patients show a strong tendency to overly adapt to a wrong occlusal situation without giving the dentist the necessary information to perform adjustment.
26.1.6 Special Considerations When Inserting a Second Round of Implants
If BOI implants are added (for instance following the extraction of teeth) to a jaw that already contains a number of well-mineralized BOI implants, one should expect painful sensations in the regions of the pre-existing implants to occur approximately 4 weeks after the new implants have been placed. This pain is a consequence of the remodelling process, a process that – as Chapter 9 has shown – always includes extensive areas of the jaw. However, this pain will disappear all by itself, no later than after three to four months, that is, once the remodelling process has been completed. Nevertheless, the masticatory function must be checked and, if necessary, corrected, since one would have to expect morphological changes to the bones that will need to adjustment by way of the occlusal surfaces.
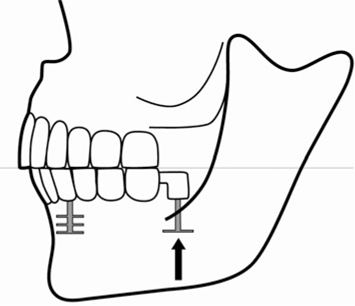
Fig. 26.5.
If the distal implant is positioned in the anterior part of or below the maxillary sinus, extrusion of the implant is likely to occur in cases with strategic implant positioning. This may be a result of the expansion of the maxillary sinus, the shortening of the vertical chewing muscles (mm. pterygoideus medialis and mm. masseter) and repositioning of the joints. Unwanted early contacts are found on the first molars. These contacts must be removed regularly until the masticatory system and the osteonal systems come to a stable rest again. For the osteonal system this may take 1–2 years (see Videos 25 and 27 and compare Fig. 26.2 to 26.4b showing the opposite development if the distal BOI is positioned behind the maxillary sinus; compare also to Fig. 9.43)
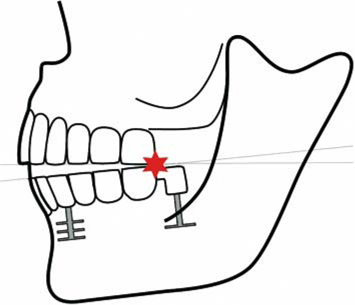
Fig. 26.6.
See Fig. 26.5
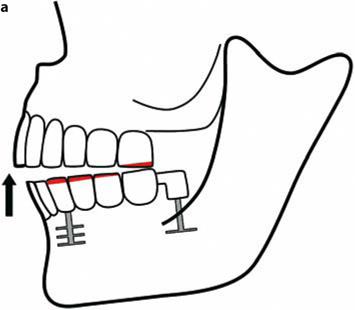
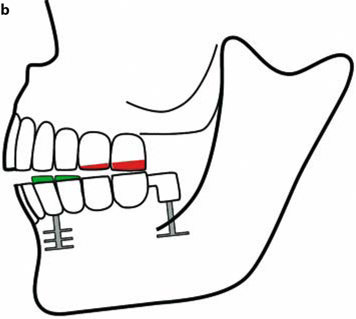
Fig. 26.7a,b.
If the mandible is implanted and the distal BOI implant is elevated, premature contacts will occur distally.These premature contacts can have various origins. On one hand, the increasing masticatory forces are accompanied by shortened vertical masticatory muscles, which may contribute toward a reduction in space available for the temporomandibular joint. On the other hand, true morphological changes may occur in the bone (Ihde 2003), which would cause the BOI implants to be dislocated in a crestal direction (see Case Study #7 in Chapter 9.1)
This pain must be differentiated diagnostically from pain whose origin lies in the muscles. The dentist, however, will easily be able to ascertain and locate the muscular origin in these cases, which may also be associated with myogelosis. Patients will be tempted to attribute muscular pain to the distal implants of both jaws (muscular trigger point syndrome). Muscular problems may be treated by jaw-stretching exercises (keeping the mouth wide open for 1 min, several times daily) and self-massage (patients are usually good at locating their own myogeloses and can “treat” them, for example, at night while watching television.
If integrated BOI implants are provided with new superstructures that change the vertical relation, the patient will experience remodelling to an extent one would usually associate only with surgical procedures. This is why it is so important to also follow these patients closely and to adjust the occlusion at narrow intervals, as well as to instruct the patient not to exert excessive masticatory forces for 6–8weeks – just as at the time of the insertion of the first superstructure.
Pre-loads on integrated implants are more harmful than on old (integrated) BOI implants because the bone around the disks has already mineralized. The risk of fractures is correspondingly higher. Re-using the existing bridge frameworks should be preferred.
26.1.7 The Mobility of ED Implants Against Abutments
The fine thread (M2×0.25) of the ED-type BOI implant may develop a certain amount of mobility against the abutment, especially if only a few implants were inserted per jaw. The reason for this is a slight plastic deformation of the implant or abutment thread. This situation will manifest itself to the patients by a slight “clicking” noise as they move their jaws. The first time this noise occurs is usually after about 6 weeks. Normally, this clicking sound will disappear all by itself after a few weeks, because continuous remodelling of the jaw will create or modify tension between the individual implants that will cause the threads to be “wedged” against each other again. Remodelling creates tension between the bony implant beds (integration, however, is preserved). As long as the treatment provider can be sure that the abutments were firmly screwed onto the threaded pin, there is no need for any therapeutic measures. However, it is necessary to reassure the patient and to double-check the stability of the implants.
The patient’s successful self-observation and his willingness to seek his treatment provider’s advice immediately is a behaviour that should be reinforced by praise.
26.1.8 Conclusion
The living human cranium has no absolute reference points whatsoever. Nor do implants constitute such absolute reference points, even if they are osseointegrated. Implants can change their positions along with the surrounding bone. This fact has to be accommodated by modifying the restorative superstructure. The extent of the necessary modifications is impossible to predict and almost impossible to control. Regular thorough recall examinations are indispensable for treatment success. Changes in bone morphology occur after functional changes as well as after surgical interventions. The changes are cumulative and are influenced by changes in basic tension and the length of the affected muscles. The necessary modifications will usually be so extensive that it will not always be possible to prevent metal from becoming visible next to the ceramic veneers. Especially in patients with very high aesthetic expectations, this will necessitate fabrication of a new restoration from time to time.
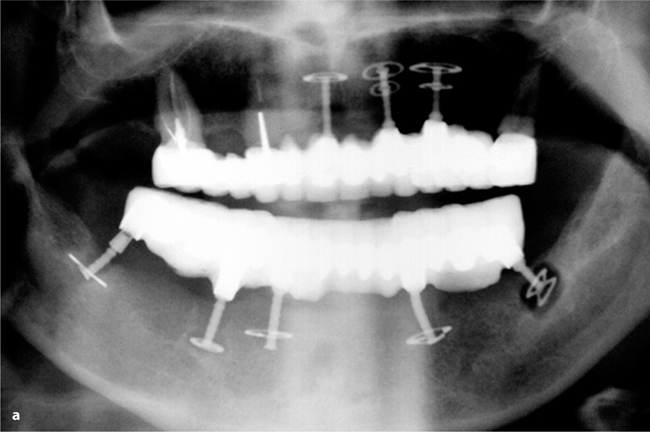
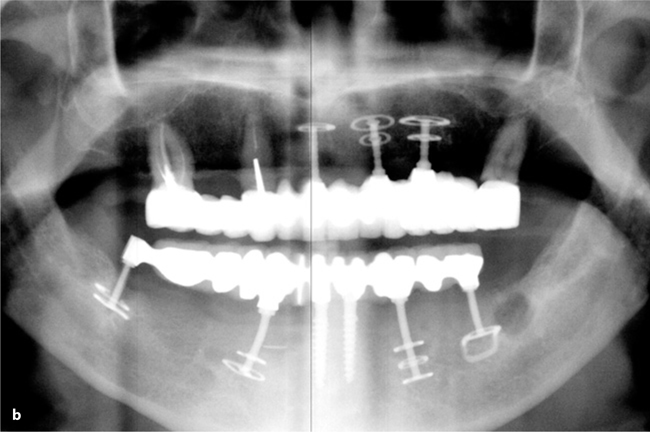
Fig. 26.8a,b.
Some time after the BOI implant in area 37 had become mobile all the implant-prosthetical system lacked the necessary distal support on one side. The implant was not replaced in a timely enough manner. This resulted in cracks of the other implants and severe mobility of the implant in Region 44. The patient did not report any pain. Even in this really undesirable situation he was happy to have teeth which were more “fixed” than the denture he had worn before. The case had to be redone and this was performed in one surgical intervention: all implants were exchanged. One base-plate was left in the bone. There is some discussion about leaving integrated base-plates in the bone. These plates are foreign bodies and they are no longer stimulated after the threaded pin has been removed. We usually take all of the implant out whenever this seems possible
26.2 Troubleshooting
The player on the opposite side will always give you another chance. He knows that your victory is his victory. There are two victories for each defeat.
Paulo Coelho
26.2.1 There Are More Solutions Than Problems
Whether a treatment method is really fit to be used in clinical practice is determined not least by one question: If a single component fails, will it be possible to make adequate repairs and corrections in a manner that is simple and that the patient can afford?
Occasionally, cemented bridges will come loose from individual bridge abutments. This is, of course, undesirable, and it may result in the additional loss of cementation on other abutments. This in turn may cause incompatible overload effects, leverage forces or vibrations through resonance. If, however, a bridge is supported by fewer and fewer abutments, and finally only one last abutment, the implant carrying this abutment may ultimately fracture.
Implant fractures are no more frequent in BOI implants than in crestal implants. However, repairing the damage is usually much easier in the case of BOI implants than for crestal implants. The fracture process usually entails material fatigue in the region of the basal plate. If this basal plate is replaced in time, no additional damage will occur. If replacement is delayed, the mobile threaded pin may cause bacterial inoculation, which in turn may result in the loss of bone volume (structural collapse around the threaded pin) and more pain during and after the replacement operation.
First of all, the treatment provider will examine the option of removing the bridge. In this respect, screw bridges on ID or IDO/IDDO/IDOT implants are easier to handle. However, screw bridges are more difficult to repair. If the bridge itself has occlusal openings (we generally recommend having those openings created during the fabrication of the bridges), one might attempt to use suitable instruments to loosen the bridge from its support, abutment by abutment. Transversal grooves applied in the non-visible area of the abutment with a tungsten carbide bur might also give some leverage for potential bridge removal.
If it is not possible to remove the bridge in order to re-cement it, there are two useful treatment alternatives:
-
If a sufficiently wide gap is present between the bridge and the abutment where the loosening occurred, or if such a gap can be created by using a bur or other rotary instrument, it will be possible to reattach the bridge to the abutment using acrylate-based cement. This requires that the gap between the bridge and the abutment to be cleaned and any greasy residue to be removed, something that is easily achieved using hydrogen peroxide and ethanol. Some treatment providers like to rinse the gap with Betaisodona for disinfection first. Monomer is subsequently introduced, attempting to wet all surfaces in the process. Thin-flowing cementing acrylate (such as Cerafix Genta by Ceraver, Frankfurt/Germany, or Pattern Resin) can now be introduced into the gap. Here it will polymerize within the time specified by the manufacturer. During this time, the position of the bridge should not be changed to ensure that the acrylate matrix is not damaged.
-
Especially in situations in which the need for bridge reattachment coincides with a desire to effect changes in masticatory parameters (such as raising the bite, adapting the curves of Spee and Wilson, adjustments to the opposing dentition), overbridges can be useful. The advantages of overbridges compared to the fabrication of a completely new bridge can be summarized as follows:
-
The positional and tensional relationships of the implant will remain unchanged. This is particularly desirable if the implants were placed strategically or if a need to make changes and adjustments has arisen within the first 12–24 months after the implants were placed. The mineralization process remains undisturbed, and the implant-bone interface will not be disturbed.
-
The patient will continue to wear a fixed restoration.
-
Repair is less costly than the fabrication of a completely new superstructure. Often only lateral segments need to be exchanged (see Fig. 17.7)
-
The treatment is usually less extensive and will therefore progress more quickly.
Fabrication of a new bridge may be considered if undesirable and noticeable gaps between the bridge and the alveolar ridge have opened due to resorption of the soft tissues (especially following extractions in the anterior maxilla), gaps that might be eliminated in the course of fabricating and inserting a new bridge.
Among the most frequent indications for over-bridges are treatments with considerable positional anomalies of the temporomandibular joints at the outset. The process of normalization and reduction of the joint position will initially cause resistance on the part of the muscles, and the occlusal surfaces will have to be adjusted with some frequency. It is usually the first bridge that is being reduced or augmented with composite in this context. The consequences of occlusal adjustment and the risk of composite loss can both be treated by inserting an overbridge. Overbridges thus also serve as permanent splints with very appealing aesthetic properties. It is an advantage to veneer all bridges with ceramics from the start. Ceramics are easy to adjust, and after etching with ceramic etching gel, any additive modification of the morphology of the occlusal surfaces can be easily built up with adhesive composite. If, by contrast, a composite veneer is used in one of the two jaws, the more abrasion-resistant ceramic material can open up functional paths in the dentition of the opposite jaw, which, while it may protect the implants to a certain extent, may also be the starting point of an undesirable lateralization of the masticatory function. Regular recalls are important – especially in the first 2–3 years after the first installation of a prosthodontic superstructure or following alterations to an existing superstructure.
If, by hindsight, the position of the implant shaft (determined intraoperatively based on the available bone volume) turns out to be less favourable, the problem is often easily solved using an overbridge. The original bridge is prepared, the threaded pin is repositioned by flexing within the limits of the material, and an impression is taken of the new position.
Smaller, unveneered overbridges are fabricated to attach replacement implants to existing bridges. Prior to replacing the implant, the residual bridge is prepared, and the bridge surface of the overbridge is modelled in acrylate (e.g. Pattern Resin). It is important to make sure that these steps are performed before any surgical intervention to keep any preparation debris from entering the freshly sutured wound. Once the new implant is in place, the abutment can be screwed onto the implant immediately and connected with the overbridge part previously modelled in acrylate using self-curing adhesive acrylate. This template can be invested immediately and cast in metal. In this manner, the patient can often be provided with a definitive fixed restoration only a matter of 1–2h following the replacement of an implant.
For a veneered overbridge, the existing bridge is prepared occlusally and on the labial and lingual aspects over a distance corresponding to about two bicuspids. Care must be taken to ensure that no undercuts are created in the area in which the bridge will later be cemented. Vertical grooves should be included to withstand removal and shear forces. The distance between the abutment and the bridge “die” must be sufficient to permit later insertion of the bridge.
If, at the time of implantation, the bone supply had been insufficient to permit parallelizing by bending the abutments, this can usually be performed several months later; the overbridge can be attached to the bridge to accommodate the new position of the implant.
26.2.1.1 Case Study 2
The following three pictures show different steps to be performed when fabricating an overbridge.
Overbridges are cemented in place using definitive cement, for example glass-ionomer cement (such as Cem Base)
The option of modifying a superstructure rather than having to fabricate a completely new one will also make it easier for the treatment provider to “isolate” individual implants that might be subject to overloading. These isolated implants can later be reconnected using a small overbridge.

Fig. 26.9.
As the overbridge is being ground down, the distal abutment can initially secure the wide-span bridge. The abutment will not be cut until the very end. The ceramic veneer has already been largely removed. Undercuts, however, must not be created. Vertical grooves can be ground in to prevent removal in a distal direction

Fig. 26.10.
The completed overbridge and the model, occlusal view. The slightly tooth-like forms on the residual bridge will later allow the dental technician to build up the ceramic veneer to the required thickness and anticipate the shape of the tooth

Fig. 26.11.
Lateral view of the overbridge on the model
26.2.1.2 Case Study 3


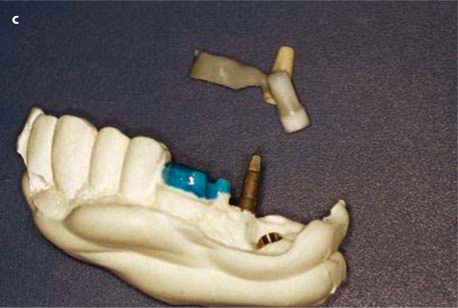


Fig. 26.12.
a, b Metal frame for combined cementing (on the distalmost BOI implant and the bridge) and screwing (onto the pterygoid screw), c Lateral aspect of the wax modellation. d Intra-oral view of the adjustment piece, e Occlusal view. It is recommended to use only temporary cement to fill the screw hole for the tuberopterygoid screw
26.2.1.3 Case Study 4
Replacing an implant in the middle of the bridge without removing the bridge can be achieved only if an access path can be cleared for a lateral osteotomy:
This procedure also has the advantage that the bridge per se remains firmly in its place. The tensional relationships between all the other implants will remain unaffected. Also, the patient continues to wear a fixed restoration, and the cost of the repair is relatively low. One thing to consider is that the fracture of a BOI implant will be the result of very strong forces that will invariably also affect the other implants within the same jaw-implant-restoration system. These cases have to be followed very closely.
Replacing a BOI implant requires a certain skill, but this interesting task has the invaluable advantage of giving the user an in-depth understanding for the treatment procedure and for the benefits of being able to work in the depth of the three-dimensional bone space. Problems and their solutions will always teach us more than any routine task.





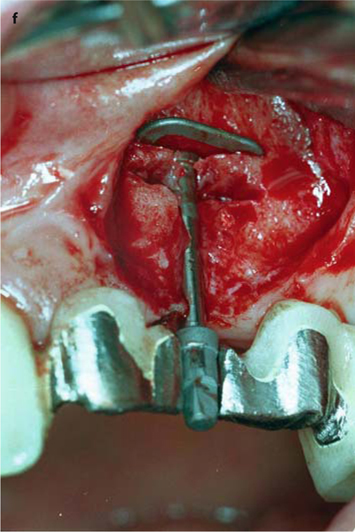

Fig. 26.13.
a Prepared area of the bridge prior to surgical intervention. b The threaded pin has been severed from the bridge. The attachment could already be accommodated. c The implantologist needs a good view of the implant site. d, e The implant can now be removed in a vestibular direction. f Further basally, a new osteotomy is made for the replacement implant (EDS 10 G10 in this case). The vertical position of the new implant, and thus of the abutment, is excellent. g The overbridge is cemented using glass-ionomer cement. – If an additional implant is to be integrated into the bridge, a very similar procedure can be followed
26.2.2 Fractures at the Threaded Pin
Fractures at the threaded pin are very rare. If they do occur, the fracture site will usually be located directly below the widened ledge of the thread.
Therapy: Fractures below the threaded pin can be treated by removing the superstructure and by placing a new threaded pin on the butt of the old one. There is a special tool TAP D that can be used together with the RAT 2 ratchet to achieve this goal. The implantologist should first become familiar with the use of these instruments by practising outside the mouth. The TAP D tool will press the new thread in soft (Grade 1,2) titanium onto the residual pin.
If the location of the fracture site is immediately below the ledge of the thread, the repair procedure will result in an implant that is about 4 mm shorter than before. To be able to reinsert the existing bridge, the longer TSD 44 abutment is used in place of the TSD 4 or a TSD 55 in place of the TSD 5. The polished part, which is 4 mm longer in an apical direction, can be sunk into the mucosa if needed. We use Terracortril ointment as a filling medium for the internal threading of the abutment. The new abutment can also be attached with resin cement (e.g. Cerafix Genta by Ceraver, Frankfurt/Germany). There is no direct replacement match for TSD 99 abutments. It is possible to use a TSD 4 abutment, but large open spaces will remain inside the crown that are best pre-filled with resin cement. It is also possible to cast a metal interface to be cemented or glued in place.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


