Key points
- •
In adults, the spinal cord terminates in the conus medullaris around L1-L2; the entry point should be the interspinous spaces below L2-L3 to lessen the chance of a neural injury.
- •
The distance from the skin to the epidural space is approximately 45 to 55 mm with the dura mater an additional 7 mm beyond that.
- •
Lumbar puncture is contraindicated in cerebral herniation, increased intracranial pressure, focal neurologic signs, suspected spinal epidural abscess, coagulopathy or anticoagulation therapy.
- •
The most common complication of lumbar puncture is post lumbar puncture headache, which may occur in up to 40% of patients undergoing lumbar puncture.
- •
Lumbar drains are indicated in patients who have undergone skull base surgery and developed a cerebrospinal fluid leak, subarachnoid hemorrhage, chronic meningitis cases, and for evaluation of normal pressure hydrocephalous.
Lumbar puncture
History
In the 1650s, a budding polymath, Christopher Wren, whose eventual interests ranged from astronomy to architecture, began using goose quills to intravenously deliver morphine in dogs to study the physical effects of injection of those compounds compared with oral use. Experimenters in England and Germany in the 17th century found the technique to be difficult to safely use, however, and complications including death led to the abandonment of the technique until the 19th century. The hollow needle with syringe was invented by Ferguson then championed by Alexander Wood of Edinburgh in the mid-19th century to deliver morphine for pain relief and later cocaine for anesthesia.
With the burgeoning interest in anesthesia in the 19th century, the development of techniques and equipment rapidly advanced in the last 2 decades of that century. Corning from New York City is attributed with having produced the first case of spinal anesthesia in a dog when he inadvertently punctured the dura between 2 lumbar vertebrae in while administering cocaine, causing paralysis of the lower extremities. Corning later proceeded to use this technique for a variety of neurologic disorders in humans, calling his procedure “spinal anesthesia.”
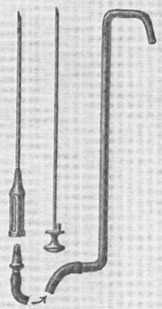
Heinrich Quincke, eventual Chair of Medicine at Kiel University, is considered the originator of the lumbar puncture, which he developed in the 1890s to relieve elevated intracerebral pressure in cases of meningitis, most commonly presumed to be tuberculous at that time. In his 1908 treatise on Lumbar Puncture , Quincke describes his expressly manufactured needles, which incorporated a steel mandrin (stylet) with a tip ground to exactly match the slanted surface of the needle. Drawings of his needle display little difference in structure from the cutting needles used today. Interestingly, in further describing the procedure, Quincke held that anesthesia was generally not necessary, describing the cutaneous pain as momentary and the pain when passing through the dura “under some circumstances, a valuable guide” ( Fig. 1 ).
Augustus Bier of Kiel followed Quincke, and using his needles successfully produced spinal anesthesia for lower limb surgery as reported in 6 case studies in 1899. This article eventually led to the widespread acceptance of this technique for surgical anesthesia. By the 1920s, however, with increasing experience, anesthetists found that the original larger bore and stiffer needles led to a greater risk of post lumbar puncture headaches (PLPH), which were felt to be owing to larger tears in dura mater causing leakage of spinal fluid.
In his initial studies, Bier and his assistant Hildebrandt first used spinal anesthesia on each other, producing a dense anesthesia that was impervious to burning cigars to the skin and needles inserted to the femur. After post anesthetic celebration with wine and cigars, Bier and Hildebrandt both suffered severe headaches with associated vomiting, which lasted for 4 days for Hildebrandt and 9 days for Bier, making these the initial case reports for PLPH.
Over the ensuing decades, a wide variety of needle designs have been tested for the express purpose of decreasing the size of the dural holes and decreasing the incidence of PLPH. The Hoyt system of the 1920s used 2 needles passing a smaller bore needle through a larger bore needle. The large needle was used to penetrate the tougher outer tissues and the finer bore needle was reserved for passing through the dura.
Greene, in presentations in 1923 and 1926, showed that a smaller dural hole was made if the cutting tip of the Quincke-type needle was rounded off by removing the cutting edges of the bevel. This led to the development of the Greene needle, a small-bore, rounded-tip needle passed through a larger introducer cutting needle with the understanding that only the small-bore needle would pass through the dura mater ( Fig. 2 ).
By the 1950s, Hart and Whitacre developed the pencil point needle without a cutting bevel to decrease the risk of PLPH. In this design, the tip was solid and sharp with an orifice several millimeters below the point. Although well-received, the orifice of the original needle was quite small, making aspiration and infusion difficult, and later models had larger orifices. The Sprotte needle developed in the 1980s modified the Whitacre needle by using a rounded penetrating tip and a much larger side orifice. Of further interest to the practitioner, programs that teach use of pencil point needles in diagnostic lumbar punctures recommend the use of a larger bore 18-gauge as an introducer through the surface of the skin in the same fashion as the older Greene needle.
There remain a wide number of spinal needles used for anesthesia, each finding a niche among proponents and remaining in production. In the experience of a general internist for diagnostic lumbar punctures, however, the Quincke-type cutting needle is generally the only needle available in the premanufactured kits the hospitals purchase, although kits with atraumatic Whitacre needles are available. Position papers from the American Academy of Anesthesiologists and the American Academy of Neurology encourage the replacement of cutting needles with atraumatic spinal needles. Although physicians may need to familiarize themselves with the differences in tip design, the Mayo Clinic Scottsdale made atraumatic needles available for lumbar puncture and saw an increase in use for diagnostic studies form 0% to 37% in 1 year.
Lumbar puncture
History
In the 1650s, a budding polymath, Christopher Wren, whose eventual interests ranged from astronomy to architecture, began using goose quills to intravenously deliver morphine in dogs to study the physical effects of injection of those compounds compared with oral use. Experimenters in England and Germany in the 17th century found the technique to be difficult to safely use, however, and complications including death led to the abandonment of the technique until the 19th century. The hollow needle with syringe was invented by Ferguson then championed by Alexander Wood of Edinburgh in the mid-19th century to deliver morphine for pain relief and later cocaine for anesthesia.
With the burgeoning interest in anesthesia in the 19th century, the development of techniques and equipment rapidly advanced in the last 2 decades of that century. Corning from New York City is attributed with having produced the first case of spinal anesthesia in a dog when he inadvertently punctured the dura between 2 lumbar vertebrae in while administering cocaine, causing paralysis of the lower extremities. Corning later proceeded to use this technique for a variety of neurologic disorders in humans, calling his procedure “spinal anesthesia.”
Heinrich Quincke, eventual Chair of Medicine at Kiel University, is considered the originator of the lumbar puncture, which he developed in the 1890s to relieve elevated intracerebral pressure in cases of meningitis, most commonly presumed to be tuberculous at that time. In his 1908 treatise on Lumbar Puncture , Quincke describes his expressly manufactured needles, which incorporated a steel mandrin (stylet) with a tip ground to exactly match the slanted surface of the needle. Drawings of his needle display little difference in structure from the cutting needles used today. Interestingly, in further describing the procedure, Quincke held that anesthesia was generally not necessary, describing the cutaneous pain as momentary and the pain when passing through the dura “under some circumstances, a valuable guide” ( Fig. 1 ).
Augustus Bier of Kiel followed Quincke, and using his needles successfully produced spinal anesthesia for lower limb surgery as reported in 6 case studies in 1899. This article eventually led to the widespread acceptance of this technique for surgical anesthesia. By the 1920s, however, with increasing experience, anesthetists found that the original larger bore and stiffer needles led to a greater risk of post lumbar puncture headaches (PLPH), which were felt to be owing to larger tears in dura mater causing leakage of spinal fluid.
In his initial studies, Bier and his assistant Hildebrandt first used spinal anesthesia on each other, producing a dense anesthesia that was impervious to burning cigars to the skin and needles inserted to the femur. After post anesthetic celebration with wine and cigars, Bier and Hildebrandt both suffered severe headaches with associated vomiting, which lasted for 4 days for Hildebrandt and 9 days for Bier, making these the initial case reports for PLPH.
Over the ensuing decades, a wide variety of needle designs have been tested for the express purpose of decreasing the size of the dural holes and decreasing the incidence of PLPH. The Hoyt system of the 1920s used 2 needles passing a smaller bore needle through a larger bore needle. The large needle was used to penetrate the tougher outer tissues and the finer bore needle was reserved for passing through the dura.
Greene, in presentations in 1923 and 1926, showed that a smaller dural hole was made if the cutting tip of the Quincke-type needle was rounded off by removing the cutting edges of the bevel. This led to the development of the Greene needle, a small-bore, rounded-tip needle passed through a larger introducer cutting needle with the understanding that only the small-bore needle would pass through the dura mater ( Fig. 2 ).
By the 1950s, Hart and Whitacre developed the pencil point needle without a cutting bevel to decrease the risk of PLPH. In this design, the tip was solid and sharp with an orifice several millimeters below the point. Although well-received, the orifice of the original needle was quite small, making aspiration and infusion difficult, and later models had larger orifices. The Sprotte needle developed in the 1980s modified the Whitacre needle by using a rounded penetrating tip and a much larger side orifice. Of further interest to the practitioner, programs that teach use of pencil point needles in diagnostic lumbar punctures recommend the use of a larger bore 18-gauge as an introducer through the surface of the skin in the same fashion as the older Greene needle.
There remain a wide number of spinal needles used for anesthesia, each finding a niche among proponents and remaining in production. In the experience of a general internist for diagnostic lumbar punctures, however, the Quincke-type cutting needle is generally the only needle available in the premanufactured kits the hospitals purchase, although kits with atraumatic Whitacre needles are available. Position papers from the American Academy of Anesthesiologists and the American Academy of Neurology encourage the replacement of cutting needles with atraumatic spinal needles. Although physicians may need to familiarize themselves with the differences in tip design, the Mayo Clinic Scottsdale made atraumatic needles available for lumbar puncture and saw an increase in use for diagnostic studies form 0% to 37% in 1 year.
Anatomy
The brain and spinal cord float within the fluid of the subarachnoid space, which is estimated to be 140 to 270 mL in adults. This fluid is produced from the arterial circulation primarily in the ventricles of the brain and is absorbed into the venous plexus and lymphatics of the central nervous system. The rate of cerebrospinal fluid (CSF) production is approximately 600 to 700 mL/d.
In adults, the spinal cord terminates in the conus medullaris around L1-2; consequently, the entry point for lumbar puncture should be the interspinous spaces below L2-3 to decrease the chance of a neural injury. Using surface anatomy, the intercrestal line between the iliac crests, often called Tuffier’s line, is usually thought to mark the body of L4 or the L4-5 interspace. In a fluoroscopic study, however, the palpated intercrestal line was most frequently L3-4, especially in heavier individuals, whereas the radiographic intercrestal line was most frequently L4-5. The L3-4 interspace is considered safe for lumbar puncture, and the technique of palpation has more than 100 years of clinical experience. If a question arises regarding the proper interspace on palpation, taking the distal (caudal) option seems warranted.
The distance from the skin to the epidural space is approximately 45 to 55 mm with the dura mater an additional 7 mm beyond that. Therefore, a standard 90-mm Whitacre needle needs to be inserted about two-third’s of its length before it even reaches the ligamentum flavum. It will then need to be advanced an additional 10 mm before puncturing the dura to obtain CSF. Standard Quincke cutting needles in kits are usually 3.5 inches long and consequently would need to be inserted for more than one-half of its length before the dura mater could be punctured. Many physicians who frequently perform lumbar punctures, however, can describe cases of obese patients where the needle was inserted to the hub before obtaining fluid ( Fig. 3 ).
Contraindications
Lumbar puncture should be eschewed in patients with current or developing signs of cerebral herniation, those with potentially increased intracranial pressure and focal neurologic signs, suspected spinal epidural abscess, or coagulopathy. In addition, it should also be avoided or performed cautiously in patients with significant cardiorespiratory compromise. CT of the head or other neuroimaging studies of the brain cannot completely exclude raised intracranial pressure before lumbar puncture, but they can exclude a mass lesion, which poses substantial risk. Patients with coagulopathy are at increased risk for developing subdural or epidural hematomas. Lumbar puncture is contraindicated in patients with severe thrombocytopenia, bleeding diatheses, or anticoagulant therapy. Lumbar puncture can be safely performed with platelet counts of 50 × 10 9 /L or higher. Aspirin therapy in isolation does not seem to pose a significant risk in spinal anesthetic, but data regarding clopidogrel and other GPIIa/IIIb inhibitors are lacking. Warfarin should be stopped approximately 5 to 7 days before lumbar puncture and the International Normalized Ratio should be less than 1.2. Clear guidance with the use of the newer novel oral anticoagulants (dabigatran, apixiban, and rivaroxaban) is insufficient, but some institutional guidelines have recommended cessation of 1 to 5 days based on the agent itself and the patient’s creatinine clearance ( Table 1 ).



