Rheumatoid arthritis is a chronic inflammatory condition that can result in progressive destruction of the articular surfaces of the joints, including the temporomandibular joint. The purpose of this article is to report the conservative correction of a Class II malocclusion in a woman with rheumatoid arthritis. The patient was 32 years 6 months old at the start of treatment. She had a convex profile and a skeletal Class II jaw-base relationship caused by severe condylar resorption. An anterior open bite of −2.0 mm and an excessive overjet of 10.0 mm were observed. Severe crowding was shown in the mandibular incisors. After 8 months of splint therapy, all first premolars were extracted, and 0.018-in preadjusted edgewise appliances were placed in both arches. Class II elastics were used during space closure. After 41 months of active orthodontic treatment, an acceptable occlusion was achieved, and the facial profile was considerably improved. From the cephalometric evaluations, the mandible was rotated counterclockwise, and the mandibular plane angle was significantly decreased. However, the anteroposterior position of the chin was not changed. The condylar resorption was not changed during and after orthodontic treatment. Conclusively, the proper facial profile was maintained, and the occlusion was stable after a 5-year retention period. Our results suggest the possibility of compromised treatment in a Class II malocclusion with an anterior open bite because of rheumatoid arthritis.
Rheumatoid arthritis is a chronic inflammatory condition that is presumed to be an autoimmune disorder, but it can be modulated by other factors such as genetics, microbes, hormones, and the environment. The nonsuppurative inflammatory process of rheumatoid arthritis causes progressive destruction of the articular surfaces of the joints, and affects fingers, wrists, hands, ankles, feet, toes, elbows, shoulders, hips, and knees symmetrically. It is the most frequent systemic inflammatory disease involving the temporomandibular joint (TMJ). In the TMJ, the pannus surrounding the articular disc and the articulating surfaces cause destruction of the disc, condyle, fossa, and articular eminence. These progressive changes in the TMJ often precipitate the development of dentofacial deformities. Bone resorption in the condyles induces subsequent downward and backward rotation of the mandible, resulting in a skeletal Class II malocclusion with an anterior open bite, a steep mandibular plane angle, an increased lower facial height, and a decreased chin projection.
Patients with rheumatoid arthritis and severe condylar resorption are mainly treated with surgical procedures. Numerous reports have indicated that surgical correction of rheumatoid-associated TMJ disease and the resulting dentofacial deformity can successfully be treated by a surgical TMJ reconstruction with mandibular advancement surgery with or without maxillary orthognathic surgery and genioplasty. Nevertheless, some patients do not want surgical correction. Conservative treatment is a compromise to reconstruct the occlusion that was worsened by the condylar resorption. However, there are few reports of long-term observation of orthodontic treatment in the patients with severe condylar resorption caused by rheumatoid arthritis.
This article demonstrates the long-term successful outcome of conservative orthodontic treatment in a rheumatoid arthritis patient with a Class II malocclusion caused by severe condylar resorption.
Diagnosis and etiology
A woman, aged 32 years 6 months, had a chief complaint of masticatory disturbance. She had felt spontaneous pain in both TMJs when she was a teenager, but it had disappeared without therapeutic measures. At 23 years of age, she was diagnosed as having rheumatoid arthritis and started therapy with an antirheumatoid agent (D-penicillamine) and a nonsteroidal anti-inflammatory drug (diclofenac sodium). She had to be treated for edema of the knees by removing water once each month. As a result of the administration of these medications for about 10 years, the symptoms of the rheumatoid arthritis were reduced. Dull arthritic pain still remained, but she had no functional disturbances in her daily life.
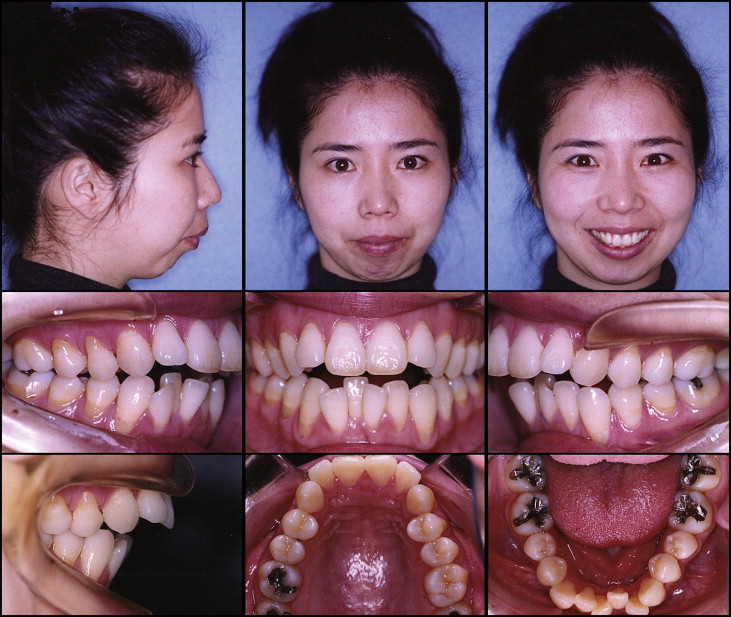
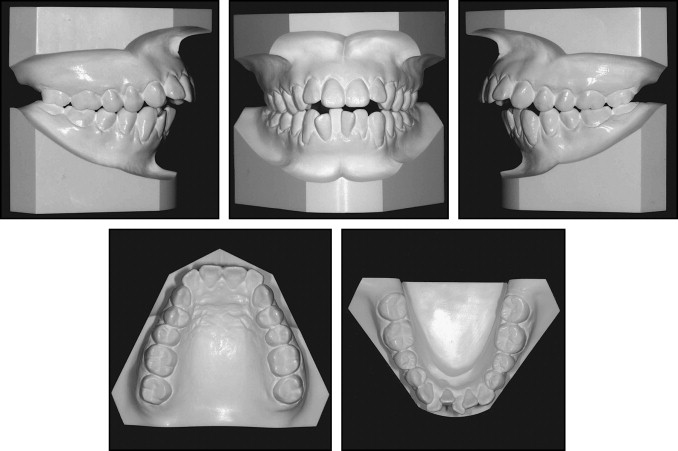
Her facial profile was convex with a retrognathic mandible ( Fig 1 ). An acute nasolabial angle, an increased lower facial height, and circumoral musculature strain on lip closure were observed. The molar relationships were Angle Class II on both sides ( Fig 2 ). Overjet and overbite were 10.0 and −2.0 mm, respectively. Two distinct occlusal planes were present in the maxillary arch, and occlusal contacts were found only in the molar regions at maximum intercuspation. Severe crowding was evident in the mandibular dentition, because of the excessive tooth size compared with the available arch length. The maxillary and mandibular dental midlines almost coincided with the facial midline. Gingival recession was found labially to the mandibular incisors and canines, and all premolars in both arches.
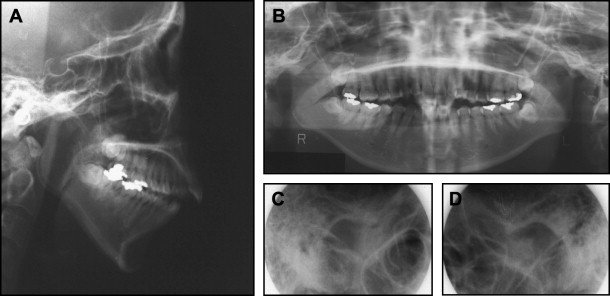
The radiographs showed that the third molars were present, and severe condylar resorption had occurred on the both sides ( Fig 3 ). The cephalometric analysis, when compared with the Japanese norm, showed a skeletal Class II jaw-base relationship (ANB, 13.0°) with mandibular retrusion (SNB, 68.5°) ( Table ). The mandibular plane angle was extremely steep (mandibular plane-Frankfort horizontal plane, 52.5°). Ramus height was significantly decreased because of severe condylar resorption (Ar-Go, 32.0 mm), but the mandibular body length was within the normal range. The maxillary incisors were lingually inclined (U1-Frankfor horizontal plane, 103.0°), and the maxillary and mandibular incisors were significantly extruded (U1/palatal plane, 35.0 mm; L1/mandibular plane, 50.5 mm).
| Variables | Japanese norm | SD | Pretreatment 32 y 10 mo |
Posttreatment 37 y 3 mo |
Postretention 42 y 7 mo |
|---|---|---|---|---|---|
| Angles (°) | |||||
| ANB | 2.8 | 2.4 | 13.0 | 13.0 | 13.0 |
| SNA | 80.8 | 3.6 | 81.5 | 81.5 | 81.5 |
| SNB | 77.9 | 4.5 | 68.5 | 68.5 | 68.5 |
| Mand pl-FH pl | 30.5 | 3.6 | 52.5 | 50.5 | 50.5 |
| Gonial angle | 122.1 | 5.3 | 124.5 | 120.0 | 120.0 |
| U1-FH pl | 112.3 | 8.3 | 103.0 | 93.0 | 93.0 |
| L1-mand pl | 93.4 | 6.8 | 91.0 | 86.0 | 87.0 |
| Interincisal angle | 123.6 | 10.6 | 113.5 | 132.0 | 132.0 |
| Occlusal pl | 16.9 | 4.4 | 31.5 | 38.0 | 38.0 |
| Lines (mm) | |||||
| S-N | 67.9 | 3.7 | 71.0 | 71.0 | 71.0 |
| N-Me | 125.8 | 5.0 | 132.5 | 130.5 | 130.5 |
| Me/palatal pl | 68.6 | 3.7 | 71.0 | 69.0 | 69.0 |
| Ar-Go | 47.3 | 3.3 | 32.0 | 31.0 | 31.0 |
| Ar-Me | 106.6 | 5.7 | 94.0 | 94.0 | 94.0 |
| Go-Me | 71.4 | 4.1 | 70.5 | 70.5 | 70.5 |
| Overjet | 3.1 | 1.1 | 10.0 | 4.0 | 4.0 |
| Overbite | 3.3 | 1.9 | −2.0 | 4.0 | 4.5 |
| U1/palatal pl | 31.0 | 2.3 | 35.0 | 34.5 | 34.5 |
| U6/palatal pl | 24.6 | 2.0 | 23.5 | 21.5 | 21.5 |
| L1/mand pl | 44.2 | 2.7 | 50.5 | 49.5 | 50.0 |
| L6/mand pl | 32.9 | 2.5 | 37.0 | 38.5 | 38.5 |
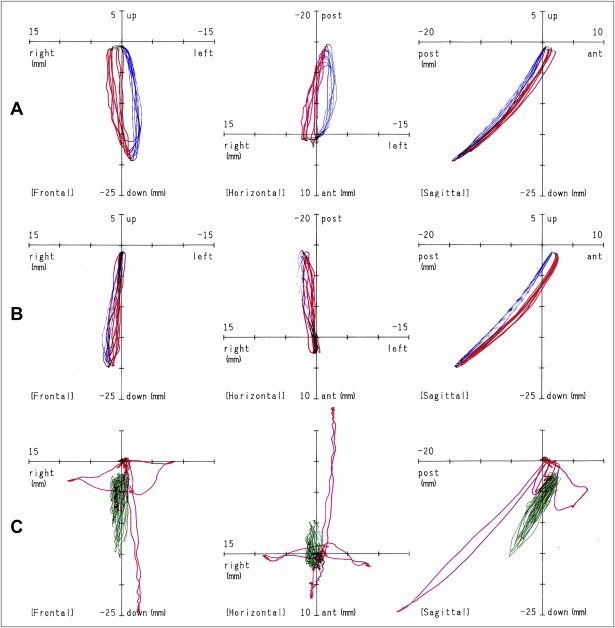
According to the results of an examination with a jaw trajectory recording system (Sirognathograph analyzing system; Tokyo Dental, Tokyo, Japan), the jaw movement paths during mastication were functionally normal ( Fig 4 , A and B ). However, the anterior displacement of the jaw movement area compared with the horizontal axis during speech suggested retropositioning of the mandible in the intercuspal position ( Fig 4 , C ).