Introduction
The purpose of this study was to examine the long-term skeletal and dental stability of mandibular symphyseal distraction osteogenesis (MSDO) with a tooth-borne and bone-borne hybrid distractor. To differentiate the effects of MSDO from the orthodontic movement and relapse, each phase of treatment was analyzed.
Methods
Twenty-five patients were included in the study, ranging in age from 12.0 to 30.9 years at the initiation of treatment (mean, 15.8 ± 4.8 years). Of this group, 16 patients were recalled at a mean of 7.5 ± 0.9 years (range, 6.3-9.6 years) after distraction for long-term analysis of skeletal and dental changes. Orthodontic records were taken at 5 times: T1, pretreatment; T2, predistraction; T3, postdistraction; T4, posttreatment, and T5, postretention. The data were statistically analyzed by using repeated-measures analysis of variance (ANOVA).
Results
There were significant increases in all interdental transverse measurements except the mandibular intersecond molar distance from T1 to T4. The largest overall expansion was achieved between the mandibular second premolars (4.32 ± 0.60 mm), followed by the interfirst premolar (3.44 ± 0.44 mm), the interfirst molar (2.60 ± 0.65 mm), and the intercanine (1.87 ± 0.44 mm) widths. The overall amount of transverse dental expansion was substantially less when analyzed from the time of the mandibular symphyseal osteotomy to posttreatment (T2-T4). From T3 to T4, there were significant decreases between the mandibular intersecond premolars (−3.10 ± 0.52 mm), interfirst premolars (−3.90 ± 0.35 m), intercanines (−4.47 ± 0.38 mm), and intercentral incisors (−5.60 ± 0.32 mm). There were no significant changes in bicondylar, bigonial, and biantigonial widths. At the long-term follow-up, there were no significant changes in the interdental or skeletal measurements between T4 and T5, except for interincisor apices. The irregularity index significantly decreased during the orthodontic treatment but significantly increased in the long-term follow-up period (T4-T5). After the MSDO, T3 to T5, the results indicated symphyseal basal bone skeletal stability.
Conclusions
The results indicate that the expansion of the mandibular arch with MSDO and conventional orthodontic mechanics produces no statistically significant transverse changes from posttreatment to long-term follow-up. The risks of using a surgical procedure and MSDO to achieve additional expansion should be evaluated by the clinician and compared with more traditional orthodontic methods.
Finding a stable and reliable method for mandibular widening has been a challenge in orthodontics and oral surgery for nearly a century. An orthodontist must balance esthetics with the requirement of long-term stability, since many treatments have a high rate of relapse. Mandibular arch form and mandibular intercanine width often restrict the amount of maxillary expansion, causing large buccal corridors. Contemporary orthodontists need a mandibular arch treatment that can deliver stability, periodontal health, and an esthetic result to their patients.
The correction of various mandibular dental space deficiencies is often accomplished via mandibular dental expansion, extraction, reproximation, or dental proclination. The stability of these treatments is often unpredictable and can result in negative side effects. Mandibular dental expansion tends to relapse toward the initial intercanine width and arch shape. Extraction treatment might adversely affect the patient’s profile, leave the patient with dark buccal corridors, and result in the subsequent reopening of the extraction spaces. Reproximation is limited by enamel thickness. Dental proclination can cause periodontal problems because of gingival recession. Aside from these complications, traditional treatments do not adequately address mandibular transverse skeletal issues. Although many orthodontists use rapid maxillary expansion during a patient’s treatment, mandibular arch widening has primarily been limited to transverse dental expansion.
Distraction osteogenesis is the biological process of new bone formation between bone segments that are gradually separated by incremental traction. Using these principles, Guerrero performed the first mandibular symphyseal distraction osteogenesis (MSDO) procedure on 10 patients, reported in 1990. He initially referred to this technique as rapid mandibular expansion. Using a tooth-borne distractor (connected to the first premolars and the first molars), he found that this technique was an adequate treatment for mandibular transverse problems. After the success of Guerrero’s technique, several clinical studies involving MSDO have been published to date. Recently, Gandini et al have supported MSDO as an alternative for borderline extraction patients. Our study further explores MSDO as a viable treatment option for narrow mandibular arches and crowding.
Although many case reports and a few clinical studies exist, there is a lack of large-scale prospective clinical studies documenting the long-term effects of MSDO. Previous studies have lacked the completeness of records or the proper timing of records. BeGole and Sadowsky stated that studies of long-term dental relapse have traditionally used measurements from study models taken at pretreatment, posttreatment, and a number of years postretention. The proper timing of records during and after orthodontic treatment is essential in distinguishing the effects of predistraction orthodontics, MSDO effects, postdistraction orthodontics, and postretention relapse. Published data regarding skeletal and dental stability after MSDO give sparse results and report relatively short follow-up periods. With records acquired from 25 patients at multiple time points during orthodontic treatment and a longer follow-up period, this study allowed for a better statistical analysis of each treatment phase. A hybrid (tooth-borne and bone-borne) distractor was used to improve dental stability. This was in response to previous reports of a disproportionate opening of the bony regenerate with tooth-borne distractors. The purposes of this study were to evaluate the skeletal and dental changes during each phase of MSDO and to analyze the long-term changes after the use of a hybrid distractor.
Material and methods
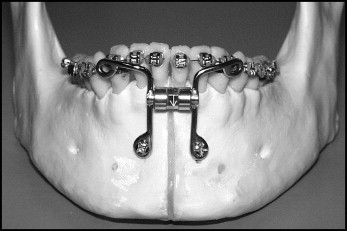
This study initially involved 31 patients who received MSDO via a custom-made hybrid distractor ( Fig 1 ). To minimize the effect of growth in this study, girls under 12 years of age and boys under 15 years of age at the initiation of treatment (T1) were removed (6 patients). Of the remaining 25, there were 7 male and 18 female patients, with a mean age of 15.8 ± 4.8 years (range, 12.0-30.9 years) at T1.
The patients received MSDO to treat at least 1 of the following dental or skeletal problems: mandibular crowding, maxillomandibular transverse deficiency, and unilateral or bilateral posterior scissors-bite (Brodie bite). Traditional orthodontic options and the surgical details of MSDO were presented to each patient. Before distraction, all patients received informed consent. In addition, the MSDO patients were informed that they were part of a research project and that any information related to this study might be used in scientific journals.
Standard orthodontic records were collected at 5 time points: T1, pretreatment; T2, predistraction; T3, postdistraction; T4, posttreatment; and T5, postretention. The T1 records were collected at a mean of 1.05 months before the start of treatment. The records acquired at these time points included clinical and temporomandibular examinations; study models; lateral, posteroanterior, and panoramic radiographs; and facial and intraoral photographs. Submental vertex radiographs were taken at T2 through T4.
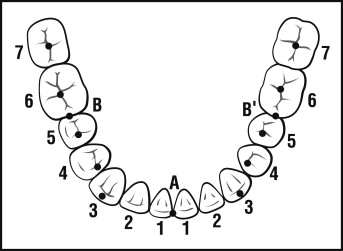
On the study models, 8 measurements were made in millimeters with digital calipers by using a total of 11 landmarks ( Fig 2 ): (1) intersecond molar width, the distance between the central fossae of the mandibular second molars; (2) interfirst molar width, the distance between the central fossae of the mandibular first molars; (3) intersecond premolar width, the distance between the mesial fossae of the mandibular second premolars; (4) interfirst premolar width, the distance between the mesial fossae of the mandibular first premolars; (5) intercanine width, the distance between the cusp tips of the mandibular canines; (6) intercentral incisor width, the distance between the mesial contact points of the mandibular central incisors; (7) arch length, the combined measurement of the distances from the mesial marginal ridge of the mandibular right first molar to the contact point of the mandibular central incisors and the mesial marginal ridge of the mandibular left first molar to the contact point of the mandibular central incisors; and (8) irregularity index, the sum of the displacement of the anatomic contact points of the 6 mandibular anterior teeth as described by Little et al.
On each lateral cephalometric radiograph, 1 angular measurement in degrees was made by using 4 landmarks: the mandibular incisor-mandibular plane angle, the angle between the mandibular plane (gonion-menton) and the long axis of the mandibular incisor (incisal tip to the incisal apex).
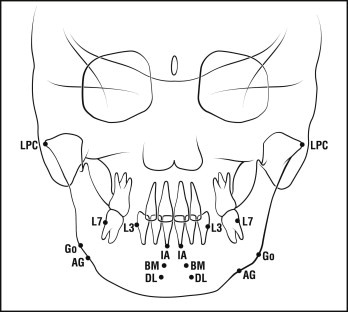
On the posteroanterior cephalometric radiograph, 8 measurements in millimeters were made by using 16 landmarks ( Fig 3 ): (1) bicondylar width, the distance between the right and left lateral condylar poles; (2) bigonial width, the distance between the right and left gonions; (3) antigonial width, the distance between the right and left antigonions; (4) intersecond molar width, the distance between the lateral cementoenamel junctions of the right and left second molars; (5) intercanine width, the distance between the lateral cementoenamel junctions of the right and left canines; (6) intercentral incisor apical width, the distance between the apices of the right and left central incisors; (7) interbone marker width, the distance between the right and left bone markers; and (8) interdistractor loop width, the distance between the right and left distractor loops.
On the submental vertex radiograph, 1 measurement was made by using 2 landmarks between T2 and T4. Bicondylar width was determined by the measurement in millimeters between the right and left lateral poles of the condyles.
At T1, all 25 patients received comprehensive predistraction orthodontic treatment. Initially, full orthodontic appliances were placed in the maxillary arch to achieve an ideal arch shape, thereby eliminating any preexisting maxillary crowding and incisor protrusion. The modified maxillary arch shape served as a template for the treatment of the mandibular arch. Of the 25 patients, 20 received predistraction rapid maxillary expansion, and 3 adult patients received concomitant surgically assisted rapid maxillary expansion. During this phase, orthodontic appliances were placed on most or all of the mandibular teeth. After selecting an osteotomy site, brackets on the teeth adjacent to the osteotomy were angulated distally to create root divergence and thus a safer procedure. In 23 patients (92%), the osteotomy was performed between the central incisors. In 2 patients (8%), severe crowding in the central incisor region prevented adequate root divergence. The osteotomy in these 2 patients was performed between the central and lateral incisors.
In cases with anterior crowding, the osteotomy site was placed as close to the crowding as possible. In all patients, a figure-8 ligation wire was extended from the tooth adjacent to the osteotomy site to the ipsilateral canine. Before the osteotomy, an archwire was placed from the first or second molar to the contralateral molar.
All 25 patients receiving MSDO were treated by the same oral and maxillofacial surgeon (J.C.W.). Intravenous sedation was administered to each patient in a semireclined position. Local anesthesia was also used for hemostasis and postoperative pain management. We used the technique for MSDO as described by Guerrero and Bell. A horizontal incision was made with a number 15 blade approximately 8 mm below the mucogingival reflection extending from the right canine to the left canine. The incision was carried through the mucosa, submucosa, muscle, and periosteum. A full-thickness subperiosteal flap was elevated inferiorly, and the symphysis was completely degloved, including the inferior border of the mandible.
The distractor consisted of a modified expansion screw (SUPERscrew, SUPERspring, Highwood, Ill). The appliance was placed adjacent to the anterior teeth and secured to the bone of the symphysis with 2 bicortical screws (2 × 10 mm) through the loops of the inferior distractor arms. After the distractor was checked for proper positioning, the superior loops were secured to the canine (or other designated tooth) on either side of the planned osteotomy with 24-gauge stainless steel circumdental wire and light-cured composite. A tunnel was made in the mandibular midline beneath the attached gingiva and continued superiorly to the gingival margin. The midline of the mandibular bone was scored vertically with a bone bur from the mandibular incisor apices to the crestal bone. A reciprocating bone saw was then used to create a vertical midline osteotomy cut from the inferior border of the mandible up to the apices of the mandibular incisors. A narrow osteotome and a mallet were used to complete the cut in the scored bone between the roots of the central incisors (or between alternate teeth if a step osteotomy was performed). The 2 halves of the mandible were then mobilized.
After the osteotomy, complete mobilization of the hemi-mandibles was verified by opening the distractor screw to a width of 2.0 mm. The distractor screw was subsequently closed 2.0 mm, and soft-tissue closure was completed. Thus, there was no intentional expansion of the hemi-mandilbes at the time of the midsymphyseal osteotomy. The mean latency period before distraction was 7.7 ± 1.7 days.
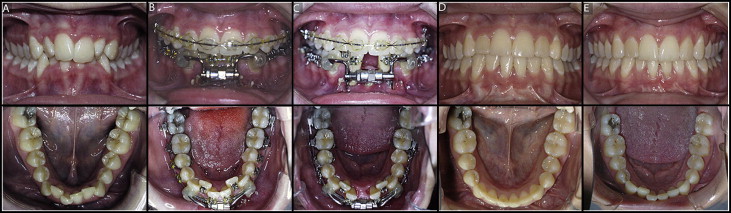
Predistraction records (T2) were collected immediately after the latency period. In addition to the previously described records, a digital caliper was used to measure the distractor screw length. The archwire was cut and cinched at the osteotomy site before the distractor screw was activated. The patients were instructed how to properly make 2 turns (0.5 mm each) per day for a total distraction rate of 1.0 mm per day. An instruction card, which included a daily log, was also provided to each patient. Patients were monitored every 2 to 4 days until adequate space had been created to definitively eliminate the crowding and protrusion. At this time, the distractor locknut was secured to prevent back turning of the distractor screw. A denture tooth was then placed in the distraction site and secured to the adjacent teeth with a sectional wire as an esthetic consideration. The mean time between T2 and T3 was 12.1 ± 3.6 days (range, 8-27 days). Postdistraction records (T3) were taken at this time. The distractor was removed at 3.0 ± 1.0 months after distraction, and postdistraction orthodontics were initiated to complete the treatment ( Fig 4 ). The retention protocol included removable maxillary and mandibular Hawley retainers; no patient received a fixed retainer.
Statistical analysis
The changes in the measurements between the dental and skeletal landmarks during treatment were statistically analyzed by using mixed-model repeated-measures analysis of variance (ANOVA) (version 9.1; SAS, Cary, NC). The differences were calculated with the following time period comparisons: pretreatment to predistraction (T1-T2), predistraction to postdistraction (T2-T3), postdistraction to posttreatment (T3-T4), posttreatment to postretention (T4-T5), pretreatment to posttreatment (T1-T4), and pretreatment to postretention (T1-T5). The Tukey-Kramer adjustment was used to control for the multiple comparisons of the skeletal and dental landmarks. A significance level of P <0.05 was set for all analyses.
To test intraexaminer and interexaminer reliability, the study model and cephalometric measurements were repeated for a subsample of 6 patients. The systematic error for the study models were not statistically significant, and the typical errors for the study model data ranged from 0.17 mm for intraexaminer measurements to 0.23 mm for interexaminer measurements. The systematic errors for the cephalometric measurements were not statistically significant, and the typical error ranged from 0.21 mm for interexaminer measurements to 0.52 mm for intraexaminer measurements.
Results
The treatment phases and time points (T1-T5) in this study are illustrated in Figure 5 . The descriptive data measurements for the study models; the posteroanterior, lateral, and submental vertex radiographs; and the distractor screw measurements are presented in Table I . Table II shows the statistical comparisons ( P values) of these variables between each time point.
| T1 | T2 | T3 | T4 | T5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment | Predistraction | Postdistraction | Posttreatment | 5–year follow-up | ||||||
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | |
| Study models | ||||||||||
| Second molar (mm) | 44.31 | 2.54 | 43.68 | 2.08 | 45.58 | 2.78 | 46.11 | 2.49 | 43.47 | 1.93 |
| First molar (mm) | 38.33 | 2.58 | 38.70 | 2.61 | 41.84 | 2.32 | 40.92 | 2.01 | 41.65 | 1.82 |
| Second premolar (mm) | 31.50 | 2.59 | 34.35 | 1.88 | 38.92 | 2.08 | 35.82 | 1.49 | 35.58 | 1.51 |
| First premolar (mm) | 26.37 | 1.92 | 28.37 | 1.40 | 33.62 | 1.39 | 29.81 | 1.07 | 29.57 | 1.55 |
| Canine (mm) | 24.06 | 1.98 | 24.76 | 1.66 | 30.44 | 1.62 | 25.96 | 0.93 | 25.35 | 1.16 |
| Central incisor (mm) | −0.28 | 0.48 | −0.14 | 0.61 | 5.60 | 1.56 | 0.00 | 0.00 | 0.00 | 0.00 |
| Irregularity index (mm) | 7.44 | 2.96 | 0.73 | 0.36 | 2.37 | 1.42 | ||||
| Arch length (mm) | 57.70 | 3.78 | 59.75 | 2.88 | 60.22 | 2.34 | 58.85 | 1.67 | ||
| PA cephalometric radiograph | ||||||||||
| Bigonion (mm) | 96.71 | 3.78 | 98.33 | 7.36 | 97.67 | 6.99 | 94.95 | 7.27 | 95.68 | 7.04 |
| Biantigonion (mm) | 85.37 | 5.10 | 85.76 | 6.02 | 86.06 | 6.06 | 85.47 | 5.57 | 86.11 | 5.46 |
| Bicondylar width (mm) | 130.92 | 5.41 | 124.30 | 8.80 | 125.89 | 6.55 | 127.79 | 4.60 | 126.66 | 6.08 |
| Bone markers (mm) | 6.36 | 1.18 | 11.47 | 1.45 | 11.18 | 1.63 | 12.28 | 1.94 | ||
| Distractor loops (mm) | 10.01 | 1.02 | 15.67 | 1.44 | ||||||
| Interincisor apices (mm) | 3.47 | 0.96 | 7.09 | 1.70 | 12.15 | 1.88 | 4.39 | 1.08 | 5.27 | 0.90 |
| Intercanines (mm) | 30.22 | 1.54 | 31.20 | 1.17 | 36.81 | 1.61 | 33.43 | 1.07 | 34.42 | 1.19 |
| Intersecond molars (mm) | 66.53 | 2.92 | 62.03 | 3.10 | 64.36 | 3.09 | 63.29 | 2.86 | 63.94 | 2.40 |
| Distractor screw (mm) | 15.31 | 0.34 | 21.64 | 1.03 | ||||||
| Lateral cephalometric radiograph | ||||||||||
| L1-MP (°) | 91.30 | 6.72 | 93.83 | 6.84 | 94.75 | 6.25 | 93.70 | 7.43 | 91.64 | 7.88 |
| Clinical measurement | ||||||||||
| Distractor screw (mm) | 14.76 | 0.30 | 21.13 | 0.91 | ||||||
| SMV cephalometric radiograph | ||||||||||
| Bicondylar width (mm) | 110.65 | 19.19 | 110.38 | 18.49 | 112.36 | 19.91 | ||||
| Change (T2-T1) | Change (T3-T2) | Change (T4-T3) | Change (T5-T4) | Change T4-T1) | Change (T5-T1) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | P | Sig | Mean | SE | P | Sig | Mean | SE | P | Sig | Mean | SE | P | Sig | Mean | SE | P | Sig | Mean | SE | P | Sig | |
| Study models | ||||||||||||||||||||||||
| Second molar (mm) | −0.63 | 0.85 | 0.9475 | NS | 1.89 | 0.88 | 0.2020 | NS | 0.53 | 0.77 | 0.9576 | NS | 0.36 | 0.68 | 0.9837 | NS | 1.80 | 0.74 | 0.1156 | NS | 2.17 | 0.71 | 0.0232 | ∗ |
| First molar (mm) | 0.38 | 0.74 | 0.9866 | NS | 3.14 | 0.71 | 0.0002 | ‡ | −0.92 | 0.62 | 0.5802 | NS | 0.73 | 0.61 | 0.7515 | NS | 2.60 | 0.65 | 0.0012 | † | 3.33 | 0.69 | <0.0001 | ¶ |
| Second premolar (mm) | 2.86 | 0.64 | 0.0002 | ‡ | 4.56 | 0.57 | <0.0001 | ¶ | −3.10 | 0.52 | <0.0001 | ¶ | −0.24 | 0.48 | 0.9876 | NS | 4.32 | 0.60 | <0.0001 | ¶ | 4.08 | 0.64 | <0.0001 | ¶ |
| First premolar (mm) | 2.01 | 0.48 | 0.0005 | ‡ | 5.25 | 0.40 | <0.0001 | ¶ | −3.90 | 0.35 | <0.0001 | ¶ | −0.24 | 0.44 | 0.9823 | NS | 3.44 | 0.44 | <0.0001 | ¶ | 3.20 | 0.55 | <0.0001 | ¶ |
| Canine (mm) | 0.67 | 0.52 | 0.7028 | NS | 5.68 | 0.47 | <0.0001 | ¶ | −4.47 | 0.38 | <0.0001 | ¶ | −0.62 | 0.35 | 0.3891 | NS | 1.87 | 0.44 | 0.0004 | ‡ | 1.26 | 0.49 | 0.0861 | NS |
| Central incisor (mm) | 0.14 | 0.16 | 0.9044 | NS | 5.75 | 0.34 | <0.0001 | ¶ | −5.60 | 0.32 | <0.0001 | ¶ | 0.00 | 0.00 | 0.9981 | NS | 0.28 | 0.10 | 0.0327 | ∗ | 0.28 | 0.10 | 0.0327 | ∗ |
| Irregularity index (mm) | 1.64 | 0.36 | <0.0001 | ¶ | −6.71 | 0.60 | <0.0001 | ¶ | −5.08 | 0.69 | <0.0001 | ¶ | ||||||||||||
| Arch length (mm) | 2.05 | 0.96 | 0.1481 | NS | −1.37 | 0.63 | 0.1350 | NS | 2.52 | 0.89 | 0.0289 | ∗ | 1.15 | 0.86 | 0.5464 | NS | ||||||||
| PA cephalogram | ||||||||||||||||||||||||
| Bigonion (mm) | 1.52 | 2.63 | 0.9782 | NS | −0.66 | 2.03 | 0.9975 | NS | −0.72 | 2.02 | 0.9965 | NS | −1.27 | 2.33 | 0.9822 | NS | 0.14 | 2.62 | 1.0000 | NS | −1.13 | 2.84 | 0.9946 | NS |
| Biantigonion (mm) | 0.39 | 3.18 | 0.9999 | NS | 0.30 | 1.71 | 0.9998 | NS | −0.59 | 1.65 | 0.9963 | NS | 0.65 | 1.76 | 0.9961 | NS | 0.10 | 3.15 | 1.0000 | NS | 0.75 | 3.24 | 0.9994 | NS |
| Bicondylar width (mm) | −6.62 | 4.33 | 0.5472 | NS | 1.60 | 2.54 | 0.9700 | NS | 1.89 | 1.89 | 0.8535 | NS | −1.12 | 2.00 | 0.9802 | NS | −3.13 | 3.98 | 0.9334 | NS | −4.25 | 4.18 | 0.8463 | NS |
| Bone markers (mm) | 5.12 | 0.43 | <0.0001 | ¶ | −0.29 | 0.52 | 0.9407 | NS | 1.11 | 0.71 | 0.4054 | NS | ||||||||||||
| Distractor loops (mm) | 5.66 | 0.36 | <0.0001 | ¶ | ||||||||||||||||||||
| Interincisor apices (mm) | 3.61 | 0.65 | <0.0001 | ¶ | 5.07 | 0.51 | <0.0001 | ¶ | −7.77 | 0.43 | <0.0001 | ¶ | 0.88 | 0.31 | 0.0438 | ∗ | 0.91 | 0.60 | 0.5433 | NS | 1.80 | 0.60 | 0.0281 | ∗ |
| Intercanines (mm) | 0.99 | 0.92 | 0.8187 | NS | 5.61 | 0.40 | <0.0001 | ¶ | −3.39 | 0.39 | <0.0001 | ¶ | 0.99 | 0.37 | 0.0661 | NS | 3.21 | 0.91 | 0.0061 | † | 4.20 | 0.94 | 0.0002 | ‡ |
| Intersecond molars (mm) | −4.50 | 1.80 | 0.0997 | NS | 2.33 | 0.88 | 0.0687 | NS | −1.07 | 0.84 | 0.7089 | NS | 0.65 | 0.83 | 0.9329 | NS | −3.24 | 1.78 | 0.3696 | NS | −2.59 | 1.79 | 0.6013 | NS |
| Distractor screw (mm) | 6.33 | 0.24 | <0.0001 | ¶ | ||||||||||||||||||||
| Lateral cephalogram | ||||||||||||||||||||||||
| L1-MP (°) | 2.53 | 1.94 | 0.6870 | NS | 0.92 | 1.89 | 0.9886 | NS | −1.05 | 1.96 | 0.9834 | NS | −2.06 | 2.47 | 0.9197 | NS | 2.40 | 2.00 | 0.7527 | NS | 0.34 | 2.38 | 0.9999 | NS |
| Clinical measurement | ||||||||||||||||||||||||
| Distractor screw (mm) | 6.37 | 0.28 | <0.0001 | ¶ | ||||||||||||||||||||
| SMV cephalogram | ||||||||||||||||||||||||
| Bicondylar width (mm) | −0.26 | 5.44 | 0.9987 | NS | 1.97 | 5.68 | 0.9357 | NS | ||||||||||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


