Beckwith-Wiedemann syndrome (BWS) is a congenital growth disorder. Children born with BWS develop enlarged organs, including the tongue, a large body, and other signs. A woman with BWS was treated and followed for 30 years. Treatment consisted of tongue reduction, orthopedic and orthodontic treatment, orthognathic surgery, and retention. The patient was first treated when she was 5 years old. Her original orthodontic problems included macroglossia, anterior open bite, anterior crossbite, and a skeletal Class III jaw relationship caused by significant mandibular protrusion. The jaw-base relationships did not improve in the early preadolescent period after phase 1 of orthodontic treatment with a vertical chincap. With the growth spurt accompanying puberty, she developed a severe skeletal Class III jaw relationship and a constricted maxillary arch. Surgically assisted rapid maxillary expansion was performed at 23 years of age to correct the severe discrepancy between the maxillary and mandibular dental arch widths. Then, at 26 years, a LeFort I osteotomy, a horseshoe osteotomy, a bilateral sagittal split ramus osteotomy, and genioplasty were performed after presurgical orthodontic treatment with extraction of the mandibular first molars. Both the facial profile and the occlusion were stable after 6 years of retention. This case report discusses the result of long-term observation of a patient with BWS who underwent tongue reduction, early orthodontic treatment, and surgical-orthodontic treatment.
Beckwith-Wiedemann syndrome (BWS) is caused by mutation or deletion of an imprinted domain in the chromosomal region 11p15.5, which harbors the H19 , p57 ( KIP2 ), and LIT1 genes. The prevalence of BWS is estimated to be 1 in 13,700 births. It is characterized by exomphalos (80%), macroglossia (97%), and somatic gigantism (88%) resulting from overgrowth during the latter half of gestation and during infancy. Previous studies have shown that patients with BWS have protrusion of the mandible with an abnormally widely dilated gonial angle, increased mandibular length, anterior open bite, and a wide dental arch, primarily as a consequence of the macroglossia.
Some reports have suggested that early diagnosis and treatment of the oral manifestations of BWS could reduce the associated aberrant craniofacial development and growth. Although there have been some reports concerning the longitudinal craniofacial changes in BWS patients treated with tongue reduction and orthodontic treatment, the long-term outcome of surgical-orthodontic treatment with tongue reduction remains unclear. We herein report on a patient with BWS showing a good prognosis and long-term stability after tongue reduction, orthopedic and orthodontic treatment, and orthognathic surgery.
Diagnosis and etiology
A Japanese girl, 5 years 10 months of age, was referred to the orthodontic department of the Tokyo Medical and Dental University Dental School Hospital. Her chief complaint was a severe anterior crossbite with an open bite. She was born by Caesarean delivery at the normal gestational age; her birth weight was 4.324 g. She had been diagnosed with BWS at birth and had undergone surgery for exomphalos immediately after birth. Furthermore, she had a medical history of stomach volvulus and ileus and had undergone tongue reduction surgery when she was 2 years 7 months of age at another medical school hospital.
At the first medical examination, she had no significant systemic or orthodontic family history. Her facial profile was concave with chin protrusion and long lower facial height ( Fig 1 ). The tongue was long enough to reach the mentum, and abnormal earlobe creases were observed ( Fig 1 ). She had an anterior open bite with an overjet of −9.0 mm and an overbite of −3.0 mm, and a constricted width of the maxillary dental arch with the high arched palate resulting in a total crossbite ( Figs 1 and 2 ). The terminal plane was a mesial step type on both sides ( Figs 1 and 2 ).
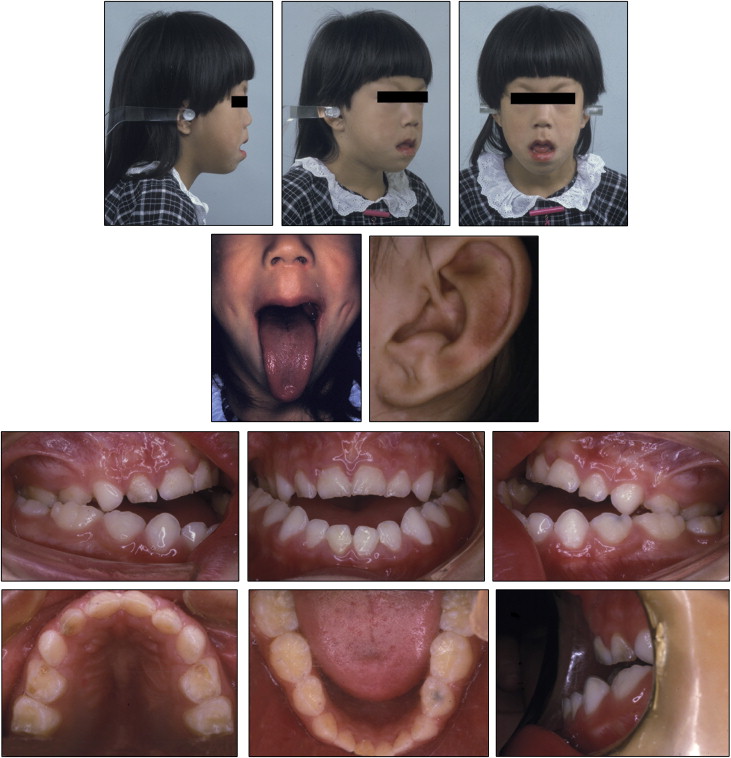
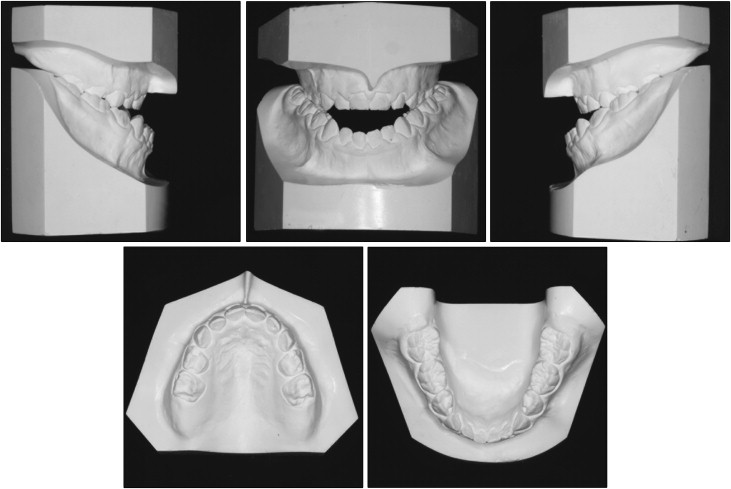
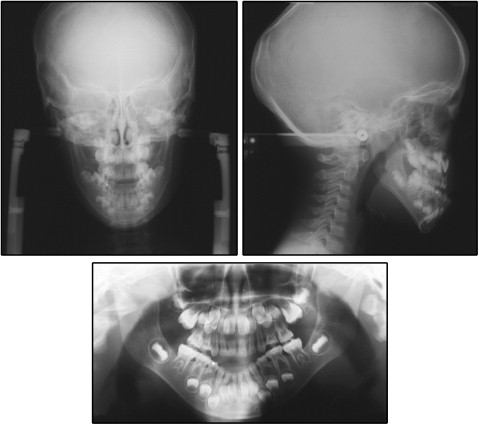
From the results of the lateral cephalometric analysis, the patient was proven to have a skeletal Class III jaw relationship with severe mandibular protrusion (ANB, 0.3°; SNB, 82.3°), long mandibular body length (Go-Pog, 75.5 mm), and a high mandibular plane angle (MP-FH, 42.7°) with an obtuse gonial angle (145.0°) ( Fig 3 , Table ). These data deviated greatly from the normative values for Japanese girls of corresponding age. This patient received a diagnosis of mandibular prognathism with a skeletal Class III jaw relationship, a high mandibular plane angle, a total crossbite, and an anterior open bite. The etiology of the severe skeletal Class III malocclusion with open bite was believed to be hyperplasia of the tongue, a phenotype associated with BWS.
| Measurement | Pretreatment | Before phase 2 | Posttreatment | 6 years postretention | Normative value ∗ | |
|---|---|---|---|---|---|---|
| Mean | SD | |||||
| Age | 5 y 10 mo | 20 y 7 mo | 28 y 4 mo | 34 y 4 mo | ||
| Angular (°) | ||||||
| ANB | 0.3 | −3.4 | 3.7 | 3.7 | 3.4 | 1.8 |
| SNA | 82.7 | 84.7 | 87.5 | 87.5 | 82.3 | 3.5 |
| SNB | 82.3 | 88.1 | 83.9 | 83.9 | 78.9 | 3.5 |
| MP-FH | 43.7 | 45.0 | 42.7 | 42.7 | 28.8 | 5.2 |
| Gonial angle | 145.0 | 150.6 | 143.1 | 143.1 | 122.2 | 4.6 |
| U1-SN | 87.9 | 104.3 | 94.8 | 95.7 | 104.5 | 5.6 |
| L1-MP | 77.7 | 72.8 | 63.6 | 63.6 | 96.3 | 5.8 |
| Convexity | 3.8 | −4.8 | 7.5 | 7.5 | 7.6 | 5.0 |
| Interincisal angle | 144.5 | 131.8 | 153.0 | 152.1 | 124.1 | 7.6 |
| Occlusal plane | 30.5 | 14.6 | 15.2 | 15.1 | 11.4 | 3.6 |
| Linear (mm) | ||||||
| Ar-Go | 33.4 | 48.1 | 47.0 | 48.1 | 41.3 | 5.0 |
| Go-Pog | 75.5 | 96.7 | 87.2 | 88.0 | 78.0 | 4.7 |
| Overjet | −9.0 | −12.0 | 4.0 | 3.0 | 1.0 | 1.5 |
| Overbite | −3.0 | −12.0 | 4.0 | 3.0 | 1.0 | 1.5 |
∗ Means and standard deviations of normally developed Japanese women.
Treatment objectives
The treatment objectives for this patient included accomplishing the following: (1) correct the severe skeletal Class III jaw relationship caused by the excessive mandibular growth; (2) correct the anterior open bite and the total crossbite, and establish ideal overjet and overbite; (3) achieve an acceptable occlusion with a good functional Class I occlusion; (4) achieve a favorable facial profile; and (5) maintain the stability of her occlusion during retention for a long term.
Treatment objectives
The treatment objectives for this patient included accomplishing the following: (1) correct the severe skeletal Class III jaw relationship caused by the excessive mandibular growth; (2) correct the anterior open bite and the total crossbite, and establish ideal overjet and overbite; (3) achieve an acceptable occlusion with a good functional Class I occlusion; (4) achieve a favorable facial profile; and (5) maintain the stability of her occlusion during retention for a long term.
Treatment alternatives
There have been some controversies in active phase 1 orthodontic and orthopedic approaches to patients displaying severe skeletal Class III problems. Some authors reported minimal or no effects. On the other hand, others have reported that phase 1 orthodontic and orthopedic treatment for these patients might be recommended to resolve skeletal problems in the transverse, vertical, and sagittal dimensions. These effects sometimes contribute to relieving the difficulty of phase 2 of orthodontic treatment, including orthognathic surgery after pubertal growth. On the basis of this information, we performed early phase 1 orthodontic and orthopedic treatment for our patient in the hope of a better prognosis.
Regarding the method of orthognathic surgery for our patient with a severe skeletal Class III condition, the options were isolated mandibular setback or bimaxillary orthognathic surgery. Because of her extremely large tongue and concave profile with mandibular protrusion, we opted for bimaxillary surgery rather than isolated mandibular setback, LeFort I osteotomy combined with horseshoe osteotomy, and genioplasty to achieve the appropriate volume of the oral cavity and a favorable profile.
We chose surgically assisted rapid maxillary expansion (RME) because of her age at the time of phase 2 treatment, the damage of periodontal tissues from the lateral expansion of the maxillary dentition, and the amount of expansion required to establish harmonic maxillary and mandibular dental arch widths.
Treatment progress
A vertical chincap was applied at 6 years 1 month of age and continued for approximately 10 years as phase 1 orthodontic treatment. At the beginning of phase 2 treatment, the mandibular first molars on both sides were extracted under local anesthesia. The decision to extract these teeth was made for maximal restoration of her open bite during preoperative orthodontic treatment by mesial driving of the mandibular second and third molars.
Edgewise appliances were placed on the mandibular dental arch at 20 years 10 months of age. Leveling was performed in the mandibular dental arch for 7 months, and space closure in the mandibular dental arch was performed for 2 years 4 months. At 23 years 10 months of age, the constricted maxillary dental arch was expanded by 8.5 mm (from 40.5 to 49.0 mm) between the maxillary first molars with surgically assisted RME. A lingual arch with a palatal bar was placed for 3 months to retain the width of the maxillary dentition, and then edgewise appliances were placed on the maxillary dental arch. At 1 year 3 months after the surgically assisted RME, a quad-helix appliance was placed for 3 months on the maxillary dentition for lateral reexpansion. The duration of the preoperative orthodontic treatment was 7 years. Then a LeFort I osteotomy combined with a horseshoe osteotomy, a bilateral sagittal split ramus osteotomy, and genioplasty were performed under general anesthesia at 26 years 9 months of age. All surgical orthodontic procedures were performed in the oral surgery department of the Tokyo Medical and Dental University Dental School Hospital. The total postoperative orthodontic treatment time was 1 year 5 months, and the overall active orthodontic treatment period was 8 years 4 months. After removal of the edgewise appliances, circumferential and Hawley-type retainers were applied on the maxillary and mandibular dentitions, respectively. The observation term of the retention period was almost 6 years 1 month.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


