Armamentarium
|
History of the Procedure
Soft tissue repair of the face originated around 600 bc , when Sushruta Samita of India described nasal reconstruction with a cheek flap. As surgery evolved, our reconstructive options multiplied into a prolific body of literature.
Reconstructive flaps are definitive procedures, which often benefit from adjustment or revision. They may compromise adjacent tissue with scars and may live or die depending on the (1) condition of the patient, (2) viability of adjacent skin, (3) choice of flap, and (4) timing of repair.
Patient-specific conditions can alter the surgeon’s choice for reconstruction. For example, smoking and diabetes may impact the viability of a flap. Other considerations include prior radiation therapy, previous surgery around the planned operative area, collagen-vascular disease, anticoagulants, and immunosuppression.
The viability of adjacent skin heavily influences choices. Traumatic wounds often have crushed borders. Gunshots produce areas of hyperemia and stasis of the tissue. Prior scars and radiation often limit flap mobility and viability. Other reconstructive options that might be considered include doing nothing, which allows healing via secondary intention, and split or full thickness skin grafting. These options may be superior for traumatic avulsion wounds.
Healing by secondary intention, rather than primary wound closure, may be a superior choice when shrinkage of the wound circumference would be beneficial. Certain areas can heal nearly imperceptibly and without distortion, such as the periauricular area, the posterior scalp, and small medial canthal defects. Secondary healing necessitates patient motivation and reliability, as well as a commitment to home care of the open wound. This is a relatively painless option, provided the wound is covered. Secondary healing can also be a useful temporary option for wound management. There is still opportunity at any time during the secondary epithelialization process to intervene with a flap or graft.
Grafting the defect provides a less elegant wound closure that may be a better option, depending on the surgeon’s goals. Grafting the defect reduces wound size; full thickness grafts shrink much less than split thickness or meshed grafts. Advantages to grafting include the elimination of complex wound care, simplification of closure in compromised patients, reduction in future flap size, and observation for possible tumor recurrence.
History of the Procedure
Soft tissue repair of the face originated around 600 bc , when Sushruta Samita of India described nasal reconstruction with a cheek flap. As surgery evolved, our reconstructive options multiplied into a prolific body of literature.
Reconstructive flaps are definitive procedures, which often benefit from adjustment or revision. They may compromise adjacent tissue with scars and may live or die depending on the (1) condition of the patient, (2) viability of adjacent skin, (3) choice of flap, and (4) timing of repair.
Patient-specific conditions can alter the surgeon’s choice for reconstruction. For example, smoking and diabetes may impact the viability of a flap. Other considerations include prior radiation therapy, previous surgery around the planned operative area, collagen-vascular disease, anticoagulants, and immunosuppression.
The viability of adjacent skin heavily influences choices. Traumatic wounds often have crushed borders. Gunshots produce areas of hyperemia and stasis of the tissue. Prior scars and radiation often limit flap mobility and viability. Other reconstructive options that might be considered include doing nothing, which allows healing via secondary intention, and split or full thickness skin grafting. These options may be superior for traumatic avulsion wounds.
Healing by secondary intention, rather than primary wound closure, may be a superior choice when shrinkage of the wound circumference would be beneficial. Certain areas can heal nearly imperceptibly and without distortion, such as the periauricular area, the posterior scalp, and small medial canthal defects. Secondary healing necessitates patient motivation and reliability, as well as a commitment to home care of the open wound. This is a relatively painless option, provided the wound is covered. Secondary healing can also be a useful temporary option for wound management. There is still opportunity at any time during the secondary epithelialization process to intervene with a flap or graft.
Grafting the defect provides a less elegant wound closure that may be a better option, depending on the surgeon’s goals. Grafting the defect reduces wound size; full thickness grafts shrink much less than split thickness or meshed grafts. Advantages to grafting include the elimination of complex wound care, simplification of closure in compromised patients, reduction in future flap size, and observation for possible tumor recurrence.
Indications for the Use of the Procedure
Correct timing of any wound repair influences success. Two concepts are noteworthy.
First, immediate flap coverage for either trauma or tumor resection is rarely emergently indicated. Exceptions to this standard are limited to unusual circumstances such as covering the brain or a major vessel. Open wounds may be left unrepaired for extended times, as long as debris and bacteria are removed and the wound is covered. Appropriate coverage may consist of ointment or a simple bandage.
Second, delay of wound repair may offer opportunities to increase flap success. Delay maneuvers before final repair can enhance adjacent tissue viability, shrink defect size, and allow an augmented vascular base of granulation tissue. Delay allows the surgeon to carefully plan the approach. Surgical delays (e.g., limited flap lifting or tissue expansion) can precondition the flap and promote neovascularization and angiogenesis.
The surgeon should develop a schematic progression of reconstructive possibilities. This progression begins by mentally trying to close any wound by direct advancement of tissue in or near resting skin tension lines if possible. Repositioning of end triangles and harnessing tissue creep modifications may be necessary. After the advancement flap has been considered, possible rotational flaps are evaluated. Finally, transposition and interpolation flaps are assessed. Obviously, there are locations on the face (e.g., the lips and nose) where a specific type of flap works optimally.
Flap Concepts
Whereas early facial defect closures were directed toward “filling the hole,” more elegant and aesthetic solutions now allow opportunities to create a natural harmonious result. The fundamental concepts of local flap reconstruction are listed in Box 95-1 .
- 1.
Consider flap mobility blood supply.
- 2.
Consider tension forces within the flap and the effects on or of local anatomy.
- 3.
Consider where excess tissue may be ultimately positioned.
- 4.
Consider allowable wound tension at closure and where any technical maneuvers may be reasonable.
- 5.
Consider flap incisions near topographic borders within relaxed skin tension lines (RSTLs) or hidden from obvious frontal views.
Anatomy
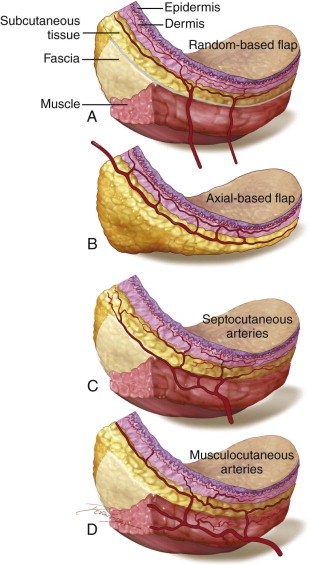
The most superficial layer of the skin is the epidermis. Beneath the epidermis, the dermis is subdivided into the superficial papillary and the deeper reticular layers.
There is both a superficial and deep intradermal vascular plexus, which typically runs parallel to the surface of the skin and provides nutrients to a large surface area. These vascular networks are extensive but by themselves cannot support tissue viability alone after significant tissue undermining is performed. The deeper, subdermal plexus lies beneath the dermis within the superficial subcutaneous tissue and plays a critical role in flap physiology. These vessels are often preserved in an advancing flap edge through the retention of a trace layer of fat on the undersurface of the tissue. A “random flap” depends upon this blood supply.
Deep to the network of intradermal plexuses are the larger caliber axial “named” vessels (i.e., superficial temporal artery). Axial vessels lie deep to the subcutaneous fat on the surface of the superficial fascia, roughly parallel to the skin surface. These vessels within the flap dramatically enhance vascularity, thus offering options for lengthening the flap without compromising viability (e.g., forehead and Abbe flaps).
Deeper interconnecting vessels, which are perpendicular to the skin surface, are musculocutaneous arteries. These vessels exit the muscle and enter the subcutaneous tissue to supply a smaller region of the skin. Collectively, the septocutaneous and musculocutaneous arteries contribute to a diffuse interconnecting vascular network of dermal and subdermal arteries that create some vascular redundancy in the skin ( Figure 95-1 ).
Flap Terminology
The Defect
A primary defect is any defect created by trauma or tumor. Direct advancement flaps close a primary defect by stretching the adjacent skin over the defect. When the elliptical advancement flap is ineffective, tissue must still be otherwise mobilized to fill the primary defect without undue tension. The use of additional incisions and maneuvers (e.g., backcuts) can allow tension-free closure.
A secondary defect is the defect that occurs as a result of movement of the flap and develops behind the advancing flap edge. Flap design compensates for the secondary defect by allowing the surgeon to close this defect as well. Sometimes the secondary defect is closed by dissipation of forces elsewhere or by grafting in an inconspicuous location.
Inherent Extensibility
Adequate skin mobility is partially attributable to skin extensibility (stretching of the elastic fibers). Low-tension closure minimizes scar widening, wound dehiscence, tissue ischemia, and anatomic distortion. On the face, tense closures can break down. This is less of a problem on the more forgiving forehead and scalp. There is generally more extensibility among older patients. A mid-cheek defect of only 1 cm may be the terminal limit of easy closure in an adolescent, 2.5 cm in a 40-year-old, and over 4 cm in a 75-year-old. On the face, no additional stretch/extensibility will be gained after 3 to 4 cm of undermining. Overstretching on the face will produce tears or striae, which can be permanent ( Figure 95-2 ).


Mechanical Creep
Mechanical creep is the tendency for any solid material to move slowly or deform under the influence of stress. Skin responds no differently. Skin held at a constant tension may require less tension over time. A common characteristic of mechanical creep can be observed following a tightly closed avulsive forehead wound. After a few days, the tissue relaxes.
Three principles of mechanical creep may be functionally garnered to help close tight flaps: presuturing, cyclic loading, and deep scoring of tense tissues:
- •
Presuturing pulls tissues together and can be employed from days to only minutes prior to attempting wound closure. This technique can gain millimeters to centimeters of additional length. Commercially available instrumentation is available, but the use of sutures can achieve the same result.
- •
Cyclic loading performs the same purpose at surgery. The surgeon cyclically loads the tissue with skin hooks or by inflating a catheter balloon to stretch it. Each cycle extracts additional stretch or creep from the tissue, yielding greater overall length.
- •
Deep tissue scoring, particularly of the galea, can also augment mechanical creep.
Biologic Creep
Biologic creep is a slow, methodic stretching of the skin, producing new skin. This physiologic property is reflected in severe obesity, pregnancy, and skin expansion.
Surgical Flap Delay
Blood supply to the terminal portion of a random flap (flaps dependent on the subdermal plexus) is not as much a function of width, but rather one of length. Flap length can be limited by vascular compromising factors such as the small veins of diabetes or vasoconstriction from nicotine. The tissue perfusion pressure decreases as the length of the flap increases from its base. When this pressure falls below a critical closing pressure of the arterioles, flap necrosis occurs beyond that point. On the face, the original studies based the actual length on angiosomal units of vascularity ( Figure 95-3 ).



Augmenting the viable length of a flap may be critical to success. The delay technique for a local flap involves circumferential incision alone, subcutaneous undermining alone through small incisions, or circumferential and subcutaneous undermining without mobilization. Two weeks after the delay procedure, the flap may be transferred to the recipient site. This delay results in enhanced circulation to the flap through the closure of arteriovenous shunts and the realignment of the vasculature within the subdermal plexus.
Angiosomal Unit
The angiosomal unit is the three-dimensional territory supplied by source arteries and veins. Identification of the anatomic territory of an individual perforator can help the surgeon define an area that may be safely lifted for a reconstructive effort with or without flap delay. The cutaneous perforator vessels at the flap base where the anastomotic connections usually occur can exhibit a reduced caliber, in which case they are named “choke arteries.” These narrowed anastomoses can produce vascular insufficiency and ultimate necrosis at the flap edge.
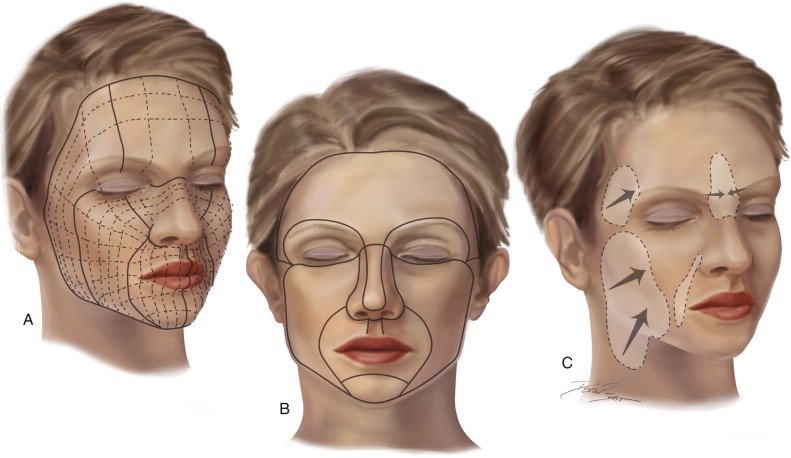
Facial Architecture
There is a wide variance of structural differences of the face depending on the location. These differences are often described and categorized as the facial units , examples of which are the eyelids, cheeks, nose, lips, mentum, and auricles. Some of these units can be further divided into subunits based on visible creases and differences in skin quality.
When designing an ideal flap for reconstruction, the most favorable result will be one that respects the facial subunits and their boundaries. Scars that lie directly along the borders of these units will be naturally camouflaged. Therefore, the surgeon who encounters a defect encompassing over half of a subunit such as the nasal tip or lip philtrum may consider removal of the entire subunit prior to reconstruction. The surgeon may consider independent repair of adjacent unit(s) so that large reconstructions do not flow nonanatomically from one unit to another ( Figure 95-4 ).
Technique: Basic Concepts in Local Flap Design
The simplest flaps are elliptical advancement flaps, which are usually designed in a 3 : 1 or 4 : 1 length-to-width proportion. Elasticity of the dermis determines how easily the ellipse can be closed.
The three quandaries to flap control are as follows:
- 1.
What to do with the triangular end of advancement excisions (Burrow’s triangles)
- 2.
What to do with the excess tissue or bunching ( dog ears, which form as tissue moves into a defect) ( Box 95-2 )
Box 95-2Management of Dog Ears- 1.
Do nothing (works well on the scalp where bunched tissue lies down over time).
- 2.
Close opposite lines of uneven lengths by spreading out the problem (halving).
- 3.
Remove the excess to a hidden area (an end or middle triangle).
- 4.
Lengthen the incision (to eliminate bunching).
- 5.
Perform an M-plasty (which shortens the problem).
- 6.
Reverse the S loop (effectively hiding the excess elsewhere).
- 7.
Advance the dog ear as a flap (subcutaneous “island”).
Modified from Zide M, Trokel Y: Head and neck skin cancer. In Miloro M, Ghali GE, Larsen PE, Waite PD: Peterson’s principles of oral and maxillofacial surgery, ed 3, vol 1, Shelton, 2012, People’s Medical Publishers. - 1.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


