Armamentarium
|
History of the Procedure
The carbon dioxide (CO 2 ) laser was invented by Kumar Patel in 1964. This was the first gas laser to produce high-power radiation continuously. The CO 2 laser has more practical applications today than any other type of laser. The chromophore (light-absorbing compound) of the CO 2 laser is water. Because more than 80% of the epidermis is composed of water, the CO 2 laser is particularly useful in the treatment of the skin. This ablative laser allows surgeons to perform CO 2 laser skin resurfacing (LSR) accurately, safely, and effectively with precise depth control.
The first CO 2 lasers were continuous wave (CW) lasers. These CW lasers increased in popularity in the 1980s but had little thermal control. Treatments of the skin took a very long time because the spot sizes were small and optical scanners did not exist. In addition, these treatments were very technique-sensitive. Thermal relaxation times were often violated, resulting in prolonged healing times and scarring. These clinical results were unacceptable, and short-pulse CO 2 laser energy was developed. These superpulsed CO 2 lasers were introduced in the 1990s. This dramatically reduced the incidence of scarring and the prolonged healing times seen with CW modalities. The superpulsed lasers were a major advantage over the CW lasers because they decreased the size of the thermal zone, with shorter pulse widths resulting in greater safety, less discomfort, and less downtime.
The first high-energy CO 2 pulsed laser, operating at a wavelength of 10,600 nm, was developed by Lumenis (Yokneam, Israel) and named the UltraPulse Laser. The advent of the Lumenis Ultrapulse Encore carbon dioxide laser (LUPCO 2 ) in the late 1990s changed everything for LSR. This laser provided the most safety with the shortest pulse width and narrowest thermal zone, resulting in less discomfort and less downtime. Erbium:YAG (yttrium-aluminum-garnet) lasers gained popularity in the 1990s and are still used today. The erbium:YAG laser emits a wavelength of 2940 nm, which is absorbed by water 10 times more efficiently than with the CO 2 laser. Unfortunately, it does not remove wrinkles the way a CO 2 laser can, so clinical results are compromised. Heat generation is insufficient to promote clinically significant collagen shrinkage. The thermal energy zone is smaller and water absorption is greater, so the collagen in the skin is undertreated compared to a CO 2 laser. The YSGG erbium laser (Cutera; Brisbane, California), with a 2790 nm wavelength, fills the gap between CO 2 and erbium:YAG lasers in terms of clinical use and effectiveness.
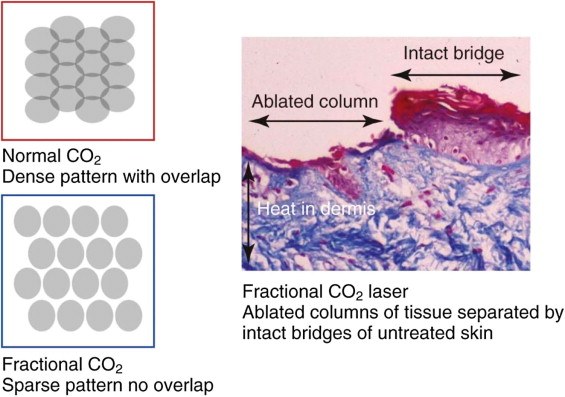
In 2004, Manstein et al. introduced the concept of fractional photothermolysis. This concept was a major advance in laser skin rejuvenation. Instead of treating 100% of the skin surface. as does traditional CO 2 LSR, this method treats a fraction of the skin on each pass. The computer coordinates drilling of multiple, small, vertically oriented holes, shaped like cylinders, of thermally damaged tissue called “microthermal zones.” The surrounding areas of unaffected tissue act as reservoirs for healing by providing structural and nutritional support and a reservoir for keratinocyte migration ( Figure 139-1 ). The thermomechanical destruction that occurs when the microthermal zones are made is followed by a predictable and beneficial skin-tightening phase through a process of heat-induced shrinkage of collagen and the initiation of neocollagenesis. Clinically, this concept of focal damage with adjacent tissue sparing has led to improved patient comfort and recovery in the postprocedural period.
Although the erbium laser wavelengths are very effective for resurfacing, the CO 2 laser has been found to be more effective for neocollagenesis because of its thermal damage, leading to dermal heating. All skin resurfacing lasers continue to be compared to the CO 2 laser. both in terms of downtime and results. The CO 2 laser has the longest track record and is considered by many to be the gold standard for laser skin rejuvenation.
History of the Procedure
The carbon dioxide (CO 2 ) laser was invented by Kumar Patel in 1964. This was the first gas laser to produce high-power radiation continuously. The CO 2 laser has more practical applications today than any other type of laser. The chromophore (light-absorbing compound) of the CO 2 laser is water. Because more than 80% of the epidermis is composed of water, the CO 2 laser is particularly useful in the treatment of the skin. This ablative laser allows surgeons to perform CO 2 laser skin resurfacing (LSR) accurately, safely, and effectively with precise depth control.
The first CO 2 lasers were continuous wave (CW) lasers. These CW lasers increased in popularity in the 1980s but had little thermal control. Treatments of the skin took a very long time because the spot sizes were small and optical scanners did not exist. In addition, these treatments were very technique-sensitive. Thermal relaxation times were often violated, resulting in prolonged healing times and scarring. These clinical results were unacceptable, and short-pulse CO 2 laser energy was developed. These superpulsed CO 2 lasers were introduced in the 1990s. This dramatically reduced the incidence of scarring and the prolonged healing times seen with CW modalities. The superpulsed lasers were a major advantage over the CW lasers because they decreased the size of the thermal zone, with shorter pulse widths resulting in greater safety, less discomfort, and less downtime.
The first high-energy CO 2 pulsed laser, operating at a wavelength of 10,600 nm, was developed by Lumenis (Yokneam, Israel) and named the UltraPulse Laser. The advent of the Lumenis Ultrapulse Encore carbon dioxide laser (LUPCO 2 ) in the late 1990s changed everything for LSR. This laser provided the most safety with the shortest pulse width and narrowest thermal zone, resulting in less discomfort and less downtime. Erbium:YAG (yttrium-aluminum-garnet) lasers gained popularity in the 1990s and are still used today. The erbium:YAG laser emits a wavelength of 2940 nm, which is absorbed by water 10 times more efficiently than with the CO 2 laser. Unfortunately, it does not remove wrinkles the way a CO 2 laser can, so clinical results are compromised. Heat generation is insufficient to promote clinically significant collagen shrinkage. The thermal energy zone is smaller and water absorption is greater, so the collagen in the skin is undertreated compared to a CO 2 laser. The YSGG erbium laser (Cutera; Brisbane, California), with a 2790 nm wavelength, fills the gap between CO 2 and erbium:YAG lasers in terms of clinical use and effectiveness.
In 2004, Manstein et al. introduced the concept of fractional photothermolysis. This concept was a major advance in laser skin rejuvenation. Instead of treating 100% of the skin surface. as does traditional CO 2 LSR, this method treats a fraction of the skin on each pass. The computer coordinates drilling of multiple, small, vertically oriented holes, shaped like cylinders, of thermally damaged tissue called “microthermal zones.” The surrounding areas of unaffected tissue act as reservoirs for healing by providing structural and nutritional support and a reservoir for keratinocyte migration ( Figure 139-1 ). The thermomechanical destruction that occurs when the microthermal zones are made is followed by a predictable and beneficial skin-tightening phase through a process of heat-induced shrinkage of collagen and the initiation of neocollagenesis. Clinically, this concept of focal damage with adjacent tissue sparing has led to improved patient comfort and recovery in the postprocedural period.
Although the erbium laser wavelengths are very effective for resurfacing, the CO 2 laser has been found to be more effective for neocollagenesis because of its thermal damage, leading to dermal heating. All skin resurfacing lasers continue to be compared to the CO 2 laser. both in terms of downtime and results. The CO 2 laser has the longest track record and is considered by many to be the gold standard for laser skin rejuvenation.
Indications for the Use of the Procedure
Laser skin rejuvenation provides a very effective way to safely treat problematic areas of facial aging. Not many skin treatments can consistently give such dramatic results as laser skin treatment. The final results of many facial cosmetic surgical treatments, including facelifts and blepharoplasties, are greatly enhanced by the addition of LSR ( Figure 139-2 ). The addition of a laser to these procedures is considered “the icing on the cake,” so to speak. It is no longer acceptable to rejuvenate the underlying structures and leave the damaged skin untreated. The laser treatment can be done in conjunction with these surgical procedures or performed as an “a la carte” protocol. This depends on the surgeon’s experience level and on variables such as the patient’s level of compliance, healing capacity, medical history, and accepted recovery time. In fact, it is widely known that it is difficult to achieve the best facial cosmetic surgical results without the addition of some form of facial laser treatment. Age certainly comes into play, but this is true for most facial cosmetic surgery. Many experienced surgeons do not consider a facelift complete without the addition of LSR.

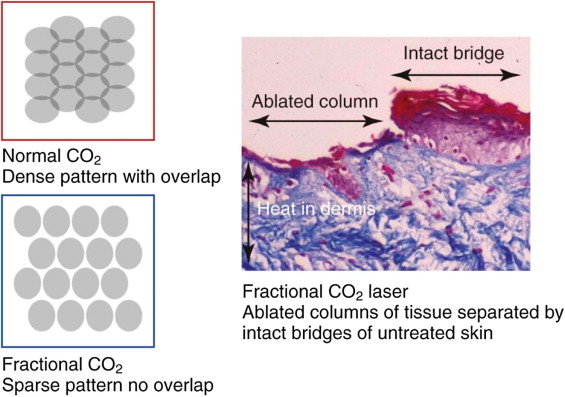
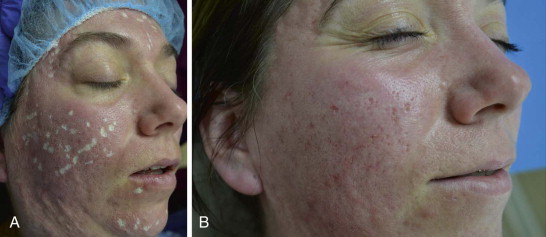
The problem areas of facial skin aging include varying degrees of skin laxity (dermatochalasis), wrinkles, skin quality, pore size, texture, and sun damage (dyschromia). Laser treatment can address all of these issues simultaneously, resulting in significant improvements. Ablative lasers do a very good job of targeting specific areas of the face that need it the most, such as fine lines and wrinkles around the eyes and mouth. “Smoker’s lines” around the lips can be identified and focused on appropriately. Dermatochalasis of the upper and lower eyelids can be treated with significant tightening and disappearance of wrinkles ( Figure 139-3 ). Pigment dyschromias confined to the epidermis are adequately treated with ablative lasers ( Figure 139-4 ). Vascular dyschromias are better treated with nonablative diode lasers or intense pulsed light (IPL) treatments in the 515 to 560 nm wavelength spectrum with specific targets for hemoglobin.
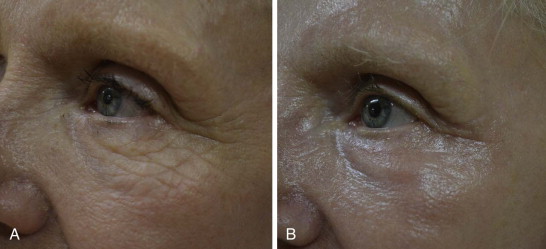

Many practitioners agree that the laser must get down to the papillary dermis to really tighten the skin and treat the signs of facial aging. Patients need to be sedated for work in the papillary dermis. The latest-generation LUPCO 2 is a high-energy, short-pulsed, scanned CO 2 laser with the added benefit of CoolScan technology ( Figure 139-5 ). This allows for safe and very effective treatment of a full face within 30 to 45 minutes. There are essentially no disposables. The laser has multiple treatment settings, ranging from fractional CO 2 (CO 2 Lite, ActiveFx, DeepFx) to full ablative CO 2 (MaxFx). This system is customizable by the surgeon for each patient, depending on the cosmetic facial subunits to be treated. The patient’s age and degree of facial aging, the amount of acceptable patient downtime, acne scarring, and other factors all can be taken into account with the CO 2 laser settings. In general, fractional settings result in decreased healing time compared to totally ablative settings. In the author’s experience, Active Fx alone requires approximately 5 days of patient recovery time. Adding Deep Fx to this treatment regimen requires approximately 7 to 10 days of patient recovery time. MaxFx also requires approximately 7 to 10 days of recovery time.
Shallow, dish-shaped acne scars can be improved with LSR, although the results are not as impressive as for wrinkle removal. Usually a combined treatment is necessary. Deep ice pick scars require dermal punch grafts, trichloroacetic acid chemical reconstruction of skin scars (TCA CROSS), subcision, other filling agents, or a combination of these ( Figure 139-6 ).
Dermatologic problems in the epidermis, papillary dermis, or midreticular dermis are also improved or removed with LSR. These problems include epidermal nevi, actinic keratoses, seborrheic keratosis, lentigines, syringomas, xanthelasmas, and superficial basal cell carcinomas. Traumatic or surgical scars can be improved with laser skin resurfacing as well. The resurfacing is performed 6 to 8 weeks after injury, while collagen remodeling is still occurring. Irregularities in scar height respond best. Actinic cheilitis also responds well to laser treatment. Rhinophyma can be reshaped with the laser with minimal bleeding, better accuracy, and a quicker healing time.
Limitations and Contraindications
Ablative skin resurfacing has its limitations, and the most important of these is patient selection by skin type. Human skin’s reaction to direct sunlight has been clinically quantified by Fitzpatrick. The Fitzpatrick classification ( Table 139-1 ) gives us a barometer to follow when selecting patients for this procedure. In general, the best candidates are Fitzpatrick skin types I, II, or III. These patients can be treated very effectively, with less risk of postinflammatory hyperpigmentation, the most common treatable complication of LSR. Special care is advisable when treating patients who have skin that is darker than Fitzpatrick type III. Patients with darker skin phenotypes are at risk for permanent hypopigmentation with procedures that reach the depth of the reticular dermis. Asian skin falls into the category of Fitzpatrick skin type IV. These patients can also be treated with minimal risk, as long as milder laser settings are used. Fitzpatrick skin types V and VI generally are not candidates for LSR due to the risk for permanent pigmentation changes.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


