History of the Procedure
Performance of the first total laryngectomy is attributed to Billroth, who in 1873 removed the entire larynx and left a pharyngocutaneous fistula. The patient lived for 7 months and died of metastatic disease. Multiple other reports from throughout Europe followed, but the operation was fraught with hazards and complications. Total laryngectomy did not achieve a level of acceptable safety until the early twentieth century. A variety of partial laryngectomy procedures evolved in the midtwentieth century and continue to be used effectively in carefully selected patients with smaller tumors. Total laryngectomy now is performed much less frequently due to advances in combined chemotherapy and radiation therapy (chemoradiotherapy [CRT]), which followed publication of the landmark Veterans Affairs Laryngeal Cancer Trial in 1991 and multiple other studies on organ preservation of the larynx that followed. Between 1997 and 2008, the number of laryngectomies performed in the United States decreased by 48%.
History of the Procedure
Performance of the first total laryngectomy is attributed to Billroth, who in 1873 removed the entire larynx and left a pharyngocutaneous fistula. The patient lived for 7 months and died of metastatic disease. Multiple other reports from throughout Europe followed, but the operation was fraught with hazards and complications. Total laryngectomy did not achieve a level of acceptable safety until the early twentieth century. A variety of partial laryngectomy procedures evolved in the midtwentieth century and continue to be used effectively in carefully selected patients with smaller tumors. Total laryngectomy now is performed much less frequently due to advances in combined chemotherapy and radiation therapy (chemoradiotherapy [CRT]), which followed publication of the landmark Veterans Affairs Laryngeal Cancer Trial in 1991 and multiple other studies on organ preservation of the larynx that followed. Between 1997 and 2008, the number of laryngectomies performed in the United States decreased by 48%.
Indications for the Use of the Procedure
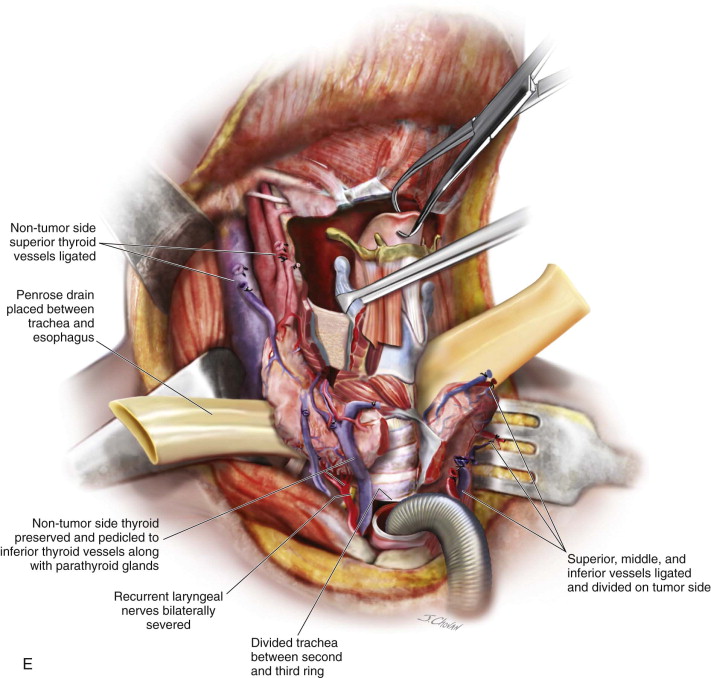
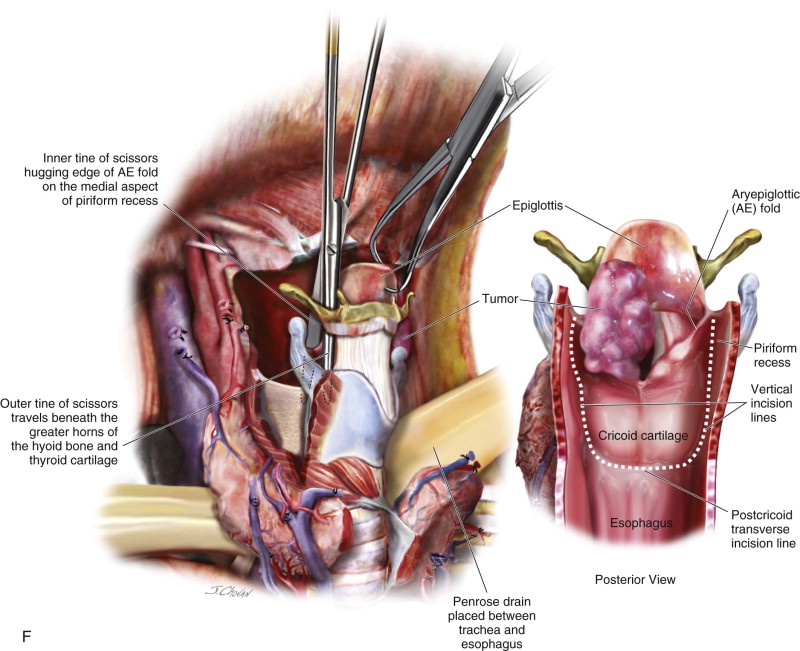
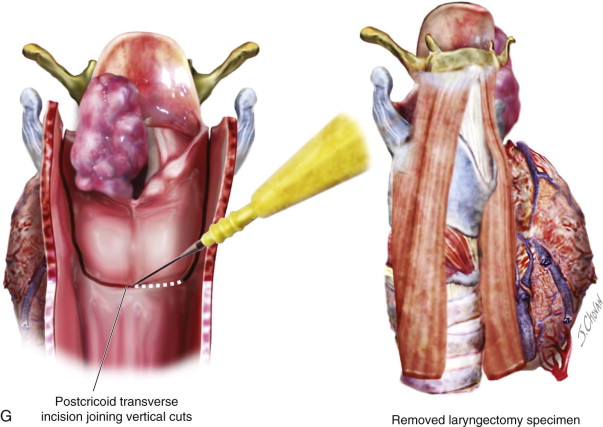
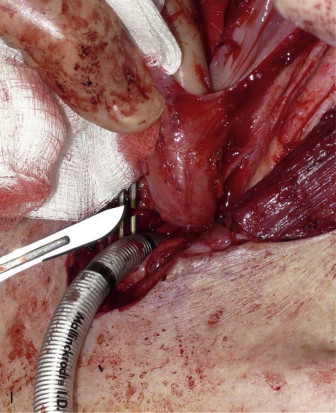
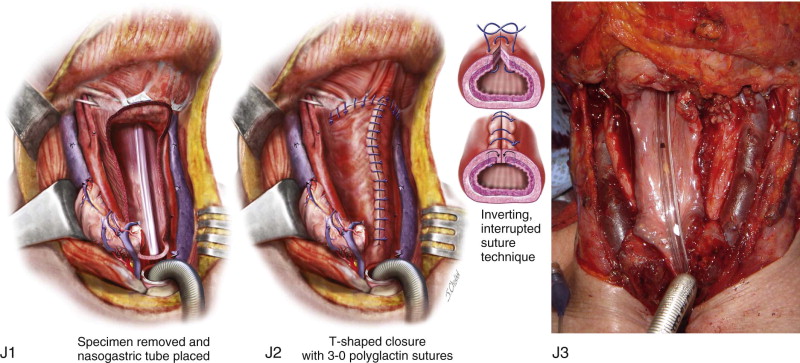
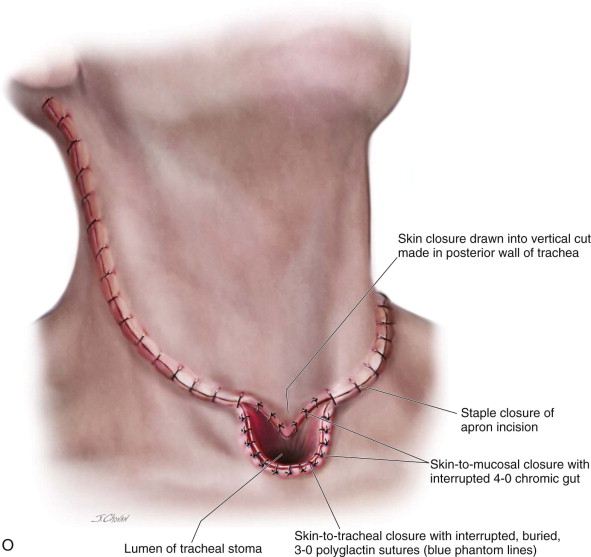
Total laryngectomy entails the complete removal of the larynx with separation of the esophagus from the trachea and establishment of a permanent tracheal stoma. A patient who has undergone total laryngectomy is known as a laryngectomee . Total laryngectomy may also include resection of portions of adjacent structures, such as the base of the tongue, lateral pharyngeal walls, cervical esophagus, and/or the proximal trachea, depending on the pattern of local tumor extension.
Early Laryngeal Cancer
Contemporary management of most early laryngeal cancer (T1 and T2) involves either radiotherapy alone or radiotherapy with various microlaryngoscopic or open partial laryngectomy techniques. Among selected patients, partial laryngectomy offers the advantage of preservation of some form of lung-powered speech, as opposed to esophageal speech or speech using an electronic device, which is required after total laryngectomy. Such procedures include vertical hemilaryngectomy, three-quarter laryngectomy, near-total laryngectomy, and so on (these procedures are outside the scope of this chapter). Supraglottic cancers arising above the glottis (e.g., in the epiglottis, vallecula, and so on) can be managed by supraglottic laryngectomy, which preserves the vocal cords and their function but can predispose the patient to chronic aspiration. In some patients, supraglottic laryngectomy can be performed transorally with a surgical robot.
Total laryngectomy is the oncologic salvage procedure should organ preservation therapy fail to control the cancer. Partial laryngectomy in the surgical salvage setting should be considered only for carefully selected patients. Total laryngectomy may also be indicated for tumor-free patients who have undergone prior partial laryngectomy and/or radiotherapy and who have developed intractable aspiration with recurrent pneumonia or other irreversible laryngeal dysfunction after cancer therapy. Use of a surgical robot to perform total laryngectomy has also been reported.
Advanced Laryngeal Cancer
Advanced laryngeal cancer is usually treated with CRT in an effort to preserve the larynx. A review of the evolution of this larynx-sparing philosophy is found in an editorial by Strojan ; however, survival after larynx-preserving CRT is only equivalent to, and not better than, that for total laryngectomy followed by radiotherapy. Total laryngectomy is often reserved for salvage of patients with advanced-stage disease (T3 and T4) whose cancer recurs after radiotherapy alone or after CRT. Laryngectomy for salvage after failure of CRT is the only therapeutic option with curative intent for such patients, but it has been associated with an overall complication rate of 56% in this setting. Total laryngectomy is often chosen as the primary treatment for patients with advanced, high-volume cancer of the larynx in which extensive cartilage destruction by the cancer would prohibit the return of meaningful laryngeal function, although this indication has been challenged. Total laryngectomy may be the preferred treatment option among cancer patients with significant pulmonary comorbidity who would be at risk for aspiration pneumonia after radiation or after partial laryngectomy. Radionecrosis of the larynx after CRT is an uncommon complication that may be difficult to differentiate from cancer recurrence, but it usually is an indication for total laryngectomy.
Limitations and Contraindications
Total laryngectomy may include partial resection of the adjacent lateral pharyngeal wall, maintaining partial continuity of the oropharyngeal mucosa superiorly with the esophagus inferiorly. Bulky tumors that extend outside the larynx to extensively involve the pharyngeal walls may require circumferential resection of the entire posterior and lateral pharyngeal walls, which produces a complete discontinuity between the mucosal surfaces of the oropharynx and the esophagus. This is termed a laryngopharyngectomy, and reconstruction requires the importation of either a tubed pedicled or microvascular flap, interposition of a microvascular jejunum, or completion esophagectomy and gastric pull-up. Subglottic and tracheal extension of carcinoma arising in the glottis may require significant tracheal resection; however, the trachea can almost always be mobilized cephalad out of the chest and pexed to the sternal periosteum, allowing construction of an adequate stoma.
Before surgery, the patient must be fully prepared for the permanent loss of lung-powered speech, and preoperative consultation with a speech-language pathologist is highly advisable. Plans must be made for the patient to be able to communicate with the medical and nursing staff after surgery, using writing equipment, word boards, or other devices. The medical and nursing staff should be aware that the patient’s only airway is the tracheal stoma; if a crisis develops, attempts at Ambu bag ventilation through the nose and mouth and attempts at oral intubation are inappropriate and ineffective. Other than life-threatening medical comorbidities, contraindications to total laryngectomy include any situation in which a neoplastic or other severe condition of the larynx could be controlled by lesser means.
Technique: Total Laryngectomy
The patient is positioned on the operating table with the head extended, using either a Mayfield horseshoe headholder or a shoulder roll. The arms are tucked, and the elbows are padded, as for any major head and neck operation. Central venous access and placement of an arterial line frequently are performed before laryngectomy, The patient is intubated orally unless a preliminary tracheostomy has been performed. Moderate hypotensive anesthesia, if appropriate for the specific patient, is helpful in minimizing blood loss.
Step 1:
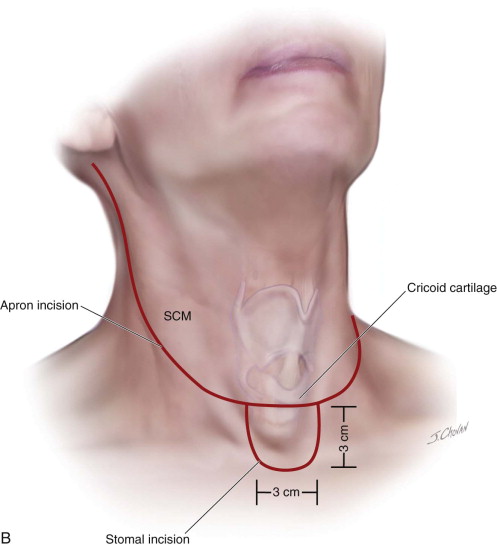
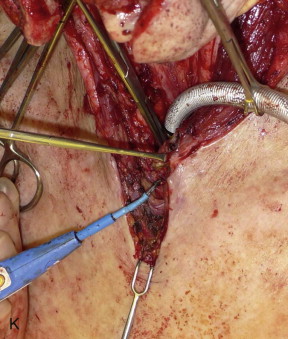
Cervical Incision
An apron incision is made with a horizontal limb that lies just below the level of the cricoid cartilage. Extending inferiorly in the midline from this incision and centered over the suprasternal notch is a U -shaped skin excision measuring 3 cm in both the vertical and horizontal dimensions. This skin excision will correspond to the position of the tracheal stoma. If a previous tracheostomy has been performed, its surrounding skin is included in this tissue.
The apron flap incision is extended through the platysma with a scalpel or electrocautery, and a subplatysmal apron flap is raised to a level above the hyoid. An effort is made not to undermine the inferior skin flaps in the area of the stoma. A tracheostomy can be performed at this point and the oral endotracheal tube can be removed, or the tracheal entry can be performed at the conclusion of step 4 ( Figure 105-1, A and B ).


Step 2:
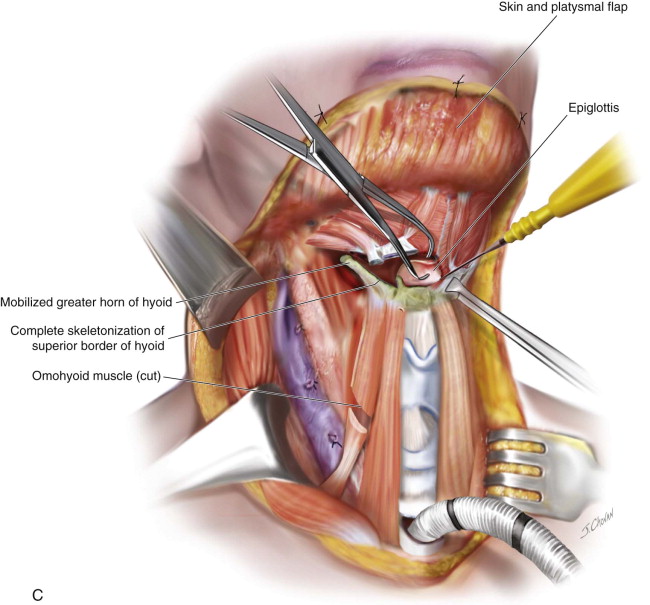
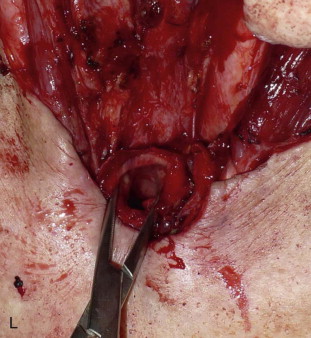
Exposing the Hyoid
After appropriate neck dissections, the neck dissection specimens can be either pedicled to the lateral aspect of the thyroid cartilage or can be divided, oriented, and sent separately to pathology. In this chapter, we will consider the neck dissections to have been removed from the larynx specimen. Electrocautery is used to separate the tongue musculature and digastrics from the superior aspect of the hyoid bone. Each greater horn of the hyoid is exposed circumferentially ( Figure 105-1, C ).
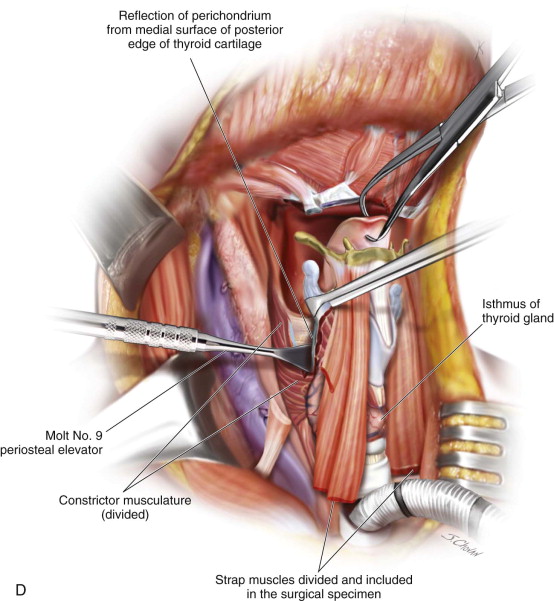
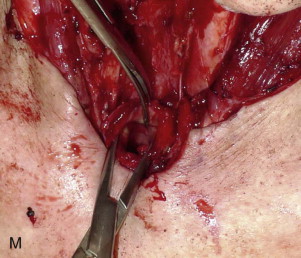
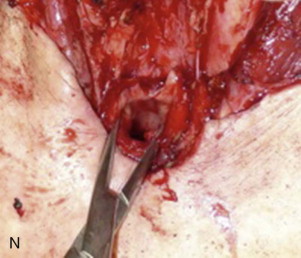
Step 3:
Skeletonizing the Lateral Aspect of the Thyroid Cartilage
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


