This article reports the comprehensive, interdisciplinary treatment of a 50-year-old periodontally compromised adult patient with multiple missing posterior teeth. After initial periodontal treatment, the maxillary first molars and right central incisor were intruded orthodontically. Miniscrews were used to intrude the maxillary first molars by 3 mm. The mandibular arch was restored with a tooth-supported overdenture. Root coverage of the maxillary right central incisor was performed using Alloderm (Biohorizons, Birmingham, Ala). At the end of the interdisciplinary therapy, the results were esthetically pleasing, with the patient’s oral functions restored to the optimum. The emphasis of this report is to highlight the importance of integrating various specialties such as periodontics, orthodontics, endodontics, and restorative dentistry toward a common goal of improving the patient’s oral health, function, and esthetics.
Recently, more adults have been actively seeking orthodontic treatment. In these patients, loss of teeth and periodontal breakdown cause pathologic migration of teeth, making the orthodontic treatment more complicated. Such patients should be treated with an interdisciplinary approach aimed not only to improve oral function and esthetics but also to prevent such problems later in life. Therefore, before initiating orthodontic treatment, the clinician should identify the various problems, establish specific treatment objectives, formulate a definitive treatment plan, and determine the exact treatment sequence involving the various specialties of dentistry.
The orthodontist has a special place on the team of specialists involved in the comprehensive treatment planning for periodontally compromised adult patients with missing teeth. Adjunctive orthodontic treatment can result in improved gingival and bone levels, traumatic occlusion, hemiseptal and infrabony defects, excessive spacing, tipped abutment teeth, inadequate pontic or implant space, and supraeruption of teeth.
Extrusion of the maxillary posterior teeth commonly results from a longstanding loss of mandibular antagonistic teeth. The elongated dentoalveolar segment can induce functional disturbances and interfere during prosthetic occlusal rehabilitation. Conventional options for removing such interferences include occlusal reduction with possible root canal treatment and posterior subapical osteotomy. Orthodontic intrusion of molars was considered a difficult movement to achieve with conventional orthodontic techniques. Fortunately, the invention of various skeletal anchorage systems such as conventional prosthetic implants, miniplates, and miniscrews has made it possible to carry out such movements.
In this article, we report the comprehensive treatment with an interdisciplinary approach of a periodontally compromised adult with multiple posterior missing teeth. The emphasis was to highlight the importance of integrating various specialties including periodontics, orthodontics, endodontics, and restorative dentistry toward a common goal of improving the patient’s oral health, function, and esthetics.
Diagnosis and etiology
A 50-year-old woman was referred by a general dentist to the graduate orthodontic clinic of Manipal College of Dental Sciences, Manipal, Karnataka, India, for assessment and possible correction of a pathologically migrated maxillary right central incisor and intrusion of the maxillary posterior teeth to facilitate prosthetic rehabilitation of her mandibular dentition. She had a history of multiple extractions and restorative work in the mandibular arch about 10 years previously. Her medical history did not contribute to underlying systemic conditions. The temporomandibular joint examination was normal, with an adequate range of jaw movements.
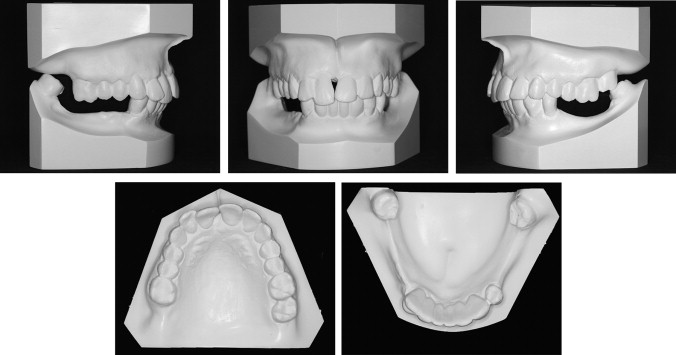
The pretreatment facial examination showed a brachycephalic facial pattern with a convex soft-tissue profile ( Fig 1 ). The ratio of lower anterior facial height to upper anterior facial height was normal, and the ratio of lower facial height to throat depth was normal. The nasolabial angle and the mentolabial sulcus were normal. The patient had competent lips; upon smiling, 50% of the occlusogingival length of the maxillary incisors was visible. The maxillary and mandibular dental midlines were coincident with the facial midline.

The intraoral examination showed that the maxillary right central incisor was extruded beyond the occlusal plane by 3 mm and was grade II mobile. There was a midline diastema of 2 mm in the maxillary anterior region. The maxillary first molars were extruded into the mandibular edentulous space by 3 mm bilaterally ( Fig 2 ), and the right second molar was missing. In the mandibular arch, on the left side, the second premolar and the first molar were missing; on right side, both premolars and the first molar were missing. Both mandibular central incisors were missing and were restored with a 6-unit fixed partial prosthesis with the mandibular lateral incisor and canines as abutments. The fixed partial denture and all abutment teeth were grade II mobile. On the right side, there was no occlusion of the posterior teeth; on the left side, only the maxillary second molar occluded with the mandibular second molar. The canines were in a Class I relationship bilaterally, but the molar relationship could not be established.
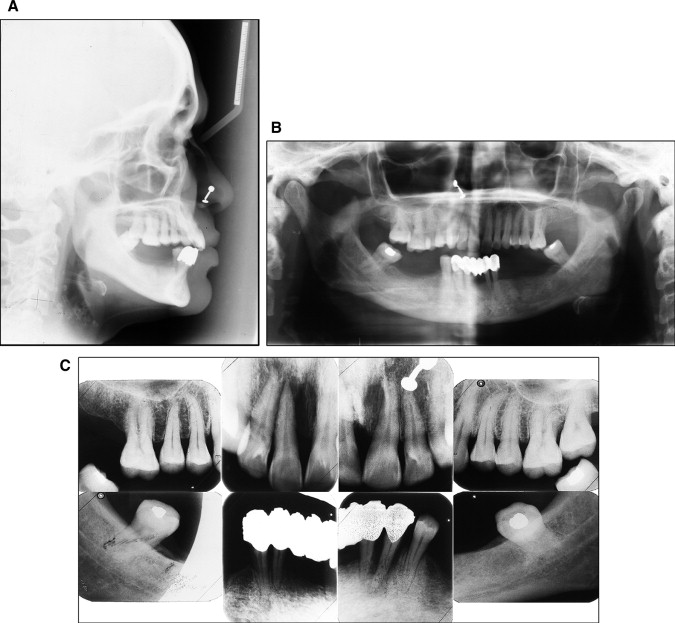
Cephalometric analysis indicated a skeletal Class I relationship with an average vertical growth pattern ( Fig 3 , Table ). The panoramic radiograph ( Fig 3 ) showed long edentulous spaces and overall decreased alveolar bone support. The mandibular second molars were tipped mesially into the extraction spaces of the first molars. The intraoral periapical radiograph showed extensive vertical bone loss on the mesial aspect of the maxillary right central incisor ( Fig 3 ). Although periapical radiolucency was apparent on the radiograph with respect to the maxillary right lateral incisor, clinically it was healthy and had a positive response to electric pulp vitality testing.
| Norm | Pretreatment | Posttreatment | |
|---|---|---|---|
| SNA (°) | 82 ± 2 | 80 | 80 |
| SNB (°) | 80 ± 2 | 79 | – |
| ANB (°) | 2 | 1 | – |
| Facial angle (°) | 88 ± 3 | 89 | 90 |
| OP-FH (°) | 8.7 | 6 | 5 |
| Interincisal (°) | 130 ± 5 | 124 | – |
| Maxillary incisor-APg (mm) | 6 | 9 | 10 |
| FMA (°) | 25 | 25 | 24 |
| IMPA (°) | 90 | 95 | – |
| FMIA (°) | 65 | 60 | – |
| Maxillary incisor-NA (°) (mm) | 22/4 | 28/9 | 32/10 |
| Mandibular incisor-NB (°) (mm) | 25/4 | 29/6 | – |
| GoGn- SN (°) | 32 | 31 | 30 |
| U6-PP (mm) | 24 | 25 | 23 |
| U1-PP (mm) | 30 | 30 | 28 |
| Upper facial height (mm) | 58 | 54 | 54 |
| Lower facial height (mm) | 75 | 68 | 66 |
| UFH/TFH (%) | 45 | 44.2 | 45 |
| LFH/TFH (%) | 55 | 55.8 | 55 |
After thorough clinical and radiographic examinations, the patient was diagnosed with a skeletal and dental Class I malocclusion with chronic generalized moderate periodontitis, maxillary right central incisor extrusion, supraeruption of the maxillary first molars, and partially edentulous maxillary and mandibular arches.
Treatment objectives
Because the patient’s problems required a multidisciplinary approach, the overall treatment objectives were control of periodontal disease, relief of the trauma to the occlusion of the maxillary right central incisor, establishment of posterior occlusion, and long-term personal and professional periodontal maintenance. The specific orthodontic objectives were to intrude the maxillary right central incisor and the maxillary first molars to obtain a flat occlusal plane so that enough interocclusal space was created for replacement of the missing posterior teeth in the mandibular arch.
Treatment objectives
Because the patient’s problems required a multidisciplinary approach, the overall treatment objectives were control of periodontal disease, relief of the trauma to the occlusion of the maxillary right central incisor, establishment of posterior occlusion, and long-term personal and professional periodontal maintenance. The specific orthodontic objectives were to intrude the maxillary right central incisor and the maxillary first molars to obtain a flat occlusal plane so that enough interocclusal space was created for replacement of the missing posterior teeth in the mandibular arch.
Treatment alternatives
Based on the treatment objectives, the following treatment alternatives were presented to the patient.
- 1.
Extraction of all remaining teeth in the mandibular arch and restoration with an implant-supported mandibular denture, intentional root canal treatment of the supraerupted maxillary teeth to reduce their clinical crown heights, and their restoration with crowns. Although this option had the advantage of the shortest treatment time, the patient wanted to retain as many of her teeth as possible, so she declined it. Moreover, for financial reasons, she did not choose the implant-supported overdenture.
- 2.
Segmental osteotomy and intrusion of the maxillary posterior segment, and restoration of mandibular arch with a tooth-supported overdenture. The patient declined any major surgical procedure because of the associated risks and hospitalization expenses.
- 3.
The third treatment option, finally chosen by the patient, was to orthodontically intrude the supraerupted maxillary teeth with miniscrews and restore the mandibular arch with a tooth-supported overdenture.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


