Abstract
Pain, swelling, trismus, and alveolar osteitis often occur after removal of impacted third molar teeth. To minimize these complications a number of mucoperiosteal flap designs have been advocated, but, to date, a pedicle flap design has not been evaluated. In a randomized prospective split mouth study, 52 participants had bilateral symmetrically impacted mandibular third molars removed over two sessions. A buccal envelope or pedicle flap was randomly assigned to the left or right third molar site. Pre-and postoperative pain and swelling were recorded using a standardized visual analogue scale, trismus was measured as the maximum inter-incisal opening distance in millimetres and dry socket was assessed clinically. Greater continuous pain, pain on maximum opening, and oro-facial swelling were recorded with the pedicle flap design. Continuous pain resolved significantly faster with this flap design ( p < 0.05). Trismus was similar for both flap designs ( p > 0.05). Five cases of alveolar osteitis occurred with the envelope flap whilst no cases developed with the pedicle flap, but the incidence was too small for statistical analysis. The pedicle flap improved some aspects of postoperative pain experience and reduced the incidence of alveolar osteitis, but further investigation with a larger sample size is required to evaluate its significance.
Third molars are the most likely teeth to become impacted with around 33% of the population having at least one impaction . Impacted third molar teeth are associated with a variety of problems including pericoronitis often leading to oro-facial infection, developmental cysts or neoplasms, as well as caries, periodontitis, and root resorption of the adjacent tooth . Lower third molar teeth can cause orthodontic and prosthetic treatment problems . Many of these issues can be managed with extraction of the offending tooth . Prophylactic or curative removal of impacted third molar teeth is the most common surgical procedure carried out by oral surgeons . Third molar tooth removal is frequently associated with debilitating acute complications including pain, swelling, trismus , and alveolar osteitis (dry socket) . As a consequence, research has concentrated on finding techniques to minimize these complications, including the use of surgical drains , different closure techniques and various flap designs .
Primary closure of the mucoperiosteal flap over sound bone is desirable on the basis that this will enhance healing of the surgical wound. The traditional flap designs used for third-molar surgery do not accomplish primary closure over sound bone if the tooth has erupted into the oral cavity. This is thought to lead to a high incidence of mucosal dehiscence with these designs . A pedicle flap design is routinely used in other types of oral surgery to achieve primary closure of a wound or defect and it is possible that this design could provide advantages to third molar extraction site healing.
The aim of this study is to assess the effect of a pedicle flap design on the occurrence and severity of common acute postoperative sequelae associated with lower third molar tooth removal.
Materials and methods
A randomized prospective split mouth study was undertaken. Ethical approval was obtained from the Health and Disability Commissioner Lower South Island ethics committee and Ngai Tahu Research consultation committee.
The inclusion criteria for this study included: bilateral symmetrically impacted partially erupted mandibular third molar teeth; no associated pathology; no medical conditions or medications that might alter wound healing potential; patients had to be ASA I and II ; and aged between 16 and 40 years. Patients were excluded from the study if they had a history of abuse of midazolam, allergy to any medications used during or after the procedure for patient management, pregnancy, previous or present radiotherapy to the third molar tooth region of the lower jaw, if they were on long term corticosteroid or bisphosphonate medication, or had a bone disorder such as Paget’s disease or fibrous dysplasia that could interfere with bone healing. 57 participants met the inclusion criteria.
Written informed consent was obtained from each participant after both the procedure and the postoperative reviews were explained. The participants were advised of their right to withdraw from the study at any time without prejudice as per ethical approval requirements with the option to be placed on the pre-existing waiting list. During the initial consultation appointment each participant’s demographic information (age and gender), and baseline measurements were recorded, including the presence of pericoronitis, pain and swelling levels and maximum inter-incisal distance. The presence of periocoronitis was assessed clinically based on the existence of pericoronal erythema, pain and swelling. Preoperative pain was evaluated by asking the patient to mark on a 10 cm visual analogue scale the level of pain they were experiencing both at rest and on maximal mouth opening. Swelling was assessed subjectively by asking participants to look into a mirror and mark on a separate 10 cm visual analogue scale the level of facial swelling they felt was present. Maximum inter-incisal distance was assessed by measuring the distance between the mesio-incisal edges of the right maxillary and mandibular central incisor teeth during maximal mouth opening with a standard ruler in millimetres.
All surgical procedures were carried out under local anaesthesia using mepivicaine hydrochloride 2% with 1:100,000 adrenaline (Scandonest 2%, Septodontont, Saint-Maur-des-Fossés, France) supplemented with intravenous sedation (Hypnovel, Roche Products Ltd., Auckland, New Zealand) by a single surgeon (SMG).
Participants were randomly allocated into one of two groups using the logan envelope technique. In one group the first procedure was carried out using the envelope flap design, whilst with the other the pedicle design was used first. Both flap designs were then randomly allocated to either the left or right side of each participant’s lower jaw again using the logan envelope technique. A minimum of 3 weeks after the first procedure the contralateral lower wisdom tooth was removed using the unemployed flap design.
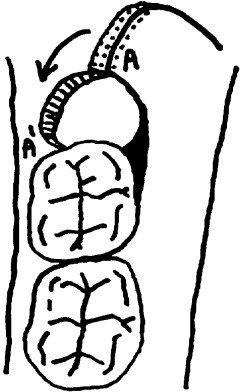
An envelope flap ( Fig. 1 ) was raised in the standard manner. An incision was placed in the buccal gingival sulcus from the mesio-buccal line angle of the first molar to the most distal visible aspect of the third molar. The releaving incision then extended up the external oblique ridge. The pedicle flap design ( Figs. 2 and 3 ) involved the same initial incision in the buccal gingival sulcus as the buccal envelope flap but distal to the third molar the incision was extended approximately 1 cm and then curved towards the buccal sulcus, allowing for rotation of the flap and primary closure over sound bone. Prior to closure the gingival papilla distal to the second molar was removed and the apex of the pedicle de-epithelialised. A lingual flap was raised in the subperiosteal plane irrespective of flap design and the lingual nerve protected using a Howarth retractor. A large round surgical bur (No 8) with copious irrigation was used to remove bone superior, distal and buccal to the crown of the third molar tooth. A fissure bur was used to section the tooth if required. The tooth was then elevated and delivered and the dental follicle removed. Sterile saline irrigation of the socket was carried out to remove any debris. Interrupted and horizontal mattress sutures (3-0 polyglactin 910; Undyed Vicryl Rapide; Ethicon, Somerville, NJ, USA) were placed to stabilize the flap and close the extraction site to the desired degree. Haemostasis was achieved prior to flap closure and was reassessed prior to discharge.


A prescription of ibuprofen 400 mg, two tablets four times daily (Ethics, Multichem NZ Ltd., North Shore City, Auckland, New Zealand) and paracetamol 500 mg, two tablets four times daily (Pharmacare, API Consumer brands, Manukau City, Auckland) was given to the participant’s escort. Codeine phosphate (15 mg) one to two tablets maximum four times daily (PSM Healthcare Ltd., t/a API Consumer Brands, Manukau City Auckland) was also included for participants to use if adequate pain relief was not provided by ibuprofen and paracetamol. In addition a 0.2%, chlorhexidine gluconate antiseptic mouth rinse with ethanol 11.8% (v/v), 15 mL three times daily (Rivacol, Orion Laboratories Pty Ltd., Balcatta, Western Australia, Australia) was prescribed. The participant’s escort was also given routine postoperative and post-sedation instructions.
Information recorded during the procedure included; the type of flap design used on each side, length of surgery time and any intra-operative problems.
Participants were requested to mark on one of a series of 10 cm visual pain scales the severity of pain they experienced at rest and on maximal mouth opening on each morning and evening for 4 days postoperatively. They were also asked to record the amount of each of the prescribed analgesics they used.
Each participant was clinically assessed on postoperative days 2 and 7 to evaluate the presence/absence of dry socket/infection, trismus (maximal inter-incisal distance), and oro-facial swelling. To determine the level of postoperative swelling participants were asked to mark on a 10 cm visual analogue scale the level of oro-facial swelling they felt was present when looking into a mirror. Maximum inter-incisal distance was assessed by the clinician by measuring the distance between the mesio-incisal edges of the right maxillary and mandibular central incisor teeth during maximal mouth opening with a standard ruler in millimetres. Any other complications were also recorded. The presence of alveolar osteitis was assessed clinically using criteria set out by Blum . The presence of infection was assessed clinically.
The data gained from this project required the use of mixed modelling for statistical analysis. This was carried out using STATA © (StataCorp LP, Texas, USA) a data analysis and statistical software version 11.
Results
Of the 57 participants, 52 had both lower third molar teeth removed and oro-facial swelling, trismus, dry socket, infection and dehiscence amongst other variables evaluated. Of these 52 participants, 10 did not complete the pain evaluation forms, so data from 52 participants was used for statistical analysis of all other variables except for pain levels, for which data from 42 participants was analysed.
The procedure duration was different between the two flap designs ( p < 0.05). The mean duration for third molar removal using the envelope flap design was 17.9 ± 5.3 min and 20.0 ± 4.8 min for the pedicle flap procedure.
Greater continuous pain and pain on maximum opening occurred overall with the pedicle flap design ( Table 1 ) ( p < 0.05). Reduction in continuous pain with this flap was steeper over the 4 days measured. Pain levels for both flap designs were higher in the morning than in the evening. Adjusting for analgesic intake did not alter the difference in pain severity between the two flap designs.
| Continuous pain | Envelope flap | Pedicle flap | Mixed model p > | z | |
|---|---|---|---|
| Preoperative | 0.210 | ||
| Mean | 0.000 | 0.095 | |
| Standard deviation | 0.000 | 0.484 | |
| Postoperative | 0.000 | ||
| Mean | 3.691 | 4.257 | |
| Standard deviation | 2.114 | 2.511 | |
| Pain on maximal mouth opening | |||
| Preoperative | 0.323 | ||
| Mean | 0 | 0.048 | |
| Standard deviation | 0 | 0.309 | |
| Postoperative | 0.003 | ||
| Mean | 3.952 | 4.601 | |
| Standard deviation | 2.239 | 2.366 | |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


