At present, there are no objective testing modalities available for evaluation of iatrogenic injury to the terminal branches of the trigeminal nerve, making such clinical diagnosis and management complicated for the oral and maxillofacial surgeon. Several imaging modalities can assist in the preoperative risk assessment of the trigeminal nerve as related to commonly performed procedures in the vicinity of the nerve, mostly third molar surgery. This article provides a review of all available imaging modalities and their clinical application relative to preoperative injury risk assessment of the inferior alveolar nerve and lingual nerve, and postinjury and postsurgical repair recovery status.
At present, there are no “purely” objective testing modalities available for evaluation of iatrogenic injury to the terminal branches of the trigeminal nerve, and this makes the clinical diagnosis and management of these conditions fairly complicated for the oral and maxillofacial surgeon. All available clinical neurosensory testing modalities require patient cooperation and are based on a patient response, thus introducing a subjective component to the “objective” process. Furthermore all testing is commonly performed at the post-injury stage, so no individual baseline testing results are available for comparison and true determination of the magnitude of the resultant damage. For objective testing, several imaging modalities are available and can assist in the preoperative risk assessment of the trigeminal nerve, as related the commonly performed procedures in the vicinity of the nerve, mostly third molar surgery. In addition, these studies may be applied for objective functional monitoring of either spontaneous or surgically assisted recovery of the inferior alveolar (IAN) and lingual (LN) branches of the third division of the trigeminal nerve. This article provides a review of all available imaging modalities and their clinical application relative to the preoperative nerve injury risk assessment, and postinjury and postsurgical repair recovery status of the IAN and LN.
General considerations
Because the LN and IAN are at risk for injury during a variety of common oral and maxillofacial surgical procedures, including third molar removal, interest in documenting the position of these specific nerves prior to surgery has been significant. Early attempts at documenting the position of the LN in the third molar region have included cadaveric dissections and clinical observations during third molar extraction surgery. These studies suffer from a variety of methodological problems, including the potential for iatrogenic displacement of the nerves during the surgical dissection (in both the cadaveric studies and the clinical trials) as well as from the cadaveric specimen fixation process. Despite these limitations, Kisselbach and Chamberlain reported the position of the LN in the third molar region in 34 cadaver specimens and 256 cases of third molar extraction. This study found that in 17.6% of cadaver specimens and in 4.6% of clinical cases, the LN was superior to the lingual crest, and in 62% of cases the LN was in direct contact with the lingual cortex. In another anatomic study, Pogrel and colleagues examined the LN position in the third molar region using reproducible landmarks in 20 cadavers (40 sides), and found the LN above the lingual crest in 15% of cases and a mean horizontal distance from the lingual crest of 3.45 mm. Both of these anatomic studies confirmed the relative vulnerable position of the LN during third molar surgery.
Objective, noninvasive, radiologic imaging modalities in the preoperative assessment of the patient at risk for nerve injury, as well as a method for monitoring following injury and postrepair phases of neurosensory recovery, are highly desirable. Radiologic assessment should be categorized with regard to the timing of the imaging period; that is, preinjury, postinjury, and postrepair phases. Preinjury assessment refers to the documentation of the in situ position of a nerve before any surgical intervention that may place that nerve at risk for iatrogenic injury (eg, third molar removal). Intraoperative monitoring of nerve function during a surgical procedure (eg, sagittal split mandibular osteotomy) that involves a specific nerve may also be used, most commonly with a functional assessment of nerve conduction and electrophysiological status, such as with somatosensory evoked potentials. Postinjury imaging may be divided into a primary phase (following nerve injury and allowing for spontaneous neurosensory recovery without microneurosurgical intervention) and a secondary phase (following surgical nerve exploration and microneurosurgical repair). Primary postinjury imaging may be clinically significant if it can correlate objective (radiologic) findings with subjective (clinical examination) findings, and thereby guide the need for microneurosurgical intervention and possibly aid in treatment planning (ie, the length of altered neural anatomy and the need for an interpositional nerve graft). In general, based on clinical neurosensory testing, an attempt is made to classify the injury according to one or more staging, or classification, schemes. The staging systems of Seddon and Sunderland are based on histologic assessment of nerve injury, and are intended to serve as prognostic indicators of the potential for spontaneous neurosensory recovery.
There have been several reports of intraoperative nerve monitoring specifically during LeFort osteotomy (V 2 division) and mandibular sagittal split osteotomy (V 3 division) procedures. These studies have used somatosensory evoked potentials to document the transient increased latency and decreased amplitude of signal activity that occurs during surgical manipulation of the nerve during the osteotomy procedures. Somatosensory evoked potentials can be used as a postinjury or postrepair test, to document the degree of neural injury and to monitor the progression of neurosensory recovery over time.
Preoperative radiologic risk assessment of the IAN and LN
Panoramic Radiography
The preoperative assessment of the position of the IAN during third molar consultation has been routinely performed with the use of a panoramic radiograph. Obviously the information gained from this study is extremely limited due to the 2-dimensional nature of the image, the variable magnification of the bony anatomy (for the IAN), and the complete inability to visualize the position of the lingual nerve. It should be kept in mind that this radiograph demonstrates the position of the inferior alveolar canal, and not the IAN, specifically. Valuable information can be obtained from the panoramic radiograph as a stand-alone imaging modality with regard to the relationship of the IAN in the vertical plane, but not in the horizontal dimension. The most useful aspect of the panoramic radiograph is in assessing increased potential for inferior alveolar nerve injury during third molar extraction based on the presence of several radiographic predictors ( Fig. 1 ).
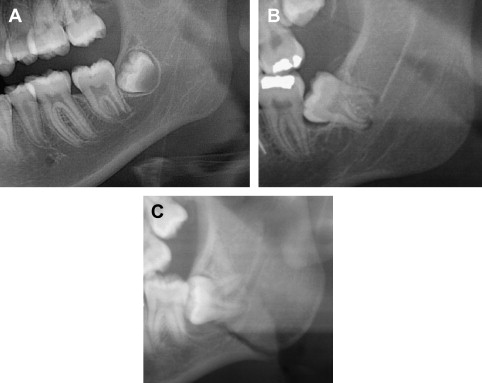
Other types of plain radiographs, such as periapical ( Fig. 2 ) or anteroposterior films and lateral cephalograms, are not routinely used for accurate preoperative routine risk assessment for IAN injury. Superimposition and wide variations in magnification of the structures based on their location do not allow for reliable and reproducible information to be obtained with plain films. Furthermore, even if the IAN could be visualized in the third molar region, only a rough outline of tooth and root anatomy would be obtained, making these images of limited if any value for nerve injury appraisal.

Computed Tomography
The use of computed tomography (CT) in the assessment of nerve injuries is very limited, although it has been used more recently for assessment of the inferior alveolar canal with regard to the position of the third molar. An evaluation of bone window attenuation images may indicate violation of the cortical outline of the inferior alveolar canal, either from implant placement or following facial trauma (eg, posterior mandible fracture) ( Fig. 3 ), but yields little information regarding the condition of the IAN itself or the neurovascular bundle. The use of soft tissue window CT images for the LN or IAN is compromised by very poor-detail resolution that precludes its routine application in neural assessment. Furthermore, dental artifacts often pose severe limitations in obtaining accurate information regarding the position of the LN to the lingual cortex of the mandible in critical areas, even in the soft tissue window views, and despite the current use of high-resolution image acquisition.
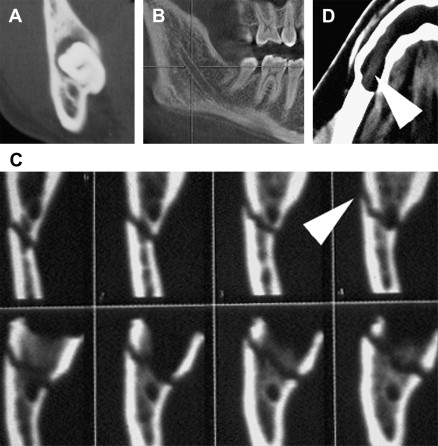
In 1998 CT cone beam (CBCT) technology, previously used only in angiographic imaging, was employed in the United States as a potential imaging modality for the maxillomandibular complex. The presurgical evaluation of impacted mandibular third molar relationship to the IAN has gained popularity over conventional CT scanning and plain panoramic radiographs among oral and maxillofacial surgeons. The need for accurate imaging with the lowest possible dose of radiation (ie, ALARA rule: As Low As Reasonably Achievable) seems to be satisfied acceptably with this technology. CBCT provides the desirable 3-dimensional representation of the anatomic location of interest, with minimal distortion compared with traditional plain films and by simpler acquisition compared with traditional CT systems. Similar to the panoramic radiograph, CBCT can be used for preoperative risk assessment in various dentoalveolar procedures such as third molar surgery or dental implants and preprosthetic surgery. A major limitation, of course, remains the inability to visualize the IAN itself (within the inferior alveolar canal), or the LN, because no accurate soft tissue information can be obtained with use of CBCT ( Fig. 4 ).

High-Resolution Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is the method of choice for visualization of all cranial nerves (CN), and each nerve segment can be seen and examined in detail with specific MR sequences. Due to the complexity of the course and surrounding anatomic structures, detailed examination of the CNs is made possible only with careful planning and selection of the specific MRI technique. The imaging plane, coil selection, slice selection, in-plane resolution, and use of special techniques can be tailored based on the individual CN and the segment of interest so that the highest possible image quality may be obtained. The trigeminal nuclei (intra-axial), cisternal (preganglionic), and Merckel cave (intradural) segments contain both the motor and sensory components of the trigeminal nerve and can be visualized with high-resolution T1- or T2-weighted MR images. At the anterior aspect of the Gasserian ganglion, the sensory root divides into the ophthalmic, maxillary, and mandibular divisions, and each may be followed and examined separately based on their known course peripherally. The course of the LN and IAN branches of the mandibular division, after it exits from foramen ovale, can be followed with high-resolution, contrast-enhanced, T1-weighted (T1W), or T1W 3-dimensional, fast-filled echo (T1W 3D-FFE) sequences in the axial, coronal, and sagittal or parasagittal planes. Although detailed information can be obtained with the use MRI, routine presurgical evaluation of the route and integrity of the LN and IAN is not undertaken. Rather, the MRI is employed as the preferred imaging modality for examination of the status of the CNs, most commonly in the presence of a disease process or following brain injury.
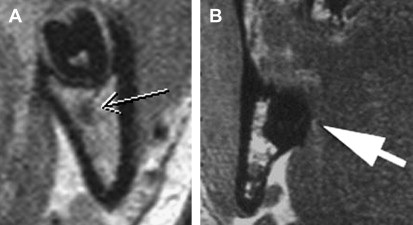
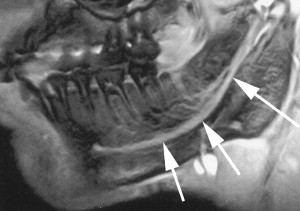
Miloro and colleagues have used high-resolution MRI (HR-MRI) in an attempt to document the in situ position of the LN in the third molar region directly, without surgical manipulation or tissue distortion artifact as in the studies by Kisselbach and Pogrel. Ten patients (20 sides) without prior dental surgery were imaged using an HR-MRI sequence (PETRA-phase encoded time reduction acquisition) that enabled direct visualization of the LN ( Fig. 5 ). This study documented that the lingual nerve position, while variable, was indeed vulnerable during third molar surgery; the LN was found to be superior to the lingual crest in 10% of cases, and in direct contact with the lingual plate in 25% of cases. Kress and colleagues have been able to image the IAN using T2-weighted MRI to visualize the IAN ( Fig. 6 ).