Introduction
In this randomized, placebo-controlled clinical trial, we investigated the effect of noninvasive extracorporeal shock waves on the stability of temporary anchorage devices (TADs) under orthodontic loading.
Methods
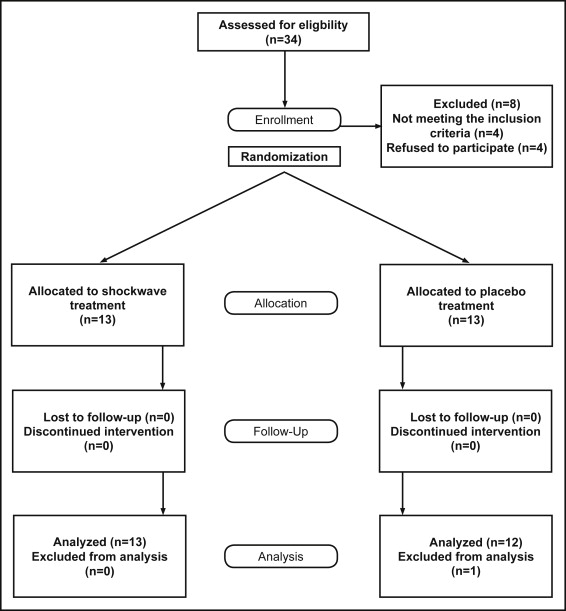
Thirty adult orthodontic patients of the Bernhard Gottlieb University Clinic in Vienna, Austria, were enrolled in this clinical trial and allocated by block randomization (size, 4) in a 1:1 ratio to either the treatment or the placebo group. Randomization was performed with software, and the allocations were concealed in sealed envelopes. Eligibility criteria included healthy adult patients with mesially directed orthodontic movement of the mandibular second molar into the extraction site of the mandibular first molar. The fixed orthodontic devices included active superelastic coil springs (200 cN) and TADs in the mandibular alveolar bone. Blinding was performed for the subjects and the outcome assessor. The treatment group received 1 shock-wave application with 1000 impulses at 0.19 to 0.23 mJ per square millimeter in the region of the TADs. The placebo group was treated with a deactivated shock-wave applicator and acoustic sham. The TADs positions were evaluated at placement and after 4 months. The reliability and precision of the impression process of the TADs were evaluated in an in-vitro model.
Results
Thirteen participants finished the investigation successfully in the treatment group but only 12 finished in the placebo group because 1 TAD loosened. The difference of the total TAD displacement for the 4-month time period between the placebo and treatment groups was 0.17 ± 0.95 mm (95% CI: −0.96, 0.62). No statistically significant difference between the 2 groups was found when sex was evaluated. Primary stability of the TADs as measured by placement torque, amount of tooth movement, and age of the patients did not influence displacement of the TADs. The reliability and precision of TAD impressions were confirmed. No unintended pernicious effects occurred after shock-wave treatment during the study period.
Conclusions
A single application of extracorporeal shock-wave treatment did not improve the stability of the TADs during orthodontic loading. Sufficient interradicular space should be provided to minimize the risk of periodontal and dental root defects.
Registration
This trial was registered at https://clinicaltrials.gov .
Protocol
The protocol was published before trial commencement, NCT01695928 .
Funding
No funding or conflict of interest to be declared.
Highlights
- •
Extracorporeal shock-wave treatment did not improve TAD stability during orthodontic loading.
- •
Sufficient interradicular space should be provided to minimize the risk of periodontal and root defects.
- •
The absence of side effects allows for further shock-wave investigations in the oral cavity.
Over the last decade, temporary anchorage devices (TADs) have become an essential tool in orthodontics as an alternative to compliance-dependent devices such as extraoral headgear traction and intermaxillary elastics. Various types of TADs are being used as aids in critical anchorage situations. The success of any TAD will depend on several factors such as diameter, length, placement site, placement torque, inflammation, mobility, distance to the root, and soft-tissue type. Recently, a meta-analysis described a success rate of 88%, whereas success rates in systematic reports have ranged between 80% and 100%. However, these high success rates might not be representative for clinical settings, because loose TADs were also included in these numbers. This must be borne in mind, since several studies have reported displacement of TADs under orthodontic loading, which can also affect the surrounding tissue. This issue is even more significant because most TADs are in contact with the periodontal ligament after placement. Hence, an unstable TAD position might result in its loosening, periodontal defects, or root damage; consequently, a stable position of the TAD during orthodontic treatment is of major importance.
Extracorporeal shock waves have become the treatment of choice for kidney and urethral stones in medicine as well as for the recovery of pseudoarthrosis after long-bone fractures, for tendinopathies, and for wound healing. Shock waves can induce osteogenesis, angiogenesis, and revascularization, but their local and systemic molecular and cellular effects are still unclear.
The effect of extracorporeal shock waves has already been investigated in dentistry. In animal models, shock-wave therapy showed a microbicidal effect against Streptococcus mutans and Porphyromonas gingivalis . Recently, Hazan-Molina et al, Kohno et al, and Iwasaki et al investigated the effect of extracorporeal shock waves on tooth movement in an in-vitro model and found a significant increase of selected cytokines: ie, VEGF and interleukin-1β. Furthermore, a bone regenerative effect was found when extracorporeal shock waves were applied after artificial trauma. Thus, shock waves might have a positive effect on TAD stabilization, accelerating the bone formation process from primary stability to secondary stability.
Specific objective and hypothesis
The purpose of this study was to investigate the effect of noninvasive extracorporeal shock-wave therapy on TAD stability. The null hypothesis stated that shock-wave therapy does not stabilize the position of TADs.
Material and methods
Trial design
The study design defined the investigation as a single-center, randomized, placebo-controlled trial with a 1:1 allocation ratio performed at the University Clinic of Dentistry in Vienna and approved by the institutional review board (EK 134/2011). The protocol was registered at ClinicalTrials.gov ( NCT01695928 ) of the US National Institutes of Health, and this article was written according to the CONSORT statement.
Participants, eligibility criteria, and setting
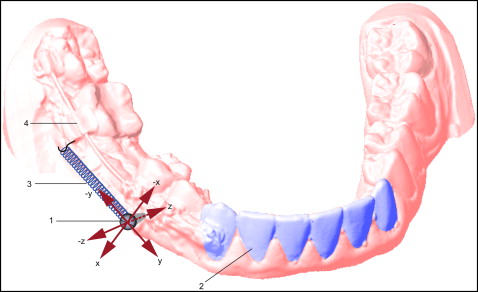
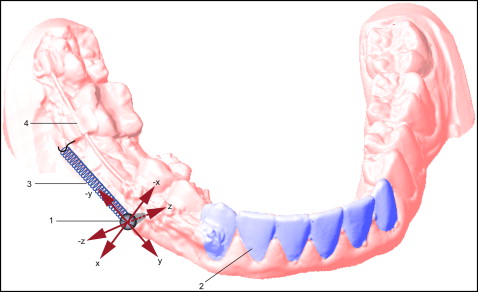
All study subjects provided informed consent. They were healthy adults undergoing comprehensive orthodontic treatment ( Fig 1 ). The women had a pregnancy test (Femtest; Omega Teknika, Dublin, Ireland) before inclusion. The inclusion criteria defined patients with mesially directed orthodontic movement of the mandibular second molar into the extraction site of the mandibular first molar facilitated by a TAD (Dual Top G2, 1.6 × 8-mm, self-drilling; Jeil Medical, Seoul, Korea). The insertion site of the TAD was between the mandibular first and second premolars in the attached keratinized gingiva.
The full-fixed orthodontic appliance included a self-ligating bracket system (Smartclip, 0.022-in slot; 3M Unitek, Monrovia, Calfi), an 0.018 × 0.025-in stainless steel archwire (SDS; Ormco, Glendora, Calif) connecting the posterior and anterior tooth segments, an 0.018 × 0.025-in stainless steel lever arm (SDS; Ormco) inserted in the auxiliary tube of the molar attachment, and an active superelastic coil spring (Sentalloy; GAC Dentsply, Bohemia, NY) between the second molar and the TAD, delivering a continuous force of 200 cN.
Interventions
The insertion of the TAD was done transmucosally under local anesthesia (Ultracain dental forte; Sanofi Aventis, Paris, France) between the first and second premolars in the keratinized gingiva with a screwdriver perpendicular to the alveolar bone, including primary stability measurement: ie, placement torque (TSD Torque screwdriver; Checkline Europe, Enschede, The Netherlands). All TADs were inserted to the contact between the TAD collar and attached gingiva. Root proximity was evaluated radiographically before and after TAD placement to check for sufficient space for insertion and exclude a contact between the TAD and the adjacent root surface at the end of the investigation. The mandibular anterior teeth were bonded lingually with a passive 0.022-in stainless steel retainer wire (Wildcat wire; GAC Dentsply), also serving as the reference area for TAD displacement measurement.
Outcomes (primary and secondary) and any changes after trial commencement
The major outcome of this trial was the TAD displacement measurement. Therefore, impressions of the mandibular dental arch (Flexitime easy putty; Heraeus Kulzer, Hanau, Germany) were taken twice: immediately after TAD placement and 4 months later with a bisected impression tray (Align Technology, San Jose, Calfi). Impression caps (Transfer caps; Tiger-Dental, Bregenz, Austria) were positioned on the TADs. Extraorally, the TADs were put into the TAD impression caps before manufacturing the dental casts. A strip-light scanner (S600 ARTI; Zirkonzahn, Gais, Italy) was used to scan the dental casts of the mandible digitally. A 3-dimensional analysis of TAD displacement was performed using the Onyx Ceph software (Image Instruments, Chemnitz, Germany). The TAD head position and the incisal edges of the rigidly connected mandibular anterior teeth were registered at the beginning and end of the observation period ( Fig 2 ). The relative position of the TAD was evaluated in 3 dimensions. The x-axis represented the vertical (DX), the y-axis the sagittal (DY), and the z-axis the transverse (DZ) displacements of the TAD. The difference between the start and end positions of the TAD represented the total TAD displacement (DR). The systematic error for scanning and digitizing the dental casts was 0.05 mm. The random error for repeated positioning of the same measuring point on the digitally scanned dental casts was 0.1 mm.
The proximity of the TAD insertion site was evaluated for swelling and bleeding at the end of the observation period. Swelling of the gingiva was defined as a proliferation above the TAD collar. Bleeding was evaluated immediately after probing on 2 opposing TAD positions with a calibrated periodontal probe (click-probe; KerrHawe, Bioggio, Switzerland).
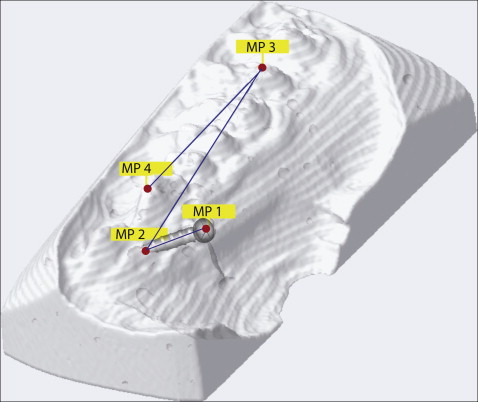
The accuracy and reliability of the TAD impression was investigated separately in an in-vitro study. TAD placement was performed on 6 pig jaws, including 2 separate TAD impressions of each TAD, dental cast manufacturing, and digital scanning as described above. The pig jaws were x-rayed for reference with computed tomography (CT) (Somatom Sensation 4; Siemens, Forchheim, Germany). The measurements were performed digitally between the 2 digital dental cast scans and the CT scans for each TAD on the 4 reference points shown in Figure 3 . Each dental cast scan was the iterative closest point superimposed with the outer surface rendered in the corresponding CT scan by a marching cube isosurface algorithm. Surface landmarks MP 1, MP 3, and MP 4 were digitized manually on the scanned or rendered surface by visual feature identification. Landmark MP 2 was used to define the TAD axis direction and digitized in the CT volume as far as possible from the TAD head. All data were stored digitally in a computer (MacBook Pro; Apple, Cupertino, Calif).
For the single shock-wave intervention ( Fig 4 ), all subjects received topical anesthesia (xylocain 2% gel; Astra Zeneca, Vienna, Austria) in the vestibulum between the second molar and the canine. Sonic gel liquid (Gerasonic; Gerot Pharmazeutika, Vienna, Austria) was applied on the cheek as a conduction medium. An ear protector reduced the acoustic disturbance. The subjects of the treatment group were treated with 1000 impulses of extracorporeal shock waves at an energy flux density of 0.19 to 0.23 mJ per square millimeter, with a pulse rate of 5 pulses per second by a focused shock wave device (Orthogold 100; MTS/TNT, Konstanz, Germany). These parameters were defined according to previous shock-wave studies focusing on bone regeneration. Shock waves interfuse soft tissues (silicone membrane of the applicator, skin, cheek, gingiva) and liquids (water, sonic gel liquid, saliva) almost without any loss of energy reaching the alveolar bone where the focus is positioned. At the energy flux densities used, the focal area has an elliptical shape with a length of about 3 cm and a diameter of 6 to 7 mm.

In the placebo group, the subjects were treated with an acoustic sham of the extracorporeal shock wave with the same pulse rate, volume level, and treatment time; the shock-wave applicator was used in deactivated form and in the same manner as in the treatment group.
Sample size calculation
The sample size for this clinical trial was calculated according to the study of Liou et al, who investigated TAD displacement (primary outcome) under orthodontic loading using a 2-sided t test. The number of patients was 15 per group to detect 0.8 mm of displacement (SD, 0.8 mm) at an alpha level of 0.05 and power of 80%.
Interim analyses and stopping rules
Not applicable.
Randomization (random number generation, allocation concealment, implementation)
All patients with a TAD for molar mesialization in the mandible were included in this trial. Block randomization (size, 4) was used to allocate patients to treatment or placebo intervention with digital randomization software (Randomizer, version 1.8.1; Institute for Medical Informatics, Statistics and Documentation, Medical University of Graz, Austria). The random allocation sequence was printed. The treatment allocation cards were sealed in envelopes with the participants’ initials and ages written on the outside of the envelope. Then the envelopes were locked until the start of treatment. This process was performed and monitored by 1 operator (C.A.).
Blinding
Blinding was performed for the subjects as described and for the outcome assessor (C.K.). Blinding of the shock-wave therapist was not established. The results of the measurements were coded by 1 operator for the outcome assessor to ensure blinding.
Statistical analysis (primary and secondary outcomes, subgroup analyses)
The statistical analysis was performed using the Wilcoxon 2-sample test to detect significant differences of TAD displacement in both sexes in the treatment and placebo groups. Associations between total TAD displacement and primary TAD stability, total tooth movement of the mandibular second molar, and age of the participants were analyzed using univariate linear regression for each covariable. The linear tooth movement after the 4-month observation period was measured using defined landmarks (both mesial cusps of the mandibular second molar and the canine cusp).
To assess the accuracy of the TAD impression process in each direction, differences in this direction between the dental cast scan values and the CT pig jaw values in all points were pooled, and mean differences and standard deviations were determined. To assess the reliability of the TAD impression process, differences in each direction between the first and second dental cast scan values in all points were pooled, and means and standard deviations were determined. For assessing the significance of the measured movements of the TAD vs the precision of measurement, variances of the observed displacements were compared with variances between measurements of fixed points for each direction by F-tests. In addition, an intraclass correlation coefficient (ICC) was calculated between the repeated impression measurements.
All statistical calculations were performed with SAS enterprise guide (version 5.1; SAS Software, Cary, NC) and R 3.0.1 (R Foundation for Statistical Computing, Vienna, Austria).
Material and methods
Trial design
The study design defined the investigation as a single-center, randomized, placebo-controlled trial with a 1:1 allocation ratio performed at the University Clinic of Dentistry in Vienna and approved by the institutional review board (EK 134/2011). The protocol was registered at ClinicalTrials.gov ( NCT01695928 ) of the US National Institutes of Health, and this article was written according to the CONSORT statement.
Participants, eligibility criteria, and setting
All study subjects provided informed consent. They were healthy adults undergoing comprehensive orthodontic treatment ( Fig 1 ). The women had a pregnancy test (Femtest; Omega Teknika, Dublin, Ireland) before inclusion. The inclusion criteria defined patients with mesially directed orthodontic movement of the mandibular second molar into the extraction site of the mandibular first molar facilitated by a TAD (Dual Top G2, 1.6 × 8-mm, self-drilling; Jeil Medical, Seoul, Korea). The insertion site of the TAD was between the mandibular first and second premolars in the attached keratinized gingiva.
The full-fixed orthodontic appliance included a self-ligating bracket system (Smartclip, 0.022-in slot; 3M Unitek, Monrovia, Calfi), an 0.018 × 0.025-in stainless steel archwire (SDS; Ormco, Glendora, Calif) connecting the posterior and anterior tooth segments, an 0.018 × 0.025-in stainless steel lever arm (SDS; Ormco) inserted in the auxiliary tube of the molar attachment, and an active superelastic coil spring (Sentalloy; GAC Dentsply, Bohemia, NY) between the second molar and the TAD, delivering a continuous force of 200 cN.
Interventions
The insertion of the TAD was done transmucosally under local anesthesia (Ultracain dental forte; Sanofi Aventis, Paris, France) between the first and second premolars in the keratinized gingiva with a screwdriver perpendicular to the alveolar bone, including primary stability measurement: ie, placement torque (TSD Torque screwdriver; Checkline Europe, Enschede, The Netherlands). All TADs were inserted to the contact between the TAD collar and attached gingiva. Root proximity was evaluated radiographically before and after TAD placement to check for sufficient space for insertion and exclude a contact between the TAD and the adjacent root surface at the end of the investigation. The mandibular anterior teeth were bonded lingually with a passive 0.022-in stainless steel retainer wire (Wildcat wire; GAC Dentsply), also serving as the reference area for TAD displacement measurement.
Outcomes (primary and secondary) and any changes after trial commencement
The major outcome of this trial was the TAD displacement measurement. Therefore, impressions of the mandibular dental arch (Flexitime easy putty; Heraeus Kulzer, Hanau, Germany) were taken twice: immediately after TAD placement and 4 months later with a bisected impression tray (Align Technology, San Jose, Calfi). Impression caps (Transfer caps; Tiger-Dental, Bregenz, Austria) were positioned on the TADs. Extraorally, the TADs were put into the TAD impression caps before manufacturing the dental casts. A strip-light scanner (S600 ARTI; Zirkonzahn, Gais, Italy) was used to scan the dental casts of the mandible digitally. A 3-dimensional analysis of TAD displacement was performed using the Onyx Ceph software (Image Instruments, Chemnitz, Germany). The TAD head position and the incisal edges of the rigidly connected mandibular anterior teeth were registered at the beginning and end of the observation period ( Fig 2 ). The relative position of the TAD was evaluated in 3 dimensions. The x-axis represented the vertical (DX), the y-axis the sagittal (DY), and the z-axis the transverse (DZ) displacements of the TAD. The difference between the start and end positions of the TAD represented the total TAD displacement (DR). The systematic error for scanning and digitizing the dental casts was 0.05 mm. The random error for repeated positioning of the same measuring point on the digitally scanned dental casts was 0.1 mm.