I
-iasis Suffix denoting a diseased condition e.g. elephantiasis (a rare disorder of the lymphatic system caused by parasitic worms).
iatro- Prefix denoting medicine or doctors.
iatrogenic adj. Describing an unforeseen or unwanted side-effect of treatment provided by a health professional.
ibuprofen n. A proprionic acid derivative in the non-steroidal anti-inflammatory drug (NSAID) category. It binds extensively to plasma proteins and is rapidly absorbed following oral administration. It has *analgesic, anti-inflammatory, and *antipyretic properties and is used in the treatment of musculoskeletal, dental, and rheumatic pain. It is also a popular post-operative analgesic. Trade names: Brufen, Fenbid, Junifen, Nurofen.
ICON See INDEX OF COMPLEXITY OUTCOME AND NEED.
identification dot A small elevation or pimple on the corner of a radiographic film used to indicate the surface of the film facing the x-ray tube during exposure.
idiopathic adj. (n. idiopathy) Describing a disease or medical condition of unknown cause or which occurs spontaneously.
idiosyncrasy n. (adj. idiosyncratic) An unusual and unexpected sensitivity reaction by an individual to a particular food, drug, or cosmetic. Drug idiosyncrasy occurs when the standard dose causes an excessive response.
imbalance n. A disharmonious relationship between two or more functional systems, structures, or organs.
imbibition n. (v. imbibe) The absorption of liquid by a solid or a gel. For example, *glass ionomer cement undergoes imbibition of water during its early setting phase.
imbrication n. (in dentistry) Anterior teeth in the same arch which overlap each other. Imbrication lines are mesio-distal ridges on the cervical third of the labial surface of an anterior tooth associated with enamel incremental growth formation. See also STRIAE OF RETZIUS. 
immediate denture n. See DENTURE.
immediate life support (ILS) See BASIC LIFE SUPPORT.
immobilization n. See FIXATION.
immune response (reaction) n. The bodily defence reaction of an organism that recognizes an invading substance (*antigen) such as a virus, fungus, bacteria, or transplanted organ, and produces an *antibody specific against that antigen. There are two types of immune response: B-lymphocytes (or B-cells) are responsible for humoral immunity producing free antibodies that circulate in the bloodstream; T-lymphocytes (or T-cells) are responsible for cell-mediated immunity.
immune system n. The organs and tissue responsible for *immunity. The non-specific immune system is made up of a primary barrier consisting of the skin and mucosa and a secondary barrier consisting of inflammatory cells and soluble factors. The third barrier is the specific immune system which includes the thymus, bone marrow, spleen, tonsils, and lymph nodes.
immunity n. The ability of the body to resist infection due to the presence of circulating *antibodies and white blood cells. Natural (innate or non-specific) immunity is a defence mechanism which includes natural, mechanical, chemical, and biological barriers to infection and which has no degree of memory or specificity; it is present at birth prior to exposure to infective agents. Acquired immunity is achieved in response to foreign *antigens in the body and involves the production of *antibodies which react specifically with the foreign antigen. Active immunity is achieved when the body’s own cells produce and continue to produce appropriate antibodies in response to an infection or to artificial stimulation by the use of treated antigens to stimulate the body to produce its own antibodies (*immunization, *vaccination). Passive immunity is of short duration and occurs naturally at birth from maternal antibodies in the mother’s milk (colostrum) and placental blood or by the injection of antibodies contained in antiserum taken from another immune person or animal.
immunization n. The production of *immunity by artificial means. It may be achieved actively or passively.
immunodeficiency n. A condition resulting from a reduced or deficient *immune response. This may be a primary condition due to a defect in the immune system or a secondary (or acquired) condition as a result of a disease process such as *AIDS.
immunoglobulins n. A group of structurally related serum proteins synthesized by *plasma cells which act as *antibodies.
immunosuppressant n. A drug or agent that reduces the *immune response. They are useful in maintaining the survival of transplanted organs or tissues which would otherwise be rejected and destroyed by the immune response, and for treating certain *autoimmune diseases such as rheumatoid *arthritis.
impaction n. The condition of being tightly wedged together. Food impaction can occur between the teeth due to an open contact, a poorly contoured restoration, or the plunger effect of opposing teeth. Tooth impaction occurs when a tooth is prevented from erupting into a fully functional position. The preventing agent can be another tooth, alveolar bone, or soft tissues. The most commonly impacted teeth are third molars, second premolars, and canines; the impacted tooth may lie in a variety of different positions. 
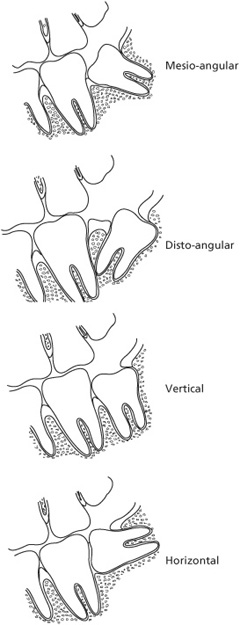
Types of impacted lower third molars
impairment n. Any loss or abnormality of psychological, physiological, or anatomical structure or function. It represents a deviation from a person’s usual biomedical state. An impairment is thus any loss of function directly resulting from injury or disease. A social model defines impairment as the functional limitation within an individual caused by restricted physical, mental, or sensory activity. Compare DISABILITY; HANDICAP.
impetigo n. A superficial bacterial infection of the skin. It is characterized by small pus-filled blisters that form a yellow crust, usually around the nose and mouth. Non-bullous impetigo is caused by Staphylococcus aureus or Streptococcus species or both, is highly contagious, and occurs mainly in young children. Bullous impetigo is caused by Staphylococcus aureus, is less contagious, and can occur at any age. Treatment is usually by topical antibiotics.
impingement n. The unusually forceful application of food, teeth, foreign objects, etc. onto tissues, teeth, or prostheses.
|
implant |
|
n. (in dentistry) A device specifically designed to be placed surgically within or on the mandibular or maxillary bone as a means of providing retention for a prosthetic replacement of one or more teeth. Implants may be broadly classified into three groups: subperiosteal, which rest on the surface of the bone beneath the *periosteum and mucosa; transosteal, which penetrate the inferior border of the mandible and project through the oral mucosa covering the edentulous ridge; and endosteal (endosseous), which are embedded in the maxillary or mandibular bone and project through the oral mucosa covering the edentulous ridge. A subperiosteal implant used to be indicated when the bone had atrophied and the jaw structure was limited; however, it has now been superseded by the endosteal implant. A subperiosteal implant had a lightweight, individually designed, metal framework fitting over the remaining bone with metal posts that projected through the soft tissue into the oral cavity, providing the equivalent of multiple tooth roots; they were used in a limited area or, if all the teeth were missing, in the entire mouth to retain a complete denture. The potential contraindicating risk factors of this type of implant were bone resorption, injury to nerves causing *paraesthesia, fracture of the mandible, and soft tissue inflammation. An endosteal implant is placed directly into the jaw bone and the intraosseous part generally has a blade or root shape. Implant material is usually machined *titanium with a modified surface such as a titanium plasma spray (TPS) or *hydroxyapatite coating. Bioceramic materials are less commonly used. |
|
The blade implant, made of steel and used mostly for partially dentulous patients, was an endosteal implant developed in the late 1950s and was narrow bucco-lingually, with the blade following the arch of the jaw bone with openings or vents through which the bone could grow; it resulted in a connective tissue capsule around the implant rather than true *osseointegration with the surrounding bone. These implants have been superseded by titanium implants capable of true osseointegration following the work of PerIngvar Branemark, a Swedish orthopaedic surgeon, started in 1952. The core-vent implant system is an endosseous implant system in which the implant is made of titanium. The portion of the implant retained in the bone has a hollow vent and the part protruding above the soft tissues is machined to receive a prosthetic abutment. An endodontic (diodontic) implant is a metallic implant that extends through the root canal of a tooth into the periapical cortical bone to provide increased retention and decreased tooth mobility. It is used to stabilize and retain natural teeth and may be smooth, tapered, threaded, or have a porous surface. The intra-dental portion is cemented in position. The IMZ (Intramobile Zylinder) implant is an endosseous implant system introduced in 1987 and consisting of a cylindrical intra-bony element and a polyoxymethylene coated stress-breaking component, called an intramobile element, to allow implant connection to natural teeth. The root-shaped endosteal implant mimics the basic shape of the natural tooth root and is manufactured in a variety of shapes, sizes, and lengths. An endosteal implant requires at least 1mm of bone between it, the adjacent teeth, and the buccal and palatal alveolar plates. |
|
A self-tapping implant is an endosteal implant which cuts its own path through bone tissue. The staple implant is an example of a transosteal implant which is retained by fixation screws tapped into the anterior region of the mandible from the lower surface to provide a number of pins penetrating the alveolar ridge and mucous membrane, to which a bar may be attached to retain a complete or partial denture. Implant placement may be undertaken either as a one-stage technique (early loading) in which the implant is placed into a new, healing, or healed extraction site and is visible above the oral mucosa immediately after placement (this avoids the necessity of a second surgical stage to expose the implant), or a two-stage technique in which the implant is placed into a new, healing, or healed extraction site and then covered by the oral mucosa so that it cannot be seen; at a second stage between one week and two months later (early loading) or after two months (conventional loading), allowing time for osseointegration to take place, the implant is uncovered and intra-oral components added to allow the placement of one or more restorations. See also ABUTMENT. |
Further Reading: Esposito M., Worthington H. V., Coulthard P., Thomsen P. Maintaining and reestablishing health around osseointegrated oral implants: a Cochrane systematic review comparing the efficacy of various treatments. Periodontol 2000 2003;33:204–12.
Bishop K, Addy L, Knox J. Modern restorative management of patients with congenitally missing teeth: the role of implants. Dent Update 2007;34:79–84.
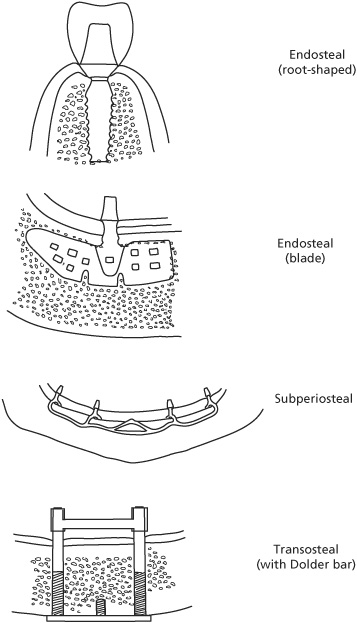
Types of implants
implantology (oral) n. A specialist branch of dentistry concerned with the surgical insertion of materials or devices into the hard or soft tissues of the oral cavity for the purpose of providing support or retention for tooth restorations or a prosthetic appliance.
implant restoration A restoration placed on an implant designed to restore normal function, aesthetics, speech, and comfort. It may be secured on the underlying implant by screw or cement retention, or a combination of the two. This allows the restoration to be removed for repair in the event of porcelain fracture, abutment fracture, or if the prosthesis needs to be modified such as when an implant has failed. The restorative prosthesis may consist of several units secured to a number of implants.
Impregum® n. The trade name for a *polyether impression material.
impression n. An imprinted mould of an object such as a tooth, arch of teeth, or edentulous ridge, obtained by pressing an *impression tray containing an *impression material over the target object, from which a positive reproduction of that object can be made. A mucodisplacive (mucocompressive, functional) impression utilizes a technique in which the denture-bearing area of the mucosa is loaded to produce a uniform reduction in volume which will be subsequently compressed during denture wearing; the impression material used is of high viscosity such as *impression compound. A mucostatic impression creates an impression of the denture-bearing tissues in their natural stateand requires a low-viscosity impression material such as *plaster of Paris or *alginate. A primary (preliminary) impression is made for diagnostic purposes or for the construction of an impression in which a more accurate secondary impression can be taken; preliminary impressions may also be taken in order to construct a *model on which a custom-made impression tray can be fabricated for the purposes of taking a more accurate secondary impression. A dual impression technique is a method of taking an impression in layers using impression materials of different viscosities, chosen appropriate to the character and mobility of the soft tissues so as to provide differential compression. A working (secondary or final) impression is an accurate impression usually taken in a custom-made *impression tray used for making a master cast. A sectional impression is made in two or more parts. A pick-up impression is an accurate impression taken with an implant superstructure or one or more crown *copings in place so that they are included in the impression material; it provides an accurate impression of the oral mucosal tissue and the location of the metallic superstructure relative to the crown preparations or implants.
impression compound n. A material composed of fatty acids, shellac, glycerine, and filler used as a primary *impression material. When heated in a water bath at about 65°C (149°F) it becomes plastic and can be moulded in an impression tray and inserted in the mouth. The material becomes fairly rigid on cooling to mouth temperature and has low material flow at room temperature. It has a low thermal-expansion coefficient so that there is minimal dimensional change as the impression is cooled from mouth temperature and it does not adhere to moist oral tissue. It may be modified by the addition of an *alginate wash. Impression compound is usually used for taking primary impressions of the edentulous ridge prior to the construction of a custom-made *impression tray for complete *dentures. Impression compound is also available in sticks of various colours indicating different softening temperature ranges e.g. greenstick compound (composition); these are used for impression correction and moulding the borders of custom impression trays, particularly around muscle attachments.
impression material n. Any substance used for making a negative mould of a structure. Rigid impression materials are inflexible and are usually used to take impressions of structures which have no undercut surfaces such that when removed the material is not required to be deformed; such materials include *plaster of Paris, *impression compound, *zinc oxide, and *wax. Elastic impression materials are capable of deformation with minimal distortion; materials commonly used are reversible and irreversible *hydrocolloid, *silicone, *polyether, and mercaptan (*polysulphide). Syringable impression material may be used for obtaining an *occlusal record.
Further Reading: Stewardson D. A. Trends in indirect dentistry: 5. Impression materials and techniques. Dent Update 2005;32(7):374–6, 379–80, 382–4.
impression tray n. A rigid receptacle in which impression material is placed. Materials commonly used for impression trays are metal, *shellac, or resin. They are usually coated with tray adhesive immediately prior to use and may be perforated with 2–4mm diameter holes or made from metallic mesh to improve the adhesion of the impression material to the tray. Stock trays are rigid trays commercially manufactured in different sizes and shapes and usually made of resin or metal. Edentulous stock trays have a shape which conforms to the shape of the edentulous ridge of either the mandible or maxilla. Dentate stock trays have a box shape to accommodate the teeth in the arch. Custom trays are made from a primary cast and, because their shape conforms more closely to the shape of the teeth and tissues to give a more uniform thickness of impression material, it provides greater dimensional accuracy. Custom trays are usually made from shellac or resin. A sectional tray is used to take an impression of a specific area of the dental arch such as a quadrant or sextant.
IMZ implant system n. See IMPLANT.
incidence n. The number of occurrences of a disease, condition, or event within a defined time interval. The incidence rate is the number of cases of a specific disease, condition, or event diagnosed or reported during a defined period of time, divided by the number of people at risk for the disease.
incipient adj. In an initial stage; beginning to become apparent.
incisal adj. Relating to the cutting edge of an anterior tooth (incisor or canine). The incisal edge is the biting edge of an incisor or canine. The incisal angle is the angle between the incisal edge and the mesial or distal surface of an anterior tooth. The incisal guide table forms the base for the incisal guide *pin on an *articulator. Incisal guidance is the influence on mandibular movements caused by the contacting surfaces of the mandibular and maxillary anterior teeth during masticatory movements (eccentric excursions from centric *occlusion).
incision n. 1. The act of making a cut in body tissue. 2. The cutting action of incisor teeth.
incisor, permanent mandibular central n. One of two teeth which are the smallest in the permanent *dentition located between the mandibular lateral incisors either side of the midline. They replace the mandibular primary central incisor teeth. It has a convex labial surface with a flattened area in the incisal half. The lingual surface is concave, except above the cervical margin where it is convex. Unlike the upper central incisors, there is no well-defined *cingulum and no definite marginal ridges on the lingual surface. The mesial and distal surfaces of the crown are triangular in shape, to give a wedge-shaped appearance, and are almost at right angles to the incisal edge. On *eruption, the incisal edge has three small tubercles (*mamelons), which wear away to give a flat surface. It has a single root, oval in cross-section and flattened on the mesial and distal surfaces. The apical region may show some degree of bifurcation. The *pulp chamber has two mesial and distal pulp horns directed towards the mesial and distal angles of the incisal edge. The root canal is subject to variation and may divide to give buccal and lingual canals. *Calcification of the tooth begins at about 3–4 months after birth and the crown is normally complete by 4–5 years of age. The tooth erupts at about 6–7 years and the calcification of the root is complete at about 9–10 years.
incisor, permanent mandibular lateral n. One of two teeth located between the mandibular central incisors and the canines in the permanent dentition. They replace the mandibular primary lateral incisor teeth. It is similar to the lower central incisor but is wider mesio-distally and therefore more fan-shaped. The lingual surface usually shows more definite mesial and distal marginal ridges. On *eruption, the incisal edge has three small tubercles (*mamelons), which wear away to give a flat surface. *Calcification of the tooth begins at about 3–4 months after birth and the crown is normally complete by 4–5 years of age. The tooth erupts at about 7–8 years and the calcification of the root is complete at about 10 years.
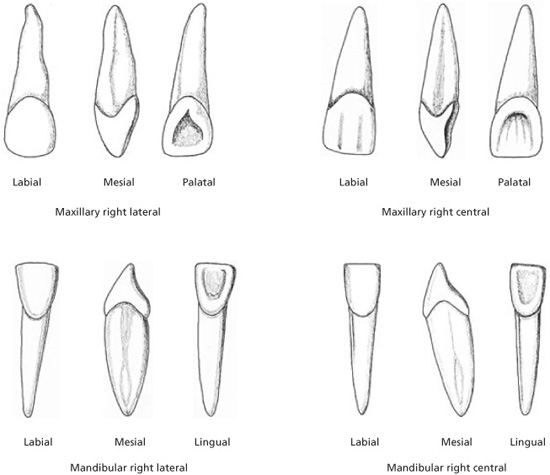
Permanent incisors
incisor, permanent maxillary central n
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



