Fungal infections
Publisher Summary
A variety of diseases that are caused by fungi might appear in the oral and perioral regions, either as localized lesions or as manifestations of systemic mycoses. However, candida infections of the oral cavity are the predominant group of fungal infections, which the dental practitioners frequently encounter; although rare mycoses, such as blastomycosis and mucormycosis might be seen, particularly in immunocompromised and sometimes in immigrant population groups. This chapter focuses on candida infections of the oral mucosa; it discusses the uncommon mycoses. A number of local and general predisposing factors play a contributory role in the pathogenesis of oral fungal infections. Debilitated individuals, such as those receiving antibiotics, steroid, or cytotoxic therapy, are particularly predisposed, as are patients with uncontrolled diabetes mellitus, other hormonal disorders such as hypoadrenocorticism, and haematogenous and malignant disorders. Certain age groups, especially the young and the old, and the pregnant are prone to oral yeast infections.
A variety of diseases caused by fungi may appear in the oral and perioral regions, either as localized lesions or as manifestations of systemic mycoses. However, candida infections of the oral cavity are by far the predominant group of fungal infections which the dental practitioners in the Western world frequently encounter, although rare mycoses such as blastomycosis and mucormycosis may be seen, particularly in immunocompromised and sometimes in immigrant population groups. Hence, the emphasis of this chapter is on candida infections of the oral mucosa; the uncommon mycoses are briefly discussed at the end of the chapter (and see Table 9.5).
Table 9.5
Uncommon systemic mycoses and their oral manifestations
| Disease and representative agent | Main sites affected | Major oral manifestations | Frequency of oral affection |
| Aspergillosis Aspergillus fumigatus | Paranasal sinuses; rarely tongue, soft palate | Plaque formation and intense local pain in oral lesions | Uncommon |
| Blastomycosis (North American)Blastomyces dermatitidis | Tongue, oral mucosa, gingivae, lip, mandibular bone | Ulceration, sessile projections, indurated swellings, actinomycosis like draining abcesses | Rare |
| Coccidioidomycosis Coccidioides immitis | Nasolabial folds, skin | Verrucous granulomas’ resembling carcinomas | Very rare |
| CryptococcosisaCryptococcus neoformans | Gingiva, hard and soft palate, mucosa, tonsillar pillar | Violaceous coloured nodules orgranulations, swellings, ulcers | Uncommon |
| Geotrichosis Geotrichum candidum | Oral mucosa | Similar to acute pseudomembranes of candidosis | Uncommon |
| HistoplasmosisbHistoplama capsulatum Histoplasma duboisii | Oral mucosa, tongue, palate, gingiva, periapical area | Nodular, indurated or granular masses or tissue destruction with bone erosion | 40% |
| Mucormycosis Mucor species | Extension from maxillary sinus through palate into the mouth | Sloughing ulcers with grey eschar and exposed bone (especillary maxilla); unilateral facial pain. | Common |
| Paracoccidioidomycosis(South American blastomycosis)Paracoccidioides brasiliensis | Hard and soft palate, gingiva, tongue | Papules or vesicles leading to ulcers; extensive local destruction | Common |
| Sporotrichosis Sporotrichum schenckii | Oral mucosa | Erythematous, ulcerative lesions leading to granuloma, or papillomas | Uncommon |
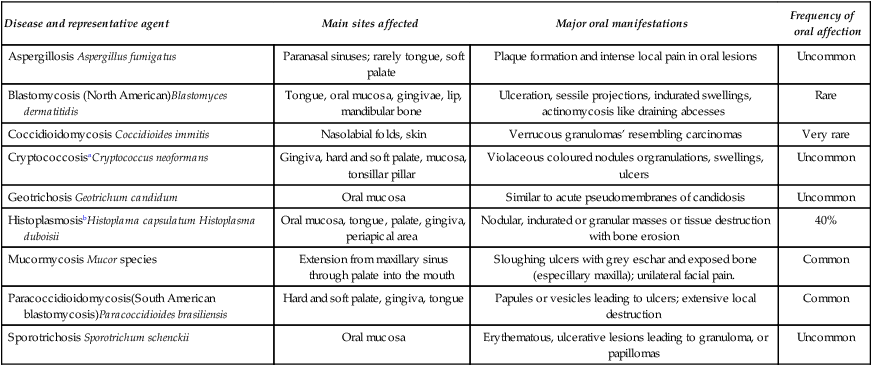
aAIDS associated oral lesions have been described.
bMay present to the dentist with initial oral manifestations.
The effects of local factors are particularly well seen in chronic atrophic candidosis. Unclean dentures which may act as the reservoir of yeasts may be an aetiological cofactor, as is mechanical trauma due to an ill-fitting denture. Local use of antibiotics and corticosteroids may predispose to oral candidosis, together with other factors which are listed in Table 9.1.
Table 9.1
Factors that predispose the host to oral candidosis
| Physiological: | Old age, infancy, pregnancy |
| Local trauma: | Mucosal irritation, denture wearing |
| Antibiotics: | Particularly broad-spectrum antibiotics |
| Corticosteroids: | Steroid inhalers, systemic steroids |
| Malnutrition: | High carbohydrate diet; deficiencies in iron, folate, vitamin B12 |
| Endocrine disorders: | Hypoendocrine states (e.g. hypothyroidism, Addison’s disease), diabetes mellitus |
| Malignancies: | Blood disorders (e.g. acute leukaemia, agranulocytosis) |
| Immune defects: | AIDS, thymic aplasia |
| Xerostomia: | Due to irradiation, drug therapy, Sjögren’s syndrome (primary and secondary), cytotoxic drug therapy |
Oral candidosis
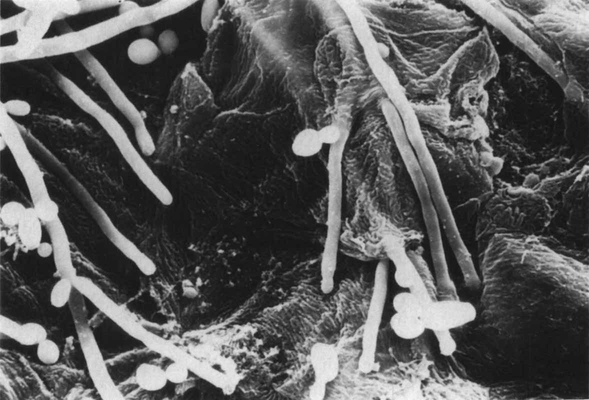
Candida albicans is a dimorphic fungus and basically exists in the classical ovoid, yeast or blastospore phase (syn. blastoconidia) and hyphal or mycelial phases (Figure 9.1). They multiply primarily by the production of buds from ovoid yeast cells. Under adverse conditions they also form spores called chlamydospores which are not usually observed in clinical specimens but can assist in the laboratory identification of yeasts.
Candidoses confined to the oral and perioral tissues
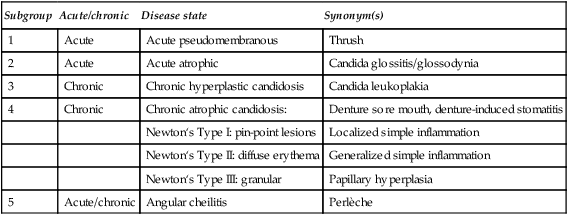
Candidoses which are relatively common but confined to the oral and perioral tissue can be classified as shown in Table 9.2.
Table 9.2
Classification of oral candidosis. Group I: Common disorders confined to the oral and perioral tissues
| Subgroup | Acute/chronic | Disease state | Synonym(s) |
| 1 | Acute | Acute pseudomembranous | Thrush |
| 2 | Acute | Acute atrophic | Candida glossitis/glossodynia |
| 3 | Chronic | Chronic hyperplastic candidosis | Candida leukoplakia |
| 4 | Chronic | Chronic atrophic candidosis: | Denture sore mouth, denture-induced stomatitis |
| Newton‘s Type I: pin-point lesions | Localized simple inflammation | ||
| Newton‘s Type II: diffuse erythema | Generalized simple inflammation | ||
| Newton‘s Type III: granular | Papillary hyperplasia | ||
| 5 | Acute/chronic | Angular cheilitis | Perlèche |
Acute pseudomembranous candidosis (thrush)
Thrush, or acute pseudomembranous candidosis, is a well-known disease entity associated with a local disturbance or systemic illness. Thrush occurs in up to 5% of newborn infants and in some 10% of elderly, debilitated individuals. In the former it is the immature host defences which mediate the disease while in the latter it could be due to one or more of the predisposing factors mentioned in Table 9.1.
Thrush has recently acquired a renewed importance as it is one of the earliest and sometimes the initial manifestation of acquired immunodeficiency syndrome (AIDS). However, in association with AIDS this lesion may persist for months and the term ’acute’ seems to be inaccurate in this context (see also Chapter 15).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses