Oral and maxillofacial surgeons must constantly weigh the risks of surgical intervention for pediatric mandible fractures against the wonderful healing capacity of children. The majority of pediatric mandibular fractures can be managed with closed techniques using short periods of maxillomandibular fixation or training elastics alone. Generally, the use of plate- and screw-type internal fixation is reserved for difficult fractures. This article details general and special considerations for this surgery including: craniofacial growth & development, surgical anatomy, epidemiology evaluation, various fractures, the role rigid internal fixation and the Risdon cable in pediatric maxillofacial trauma. It concludes with suggestions concerning long-term follow-up care in light of the mobility, insurance obstacles, and family dynamics facing the patient population.
Oral and maxillofacial surgeons have a long history of providing care for the trauma patient. This care for the maxillofacial trauma patient is one of our specialty’s greatest contributions to society as a whole. Countless residents have honed their surgical skills and patient management techniques caring for the trauma patient while providing an immense service to our patient population. The specialty of oral and maxillofacial surgery has also been responsible for trauma care in our most precious patient population, our children.
Management of maxillofacial trauma has undergone tremendous change over time. These changes have been mandated by the evolving complexity of injuries of this age as well as advances in modern imaging, instrumentation, and techniques such as rigid fixation. Perhaps the greatest impetus for change in the approaches of the surgical management of maxillofacial trauma originated through the conflicts of the World Wars. The pioneering efforts of surgeons such as Kazanjian, Converse , Gillies and Millard are examples of these advancements. Their triumphs were then moved forward and further refined by surgeons such as: Thoma, Blair, Ivy, Curtis, Dingman, Natvig, and Rowe and Killey . However, in the surgical management of pediatric craniomaxillofacial disease and deformity perhaps the greatest influence came from the contribution of Paul Tessier in his principles of cranio-orbital surgery first introduced in 1967. Gruss and colleagues and Manson and colleagues provided many of the operative principles of maxillofacial trauma employed today such as sequencing of panfacial injuries, autogenous bone grafting, and the important role of open reduction and rigid internal fixation in re-establishing facial height, width, and projection. These principles have provided the fundamental underpinnings of modern facial fracture treatment. More recently, these principles, which work so well in the adult patient, have been applied in the management of pediatric maxillofacial trauma. Posnick and Kaban have more clearly described the epidemiology and further clarified the advantages of rigid internal fixation for these injuries.
The term “pediatric” must be defined to assure that the discussion is about similar age group populations. Many health care providers consider patients under the ages of 18 or 21 as still falling within the pediatric population. Management of facial fractures in an 18-year-old patient generally follows adult principles and should not be considered pediatric management. For the sake of this discussion, the authors will follow the guidelines of the American Association of Oral and Maxillofacial Surgeons and define pediatric patients as 12 years old and younger.
Fundamentally, understanding of complex facial injuries evolved through experience, both good and bad, with adult patients. However, children are not simply “small adults” and the application of adult-type treatment can be inappropriate in many circumstances. There is still a place for conservatism in treatment of craniomaxillofacial injuries in the child.
General considerations
Craniofacial growth & development
The role of the human face is significant for reasons other than purely aesthetic considerations. Highly evolved and specialized functions of the face include vision, breathing, mastication, speech, smell, and hearing. Indeed, it is the culmination of an extremely complex process of growth and development that provides the functional and aesthetic framework of the human face. Interruption of this process, such as insult from maxillofacial injury or surgical treatment, may produce deleterious alterations of the facial framework resulting in aesthetic and functional deficits which are apparent and hard to ignore. For the surgeon who treats pediatric facial fractures, an understanding of this process becomes crucial in developing and exercising sound surgical judgment .
The mandible has both a component of endochondral ossification at the temporomandibular joint regions bilaterally, and remodeling and apposition of bone everywhere else. The mandibular body and alveolus follow the downward and forward vector of movement of the midface, but the rami and condyles grow upward and backward to maintain contact with the skull base. Vertical height is gained at the condyle through endochondral replacement and length is added though an active remodeling of the ramus. Skeletal maturity of the maxilla and mandible is reached by approximately 14 to 16 years of age in females and 16 to 18 years of age in males .
The functional matrix concept of growth first proposed by Moss has gained general acceptance . The theory, in essence, postulates that growth occurs as a result of expanding functional requirements of the cranial, nasal, and oral cavities; and that these requirements are transmitted to the bone and cartilage from the soft-tissue envelope of the face. The bones grow in response to the expansion of the cranial and facial capsule. Thus the nasal septum and mandibular condyles react to growth requirements and should not be considered the primary centers of growth as they were once professed to be. Therefore, surgical attention in managing injuries of the mandibular condyle should be directed at preserving as scar-free an envelope of soft tissue as possible and promoting function of the joint. Extending this theory to a myriad of other craniofacial problems leads to similar conclusions. A classic example of the influence of the soft-tissue envelope on growth are patients with cleft palate. Maxillary growth restriction in these patients is the result of scarring from palatal surgery. The cleft palate itself, if not operated on until skeletal maturity, would have little to no effect on maxillary growth . The importance of understanding the deleterious effects of scar tissue, traumatically or surgically induced, and restricted function on growth and development cannot be overstated when managing the child with facial fractures.
Surgical anatomy
Critical examination of the stages of gross anatomic craniofacial development leads to several particular issues that have an impact in both the epidemiology and management of facial bone injuries in children. During the early years of development, the bone itself has a very high osteogenic potential and is characterized by thick medullary space and thin bony cortices resulting in a greater likelihood of greenstick fracture. The greenstick fracture is defined as a fracture through one cortex and is almost exclusively seen in the pediatric age group. Thick periosteum allows for rapid consolidation and remodeling at the site of fracture. Comminution of fractures is rare in the pediatric population except in injuries such as gunshot wounds. The teeth in the primary dentition have particularly short, bulbous crowns that can make it difficult in achieving stable maxillomandibular fixation (MMF) during fracture reduction and stabilization using traditional techniques.
The development of the craniofacial skeleton during the later childhood years into the mixed dentition period also yields further insight. During this time, the lower two thirds of the face become more prominent as a result of the forward and downward growth of the face thus exposing these bones to more injuries. This stage of development also is characterized by the development of the permanent tooth buds which occupy space in the maxilla and mandible ( Fig. 1 ). These unerupted teeth also create areas of structural weakness in the bone with a greater probability of sustaining a fracture through them. In addition, the eruption of the permanent teeth in conjunction with loose, exfoliating primary teeth make maxillomandibular wiring, and thus fracture reduction and stabilization, more difficult. The bone itself still has excellent, although decreasing osteogenic potential and elasticity during this time. The sinuses of the face also continue their development and their presence changes fracture patterns secondary to different areas of strength and weakness in the bone. As the permanent dentition becomes fully erupted at about 12 years of age, and growth continues through the early teenage years, the craniofacial skeleton becomes more adult like in its form and its surgical management .

Epidemiology
Children have a lower incidence of facial bone injury. For the most part they reside in a very protective social environment. In the early years of life, parental supervision and a child-friendly environment mitigate the likelihood of serious injury. Although falls during these years are common, their low center of gravity ensures that little harmful force is generated which might cause injury. As they reach the later childhood years, children become involved in activities such as school and play with other children. Participation in athletic activity later in life is also a cause of facial injury proximate to a developing neuromuscular coordination system and decreased situational awareness. Balls of all sorts, hockey pucks and sticks, lacrosse sticks, bats, elbows, knees, are very common in the cause of pediatric facial injuries during athletic events, especially when the appropriate protective equipment is not worn.
While there have been several excellent studies regarding the epidemiology of pediatric facial trauma, Posnick and colleagues provided the most significant recent description of this problem. In their review of 137 pediatric patients with facial fractures, the majority was male and the largest group of patients was found in the 6 to 12 years age range. The most common cause of trauma was motor vehicle-related, followed by falls, sports injuries, and interpersonal violent altercation. Mandibular fractures comprised 55% of the injuries, orbital fractures 30%, dentoalveolar fractures 23%, midface fractures 17%, nasal fractures 15%, zygomaticomaxillary complex fractures 14%, and cranial fractures 6%. Among the reported mandibular fractures, condyle fractures are the most common, followed by the symphyseal region, body, and, last, the angle of the mandible. However, from a rational standpoint, actual incidence may vary across geographic locations depending on many factors including the absence or presence of a level I pediatric trauma facility. In addition, many minor injuries such as nasal and dentoalveolar fractures are likely underreported as they can be commonly managed on an outpatient basis. There were no cervical spine injuries in this study.
Evaluation
The evaluation of the injured pediatric patient can be challenging. A thorough, systematic approach such as the advanced trauma life support protocols is valuable to insure that significant injury is not overlooked and to prioritize treatment. Standard questions in evaluating maxillofacial trauma regarding the presence of a malocclusion or inferior alveolar nerve dysfunction are not well understood by the pediatric age group and may lead to incorrect answers or no answers at all. The diagnosis of maxillofacial trauma is primarily made by clinical and radiographic examination. Practitioners must remember that any fracture in a child is generally an indicator of significant force as children tend to “bounce” and not “break.” The practitioner must have a high index of suspicion of associated injuries whenever a fracture is diagnosed.
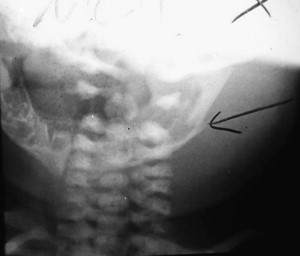
Radiographic exams are crucial to evaluate maxillofacial trauma in the pediatric patient. Most oral and maxillofacial offices are equipped with panoramic radiograph capability and, therefore, orthopantograms are commonly used to diagnose fractures of the mandible. However, in the hospital setting, there appears to be a trend to rely on CT imaging. Most emergency room facilities use the rapid CT scans to evaluate for central nervous system trauma. The scan can easily be carried through the maxillofacial region to diagnose facial fractures and give detailed three-dimensional information about fracture morphology and displacement. The CT scan is especially valuable when evaluating midface trauma. Additionally, the polytrauma patient or patient with questionable spinal injuries or long bone fractures cannot sit or stand for the traditional panoramic radiograph ( Fig. 2 ). The information obtained from the CT scan is more detailed and valuable than information obtained from the traditional panoramic films. Finally, the standard mandibular series of plain radiographs has very limited use when compared with the information gained from CT imaging ( Fig. 3 ).


Symphyseal and parasymphyseal mandibular fractures
Pediatric mandibular fractures require thoughtful consideration in management to avoid further injury to the developing dentition and significant growth disturbance. Most pediatric mandible fractures are amenable to closed reduction with MMF and the use of splints with skeletal fixation. With rapid healing and remodeling characteristic of the growing pediatric patient, even significant alterations of the occlusion and discrepancies in alignment are rapidly resolved. Indications for the use of rigid fixation are not common but do exist. Infants (less than 1 year of age) with mandibular fractures should be treated with observation. Diet modification is usually not necessary in this age group ( Fig. 4 ).
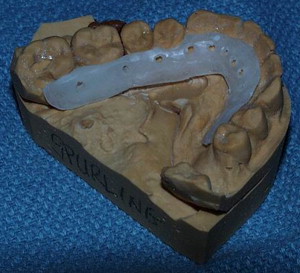
For anterior mandibular fractures, closed reduction is the preferred treatment plan. However, in fractures where proper alignment cannot be gained with MMF alone or condyle fractures require jaw function and physiotherapy, two alternative options exist. Construction of a lingual splint from dental models is an elegant but time-consuming technique for reduction and fixation. It requires taking dental impressions, a dental lab for fabrication, and yet another procedure to wire it on to the teeth ( Fig. 5 ). In addition, circumandibular wires are sometimes required to further secure the splint. This type of fixation allows for anatomic stabilization of the fracture and facilitates movement of the mandible, encouraging rehabilitation of condyle fractures if present. The second treatment alternative calls for placement of MMF and a transoral monocortical miniplate placed at the very inferior border of the mandible ( Fig. 6 ). This combination of internal fixation and arch wire or bar across the involved teeth allows adequate stability for postoperative function with guiding elastics for the closed management of condylar fractures. The importance of placing the plate at the very inferior aspect of the mandible is emphasized. In the young child, the risk of screw placement in the developing dentition is high unless this principle is followed ( Fig. 7 ).