The purpose of this article is to describe a dynamic approach for 3-dimensional analyses of facial soft-tissue movements. The method and analysis have numerous applications but, most specifically, are used to assess diagnostic and treatment outcomes of soft-tissue surgery in patients with repaired cleft lip and palate.
The recent focus on smile analysis in orthodontics has heightened the specialty’s desire for dynamic measures to assess facial soft-tissue movements. Currently, the technology exists to record 3-dimensional static facial images, and soon, clinicians will be able to automatically record and quantify animated faces during expressive behaviors in 3 dimensions and add that all-important fourth dimension of time. As part of past and current National Institute of Dental and Craniofacial Research funding (DE013814, DE016964, and DE019742), our research group has developed an approach to objectively quantify 3-dimensional facial movements and measure impairments in facial animations. The animations are mathematically generated based on the patient’s mean movements and are compared with mean, normal noncleft movements. In addition, these mean objective facial movements are independent of the patient’s actual face, where scarring of the upper lip can confound a viewer’s (subjective) assessment of facial movement. A clinician can use the comparative movements to objectively determine the degree of impairment in circumoral movements and the changes with age. This information supplements the clinician’s subjective evaluation of the patient. For the most part, we have used this approach on patients with facial disabilities such as congenital malformations (eg, cleft lip) and dentofacial deformities, but it is applicable to patients with other neuromuscular and acquired facial disorders (eg, facial trauma).
The importance of the approach lies in the fact that facial expressions are an important form of nonverbal communication that influences our interactions with others. Any disorder that impairs facial soft-tissue movements distorts and produces unesthetic animated behaviors that affect nonverbal communications. For example, early in life, there are indications that, because of the facial disability in babies born with a cleft lip and palate, the quality of mother-infant interactions is affected, and parents of these patients report various psychological problems in their children because of their facial appearance. The good news is that for the vast majority of orthodontic patients, a dynamic quantification of facial movements might be excessive. However, for patients with these more severe facial disabilities (eg, cleft lip and palate), this technology and analysis will have a positive impact on the clinician’s diagnosis of facial soft-tissue impairment, surgical treatment planning, and assessment of surgical outcomes.
When a child is born with cleft lip and palate ( Fig 1 , A ), the cleft lip is surgically repaired soon after birth ( Fig 1 , B ). Depending on the esthetic outcome of this initial or primary repair, the surgeon might recommend additional lip (revision) surgery later in life ( Fig 1 , C ). The decision for additional lip surgery is heavily influenced by the patient and the parents, and is based mainly on a subjective evaluation of the lips and nose; the dynamic functional capacity of the nasolabial region often is not considered. Studies have shown that subjective assessments are somewhat unreliable. The use of a popular subjective scale, the Asher-McDade ordinal scale, demonstrates that, at best, there is moderate reliability among surgeons. Our own research using subjective scales demonstrated that surgeons tend to agree with themselves when making the decision for additional lip surgery, but they tend to disagree with each other on this same decision.

The method presented in this article is not based on a subjective scale but on an objective measure. The more important issue with this measure is whether surgeons can use the diagnostic information obtained to modify and tailor their surgeries to meet a patient’s individual needs. Thus, it is recommended that, when formulating treatment plans for, and assessing the outcomes of facial soft-tissue surgery, a true quantification of facial movements should be used to complement the clinician’s subjective assessments. A further important benefit is that the diagnostic findings—the mean animation comparisons—can be viewed by the parents or the patient during the normal consent process to highlight the impairments before surgery as well as the outcomes after the surgery.
Material and methods
This approach consists of data acquisition instruments and statistical analyses.
Data acquisition instrument
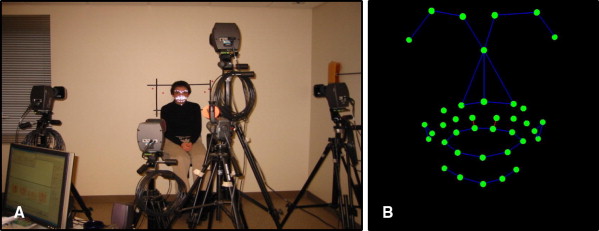
Facial movement data are acquired by using a motion analysis system (Motion Analysis; Motion Analysis Corporation, Santa Rosa, Calif). The system tracks retro-reflective markers only secured to specific landmarks on a patient’s face. Patients are asked to perform a sequence of repeated (5 times) maximum facial animations ( Fig 2 ): smile, lip purse, cheek puff, mouth opening, and grimace. A natural smile also is performed and repeated twice. During each animation, as many as 38 facial hemispherical landmarks (3 mm in size) are tracked in 3 dimensions at a rate of 60 Hz for 4 to 5 seconds.