External fixation of mandible fractures is a useful technique when an open treatment is contraindicated because of extensive comminution, bone or soft tissue loss, and infection. This technique can also be used temporarily until definitive treatment is delivered. A uniphasic or biphasic system can be placed to reduce and stabilize mandibular fractures. These systems use surgically placed threaded pins and different types of connectors that can be manipulated to optimize the reduction of fractures. External fixation remains a quick, safe, and simple method to treat mandible fractures in selected clinical situations, and it should be part of the armamentarium in surgeons treating these injuries and fractures.
External fixation of mandible fractures is a technique in which segments are manipulated in place by pins and then fixated with some type of connectors. It is often considered a subtype of closed reduction and provides semirigid fixation to the fractured mandibular segments. Historically, the first example of splinted pins being applied to long bones was reported as early as 1853 by Malgaigne and by Rigaud in 1870. The first external fixator applied to the mandible was attributed to Ginestet in 1936. Clouster and Walker described modifying a Roger Anderson orthopedic appliance to treat comminuted mandible fractures during World War II. The first biphasic fixation device was introduced by Morris in 1949, which was a variant of older fixators intended as a temporary mean of fixation until acrylic was applied and cured to link the pins. Suddenly, external fixation became the most popular method to treat many types of facial fractures in the 1950s and 1960s until the advent of rigid internal fixation. Since then, the use of external fixators has significantly decreased but remains a useful technique in selected types of fractures, as reviewed in this article.
Indications for external pin fixators
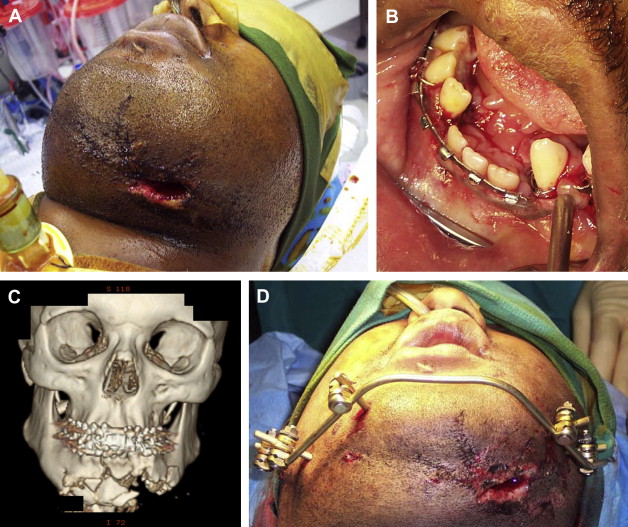
In nonatrophic mandibles, most of the blood flow is supplied from the inferior alveolar vessels. By disturbing this central flow, mandible fractures subsequently rely on the periosteum and soft tissue envelope during the healing phase. In situations in which comminution is combined with a large amount of periosteal, muscle, or mucosal damage, an increased incidence of nonunion and infections can be expected. It is based on these biologic principles that most indications for external fixation have been developed, especially when maxillomandibular fixation is not adequate because of missing teeth on either side of the fracture or is contraindicated for concomitant medical reasons. Placing these devices does not require extensive periosteal reflection as compared with open reductions, thus preserving vascularity of bone fragments. Situations like extensive fracture comminution and severe tissue loss, such as that occurring in gunshot wounds, are well-accepted indications for external fixation. In theory, by treating these fractures in a closed fashion, the viability of the fragments is maintained without disrupting their blood supply ( Fig. 1 ). These comminuted fractures then consolidate for 8 to 10 weeks before secondary surgery, if considered. At that time, the fractures are debrided or reconstructed. During the initial stabilization period of 8 to 10 weeks, the soft tissue is also allowed to be restored, optimizing future potential operations.
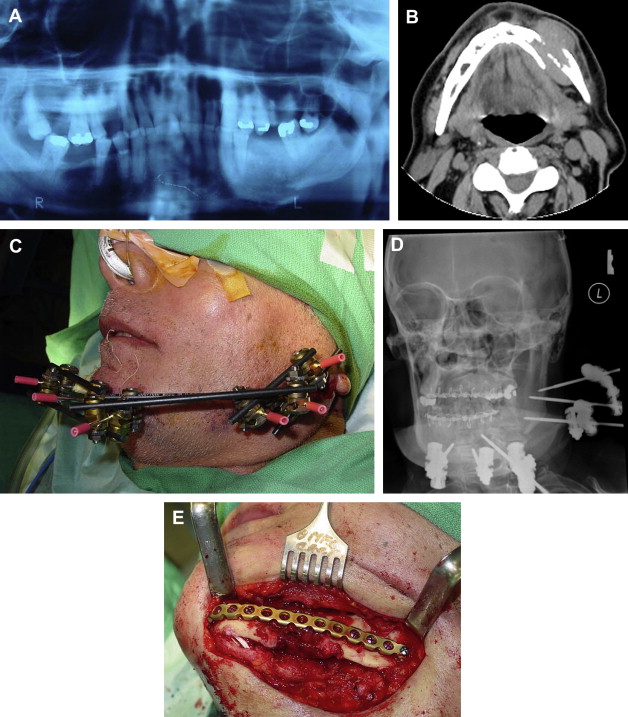
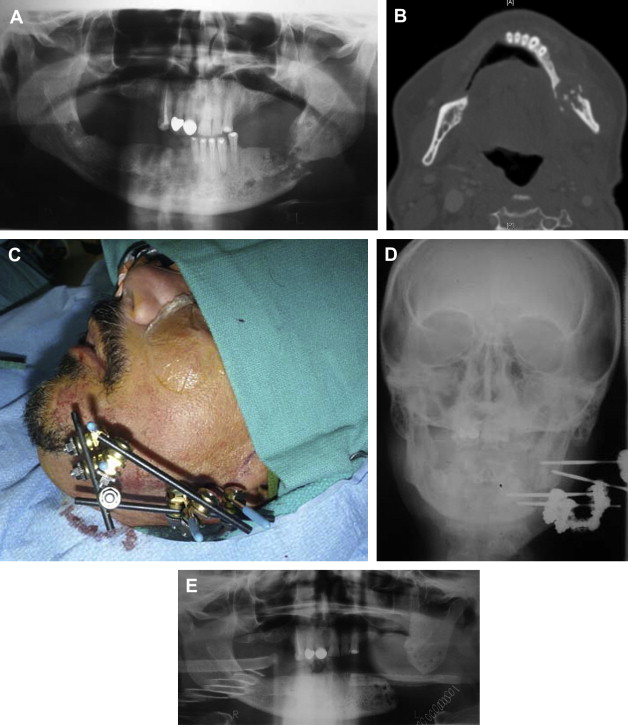
The technique of external pin fixation may also be considered when there is a large amount of bone loss in such conditions as pathologic fractures occurring through tumors, cysts, or severely atrophic mandibles. In these clinical scenarios, there may be not enough bone to adapt plates and screws reliably. Examples of pathologic fractures involving metastatic tumors, such as multiple myeloma of the mandible, are also amenable to temporary treatment with external fixation until completion of radiotherapy and subsequent reconstruction, as illustrated in Fig. 2 . Severe osteoradionecrosis of the mandible with fracture of the inferior border may also be provisionally managed with an external fixator until the conclusion of hyperbaric oxygen therapy and before definitive reconstructive procedures ( Fig. 3 ).
Grossly infected fractures with significant soft tissue edema, cellulites, and osteomyelitis are also amenable to external fixation, thus avoiding large extraoral incisions and potentially difficult neck dissections ( Fig. 4 ). This technique is often used as a temporary or final treatment, especially when teeth are absent proximally or when maxillomandibular fixation is inadequate. Once the infection is under control after a short period of external fixation, the fracture may be debrided and rigidly reconstructed. In addition, because the application of external fixators is rather simple and requires minimal operating time, it is sometimes used in patients with compromised health or in critically injured patients as a temporary means of fixation.





