This article is a review that enumerates the causes of impaction of the maxillary permanent canines, including hard tissue obstructions, soft tissue lesions, and anomalies of neighboring teeth, and discusses the much-argued relationship between environmental and genetic factors. These phenomena have been shown in many investigations to accompany the diagnosis of canine impaction and have been presented as unrelated anomalous features, each of which is etiologically construed as genetic, including the aberrant canine itself. While in general the influence of genetics pervades the wider picture, a guidance theory proposes an alternative etiologic line of reasoning and interpretation of these studies, in which the same genetically determined anomalous features provide an abnormal milieu in which the canine is reared and from which it is guided in its misdirected and often abortive path of eruption.
Highlights
- •
Guidance of the canine during normal eruption alters incisor axial orientation.
- •
Canine eruption direction and progress are influenced by environmental factors.
- •
Right and left variations in a patient cannot show different genetic features.


With the exception of the third molars, impaction of the maxillary permanent canines is the most common form of tooth impaction. Relatively recent studies into the frequency with which maxillary canine impaction occurs in the general population have indicated a prevalence from 0.27% in a Japanese population to as much as 2.4% among Italians, with the condition affecting female patients 2.3 to 3 times more frequently than males.
Notwithstanding the opinions of some respected researchers in favor of an exclusively genetic etiology for its occurrence, there are many and varied reasons for impaction of the maxillary canines. The causes can be classified into 4 distinct groupings: local hard tissue obstruction, local pathology, departure from or disturbance of the normal development of the incisors, and hereditary or genetic factors.
Local obstruction
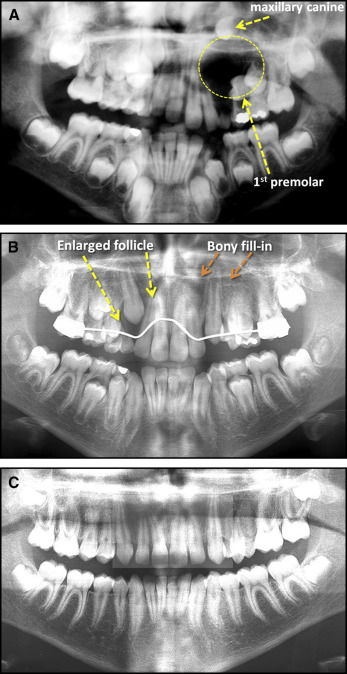
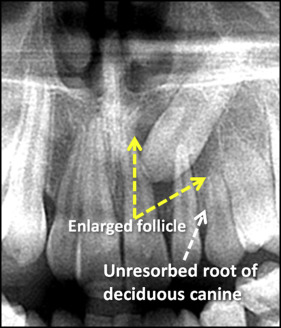
Clinical and radiographic assessment of a number of impacted canine cases led Lappin to observe that the deciduous canines were frequently overretained, often with a long and unresorbed root ( Fig 1 ). He speculated that the nonresorption of the deciduous canine was the cause of the anomaly. However, this was not a controlled study; he drew the conclusions solely from what he had observed. Although the mechanism for root resorption of a deciduous tooth is unknown, it is recognized that it occurs when the dental follicle is near an unerupted permanent tooth. Thus, it is equally plausible to argue the reverse: that resorption has not occurred because of the distance of the permanent tooth; therefore, the unresorbed root of the deciduous canine is not the cause of the displacement, but rather its result.
On the other hand, Lappin’s speculation might be justified, since several studies have shown that prophylactic extraction of the deciduous canines when there is the potential for maxillary permanent canine impaction appears to encourage spontaneous eruption of a majority of displaced permanent canines.
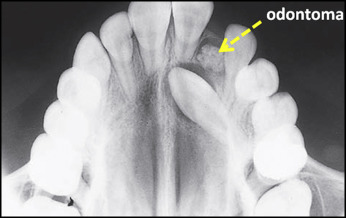
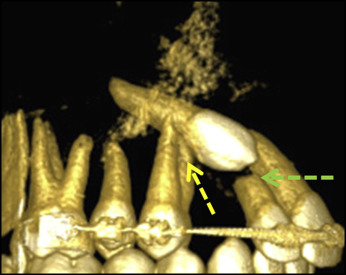
From parallel work relating to impacted incisors, we know that hard tissue pathology in the immediate area can cause displacement of a developing tooth. The first entities that come to mind are the supernumerary tooth and the odontoma. These diagnoses are highly definitive, and they present an etiologic role that is easily understood. Although this is a potent cause of impaction and is frequently seen in relation to impacted central incisors, supernumerary teeth and odontomata in the canine area are relatively rare ( Fig 2 ).
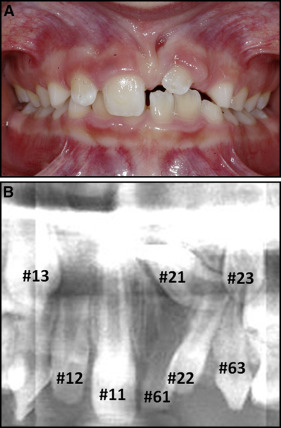
Perhaps a little more surprising was the finding in a recent study that in unilateral cases of central incisor impaction, whether because of obstruction by a supernumerary tooth or an odontoma or because of dilaceration or recent trauma, there is a high frequency of eruption disturbance of the canine on the same side. This investigation showed a significant increase in the prevalence and severity of displaced canines (41.3%): buccal displacement was seen in 30.2%, palatal displacement occurred in 9.5%, and canine-lateral incisor transposition in 1.6% of the patients. Half of the buccally displaced canines on the ipsilateral side were pseudotransposed with the adjacent lateral incisor. These figures compared with a total of 4.7% on the contralateral side.
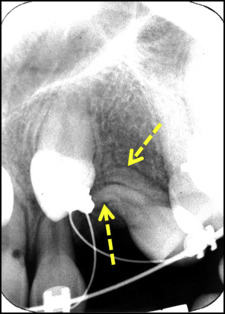
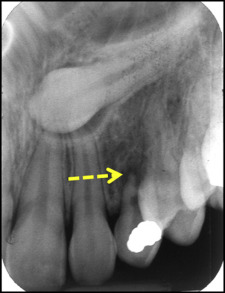
These abnormal features may be explained by the fact that the lateral incisor tips mesially and encroaches on the space of the unerupted central incisor to a considerable degree ( Fig 3 , A ). The corollary of this is that the root apex tips distally and into a position where it interferes with the eruption path of the unerupted canine.
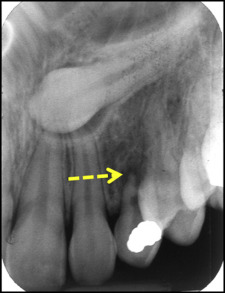
In the immediate neighborhood of the canine, the sequence of eruption of teeth dictates that the maxillary lateral incisor and the first premolar precede the canine by 3 years and 1 year, respectively. As long as the canine is in its normal eruptive position (ie, slightly buccal to the line of the dental arch) and has adequate space, its path of eruption will permit it to erupt unhindered. However, if the premolar has erupted with a mesiobuccal rotation, then its palatal root will be rotated directly into the path of the canine ( Fig 4 ). In this way, the abnormal orientation or abnormal root form of the adjacent first premolar ( Fig 5 ) can be the impediment that causes the impaction of the maxillary permanent canine, despite its normal development and location.
Local pathology
Overretained deciduous canines are commonly nonvital by the age of 12 years because of caries, trauma, or extreme attrition. The resulting chronic periapical granuloma, by itself, is a soft tissue inflammatory lesion that will have a potent effect on deflecting or arresting the eruption of the permanent canine ( Fig 6 ). Extraction of a diseased deciduous canine usually and concurrently eliminates the granuloma, which is the displacing factor for the permanent tooth.
Investigations into the efficacy of prophylactic extractions of deciduous canines have been referred to above. Those articles do not mention whether patients with nonvital deciduous canines were included in the study samples. One may be permitted to question just how many deciduous canines in these study samples were nonvital. A high percentage of the permanent canines had later erupted spontaneously in what was claimed to be the apparent sequel to the extraction of the deciduous predecessor. There are grounds to argue that their successful eruption can also be attributable to the concurrent elimination of a periapical lesion.
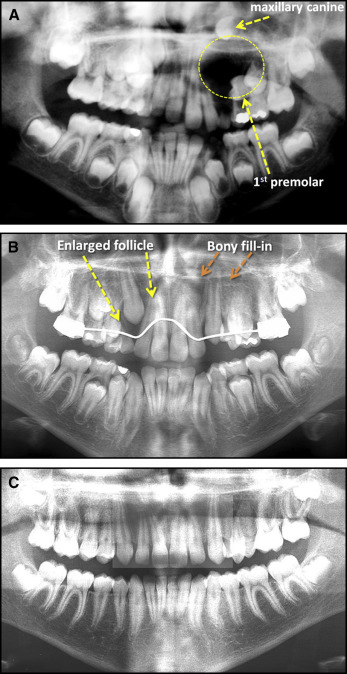
In rare instances, a granuloma develops into a radicular cyst by adversely stimulating the rests of Malassez in the area, and this expanding, space-occupying, fluid-filled, turgid, and epithelium-lined balloon will displace adjacent unerupted teeth. It is more likely, however, that a long-standing granuloma at the apex of a deciduous canine may induce cystic change in the follicular sac of the adjacent unerupted permanent canine, which begins as a benign enlargement of the sac surrounding the permanent canine and increases to become a dentigerous cyst. The hydrostatic pressure in the cyst overcomes the innate force of eruption of the tooth, arresting its downward progress and even causing the tooth to “back up” in more advanced cases. The cyst may continue to enlarge by initiating pressure resorption of the adjacent bone, until the cyst lining comes into contact with the roots of adjacent teeth, which will be displaced into an adjacent area of potentially resorbable bone.
One method of treatment of a dentigerous cyst involves opening it to the exterior—marsupialization—allowing for drainage and effectively defusing the displacing factor. The area previously occupied by the cyst remains lined with cystic/follicular epithelium. When the increased hydrostatic pressure is released, bone begins again to fill in behind this epithelial lining, which undergoes metaplasia as its healing cut edges become contiguous with the oral epithelium. The residual cyst cavity slowly shrinks, and teeth that had previously been located in the cyst wall begin to migrate with the returning bone toward more accessible positions. In this way, prophylactic extraction of a deciduous canine to resolve potential palatal canine impaction may be successful in producing spontaneous eruption, as the result of the simultaneous and inadvertent rupture and evacuation of an associated and enlarged follicular sac or early dentigerous cyst ( Fig 7 ). This has also been beautifully illustrated in several case reports.
Trauma to the face can cause laceration of the soft tissues of the lips and cheek, and its force may be transmitted to the maxilla to cause displacement of the unerupted canine or dilaceration of its developing root, particularly in younger children. Pursuant to incidents of this kind, the tooth may become impacted.
It is clear that local anatomic obstructions and hard and soft tissue pathologic entities can cause deflection in the normal eruption path of the canine. When these etiologic factors are eliminated, there is a degree of autonomous correction in the eruption path that may lead to spontaneous eruption of the canine.
Local pathology
Overretained deciduous canines are commonly nonvital by the age of 12 years because of caries, trauma, or extreme attrition. The resulting chronic periapical granuloma, by itself, is a soft tissue inflammatory lesion that will have a potent effect on deflecting or arresting the eruption of the permanent canine ( Fig 6 ). Extraction of a diseased deciduous canine usually and concurrently eliminates the granuloma, which is the displacing factor for the permanent tooth.
Investigations into the efficacy of prophylactic extractions of deciduous canines have been referred to above. Those articles do not mention whether patients with nonvital deciduous canines were included in the study samples. One may be permitted to question just how many deciduous canines in these study samples were nonvital. A high percentage of the permanent canines had later erupted spontaneously in what was claimed to be the apparent sequel to the extraction of the deciduous predecessor. There are grounds to argue that their successful eruption can also be attributable to the concurrent elimination of a periapical lesion.
In rare instances, a granuloma develops into a radicular cyst by adversely stimulating the rests of Malassez in the area, and this expanding, space-occupying, fluid-filled, turgid, and epithelium-lined balloon will displace adjacent unerupted teeth. It is more likely, however, that a long-standing granuloma at the apex of a deciduous canine may induce cystic change in the follicular sac of the adjacent unerupted permanent canine, which begins as a benign enlargement of the sac surrounding the permanent canine and increases to become a dentigerous cyst. The hydrostatic pressure in the cyst overcomes the innate force of eruption of the tooth, arresting its downward progress and even causing the tooth to “back up” in more advanced cases. The cyst may continue to enlarge by initiating pressure resorption of the adjacent bone, until the cyst lining comes into contact with the roots of adjacent teeth, which will be displaced into an adjacent area of potentially resorbable bone.
One method of treatment of a dentigerous cyst involves opening it to the exterior—marsupialization—allowing for drainage and effectively defusing the displacing factor. The area previously occupied by the cyst remains lined with cystic/follicular epithelium. When the increased hydrostatic pressure is released, bone begins again to fill in behind this epithelial lining, which undergoes metaplasia as its healing cut edges become contiguous with the oral epithelium. The residual cyst cavity slowly shrinks, and teeth that had previously been located in the cyst wall begin to migrate with the returning bone toward more accessible positions. In this way, prophylactic extraction of a deciduous canine to resolve potential palatal canine impaction may be successful in producing spontaneous eruption, as the result of the simultaneous and inadvertent rupture and evacuation of an associated and enlarged follicular sac or early dentigerous cyst ( Fig 7 ). This has also been beautifully illustrated in several case reports.