Endoscopic-assisted open reduction/internal fixation of mandibular condylar fractures is a viable alternative to traditional closed or open reduction techniques. However, case selection is important. Ideally, the fracture undergoing EAORIF should be easily manipulated into reduction and have enough stable bone on either side of the fracture to support a bone plate. It is important to note that in all reprinted studies, authors note a steep “learning curve” with the EAORIF technique. Identical procedures took the novice surgeon two to three times as long when compared with an experienced surgeon. EAORIF is a technique that should be included in the armamentarium of the maxillofacial trauma surgeon when treating mandibular condylar fractures.
The mandibular condyle is a unique area of the facial skeleton. It is an integral part of the temporomandibular joint (TMJ)—a ginglymoarthrodial joint (rotation/translation joint) found bilaterally in the face . Fractures of the mandibular condylar apparatus are common and account for about 25% to 30% of all mandibular fractures. Complications of fractures of this area include malocclusion, such as apertognathia, loss of posterior mandibular vertical height resulting in a facial asymmetry, loss of chin projection in the sagittal plane, and loss of function/mobility of the TMJ. Management of fractures of the mandibular condyle and subcondyle has historically been debated in the maxillofacial surgical literature. Many advocate simple closed reduction of these fractures, whereas others feel that open reduction is the appropriate treatment modality. Closed reduction, while minimally invasive, may not adequately reduce the fracture, resulting in long-term TMJ dysfunction or mobility issues. In general terms, fractures of this area of the jaw can be classified into fractures of
- •
Condylar head (intracapsular)
- •
Condylar neck
- •
Subcondylar/high ramus fractures
- 1.
Medially displaced (medial over-ride)
- 2.
Laterally displaced (lateral over-ride)
- 1.
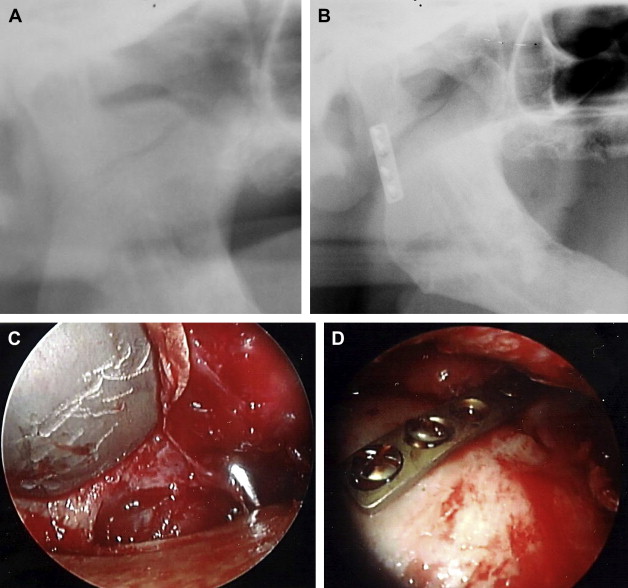
There is a general consensus that isolated fractures of the condylar head (intracapsular) are best treated via a closed approach, including soft diet or maxillo-mandibular fixation for 2 to 3 weeks followed by intensive physical therapy. Subcondylar and condylar neck fractures may be amenable to rigid fixation; however, traditional open reduction has certain risks, including facial nerve injury and preauricular scarring. Advantages of open reduction include immediate function, restoration of facial symmetry, and improved jaw motion ( Fig. 1 A–D).
Minimally invasive endoscopy was originally developed by general surgeons and gynecologists and has evolved over the past decade. It was a technique initially well suited for the abdomen, as this area of the body creates an anatomic “optical cavity” for visualization with an endoscope. Advantages of endoscopic surgery are based on its ability to provide excellent visualization of the surgical field via a small incision and include acceptable minimal scarring and decreased tissue manipulation and dissection, resulting in decreased postoperative morbidity and faster recovery with shorter hospital stay and quicker return to normal function.
The facial skeleton anatomically is not as well suited for endoscopy because the optical cavities created are significantly smaller than those of the abdomen. Smaller endoscopy instruments have been developed, allowing for use in facial skeletal surgery. A small optical cavity is created in the lateral aspect of the ramus allowing for endoscopic reduction of subcondylar fractures. By using an endoscopic technique, the advantages of open reduction are met, while minimizing the risk of facial nerve injury.
Indications for endoscopically assisted open reduction and internal fixation (EAORIF) of mandibular condylar fractures include
- •
fractures limited to the subcondyle or condylar neck in which there is enough bone stock to stabilize a bone plate
- •
malocclusion and/or decreased range of motion (edentulous patients with subcondylar fractures can be treated endoscopically; however, splints or dentures to stabilize the maxilla and mandible should be used)
- •
loss of chin projection or facial asymmetry
Contraindications to the endoscopic approach include
- •
comminuted condylar fractures or intracapsular fractures
- •
medially displaced condylar fractures that cannot be reduced
- •
condylar fractures older than 2 weeks on which fibrous union has started to develop
- •
medically compromised patients who are not healthy enough to undergo general anesthesia required for surgical procedures
There are two surgical approaches used in EAORIF of the condyle: an intraoral approach and a submandibular approach. Advantages of the intraoral approach include the lack of a skin incision, whereas its disadvantage is a smaller optical cavity to work within. The submandibular approach requires a 1.5-cm skin incision at the angle of the mandible, similar to a Risdon incision, placing the facial nerve at minimal risk; however, the optical cavity created has a larger working space with better endoscopic orientation.
Instrumentation for this technique includes
- •
endoscopic equipment: monitor, endoscope with irrigation sheath (usually 2.7 to 4.0 mm in diameter with 30-degree or 45-degree angles)
- •
subcondylar/ramus fixation set (Synthes Maxillofacial, Paoli, PA)
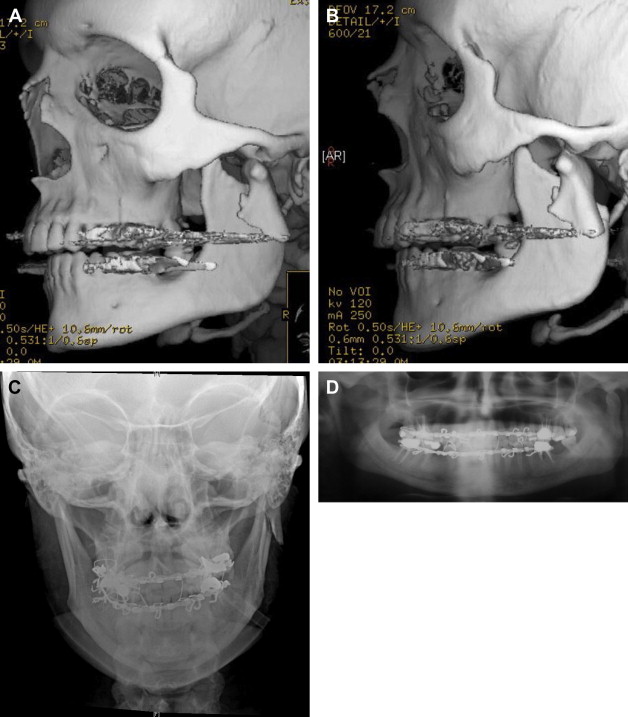
In either surgical approach, placing the patient into maxillo-mandibular fixation is necessary, typically using Erich arch bars. At this point, the optical cavity is created via an intraoral or extraoral approach as previously discussed. Once down to the lateral ramus, a periosteal elevator exposes the mandible in the subperiosteal plane from subcondyle to angle, creating the optical cavity. Once the optical cavity is created, the endoscope is placed and the fracture is visualized. Manual reduction of the fracture is then completed via manipulating the teeth or distracting the mandible in the angle region. Once reduced, a six-hole 2.0-mm noncompression miniplate is inserted using a right-angle screwdriver/drill or a trocar. Angled elevators and reduction-manipulation forceps in the Synthes fixation set facilitate reduction and fixation of these fractures. Once reduced, the patient is allowed to function—typically placed into guiding elastics for 1 to 2 weeks ( Fig. 2 A–D).