Introduction
Our objective was too assess the effectiveness of 3 analgesics (ibuprofen, naproxen sodium, and acetaminophen) and a placebo administered before and after the placement of separators in reducing the severity of postseparator placement pain. We also examined the impact of treatment on chewing efficiency at 24 hours after separator placement.
Methods
Twenty-four subjects participated in the study. Each subject received 3 of 4 treatments: ibuprofen, naproxen sodium, acetaminophen, or placebo in random order at monthly intervals. The dosing times were 1 hour before separator placement and 3 and 7 hours after separator placement. Before placement, the subjects completed a masticatory efficiency test and a visual analog scale (VAS) for expected pain and pain experienced. A VAS pain diary was kept for 24 hours. Subjects returned to the clinic after 1 week for separator removal.
Results
VAS pain summary scores after separator placement were significantly affected by the administration of ibuprofen ( P = 0.0298) and the time after separator placement ( P <0.0001). Administering ibuprofen before and after separator placement significantly reduced pain compared with the placebo. The analgesic effects diminished by day 2, resulting in peak pain levels and decreased chewing efficiency. The expected pain after separator placement also played a role in experienced pain; subjects expecting more pain experienced more pain.
Conclusions
Ibuprofen was superior to the placebo in relieving postseparator pain as measured by the VAS pain summary scores, whereas acetaminophen and naproxen sodium did not significantly differ from the placebo.
Pain is a widespread concern in dentistry, including the specialty of orthodontics. Between 90% and 95% of patients undergoing orthodontic treatment report pain with appliances. A survey of patients’ attitudes toward orthodontic treatment indicated that pain is the most discouraging aspect of treatment and the primary reason for wanting to discontinue care.
Pain after orthodontic treatment is usually felt within a few hours, reaching maximum levels 24 hours after treatment. After 1 week, the level of discomfort usually decreases. There is evidence that about 25% to 45% of patients still experience pain after 7 days of appliances. Differences in treatment, whether separators, appliances, or archwires, might explain the conflicting results among studies. With such a high incidence of discomfort, pain control and management are an obvious interest for clinicians and patients alike.
Nonsteroidal anti-inflammatory drugs (NSAIDs) include ibuprofen and naproxen sodium and are often used for their analgesic, anti-inflammatory, and antipyretic effects. Because of the gastrointestinal side effects associated with NSAIDs, acetaminophen might be recommended. Acetaminophen is classified as a nonopiod analgesic with analgesic and antipyretic properties. Acetaminophen does not have the anti-inflammatory component that is characteristic of NSAIDs.
Ngan et al were the first to evaluate analgesics to control discomfort associated with orthodontic treatment. They administered 400 mg of ibuprofen or 650 mg of aspirin immediately after separator or initial archwire placement. Steen Law et al took this a step further and instructed patients to also take a dose of 400 mg of ibuprofen 1 hour before separator placement. Both studies found pain reduction with ibuprofen. Minor et al also supported the administration of ibuprofen before and after separator placement to decrease the pain experienced at 6 hours, bedtime, and the morning after separator placement. Polat and Karaman studied several analgesics. They found that naproxen sodium and aspirin administered before and after separator placement more effectively reduced pain compared with ibuprofen, flurbiprofen, and a placebo. More recently, Bird et al found no significant differences in pain over a 24-hour period after a single dose of acetaminophen or ibuprofen administered 1 hour before separator placement.
Based on the literature, it is apparent that there is no accepted regimen for treating orthodontic pain. The objective of this prospective, randomized, double-blind, placebo-controlled crossover clinical trial was to compare the effectiveness of 3 analgesic drugs (ibuprofen, naproxen sodium, and acetaminophen) administered to reduce the incidence and severity of pain after the placement of separators. We also evaluated the effect of treatment assignment on chewing efficiency at 24 hours after separator placement.
Material and methods
Twenty-four subjects participated in this study at the University of Florida Orthodontic Clinic. Each participant met these inclusion criteria: (1) between 18 and 30 years of age; (2) not pregnant; (3) second premolars, first molars, and second molars in contact, allowing the placement of 2 separators in each of the 4 quadrants; (4) not taking pain medications; (5) no contraindications to the drugs under study or almonds, (6) no need for antibiotic prophylaxis before dental treatment; and (7) informed consent for participation in the study. The study was approved by the University of Florida Institutional Review Board for the Protection of Human Subjects.
Each subject was randomized to receive 3 of 4 treatments (ibuprofen, naproxen sodium, acetaminophen, or placebo) over 3 months. The dose and timing for each treatment varied slightly because they were based on over-the-counter directions for each medication. The dosing times for each treatment were 1 hour (D1) before separator placement, and 3 (D2) and 7 (D3) hours after separator placement. The separators were removed after 1 week. One and 2 months from the start of participation, the subjects returned to the clinic and received a second treatment. By the end of the 3 months (periods), each subject had received 3 of the 4 treatments.
The dosing amounts for each drug were 400 mg of ibuprofen at D1, D2, and D3; 500 mg of naproxen sodium at D1, placebo at D2, and 250 mg of naproxen sodium at D3; 650 mg of acetaminophen at D1, D2, and D3; and placebo at D1, D2, and D3. The Investigational Drug Service at Shands Hospital, Gainesville, Fla, encapsulated and dispensed the tablets; consequently, the researchers were blinded to the treatment group assignment.
Before the first dosing (T0), the following measurements were completed by all subjects.
- 1.
Expectation of pain after separator placement using a 100-mm visual analog scale (VAS) with anchors of “no pain” and “worst pain imaginable.”
- 2.
Modified mastication performance index, for which the subjects chewed 1 bagged almond 5 times on the right side of the mouth without swallowing. This was repeated on the left side of the mouth with another bagged almond. VAS pain ratings as a consequence of chewing the almond were recorded.
Two separators (P/N 640-0080, Ormco, Glendora, Calif) were placed in each quadrant, mesially and distally to the first molar. The method of placement was under the contact for all subjects. Pain at separator placement was recorded with the VAS. Over the next 24 hours, the subjects recorded discomfort when biting, chewing, fitting front teeth together, and fitting back teeth together in a VAS pain diary, similar to that used in other studies. VAS assessments were recorded at 2 hours after separator placement (T1), 6 hours after separator placement (T2), bedtime (T3), upon awakening (T4), and 24 hours after separator placement (T5). The remaining 2 doses were self-administered by the subject at D2 and D3. At T5, the subject completed the masticatory efficiency test with the VAS. The completed pain diary and the chewed bagged almonds were brought to the next appointment.
To analyze the chewed almonds, the whole sample was weighed and sieved through a #10 mesh, and the separated sample was weighed. The chewing efficiency was the percentage of the original sample that passed through the sieve.
Statistical analysis
Descriptive statistics were calculated for pain scores and masticatory chewing efficiency at each time point for each treatment group. Linear mixed models were used to examine VAS pain scores over time and chewing efficiency. The initial model for the VAS pain summary score (sum of pain ratings for biting, right and left; chewing, right and left; fitting back teeth together; and fitting front teeth together) included the following variables: treatment, period (month 1, 2, or 3), prior treatment (to assess carryover effects), order, time point, and treatment by time-point interaction. The interaction allowed the pain response pattern to vary over time depending on the treatment group. This model was used to evaluate differences in treatment effects at specific time points. A reduced model was examined, excluding period, prior treatment, or treatment by time-point interaction, if they did not achieve statistical significance in the initial model. The initial model for 24-hour chewing efficiency included treatment, baseline chewing efficiency, period, and prior treatment. For significant main effects, contrasts were used to identify the specific groups that differred. For both outcomes, the impact of adding additional covariates (expected pain and sex) to the initial model was also examined. For all analyses, a P value less than 0.05 was considered statistically significant. SAS software (version 9.1, SAS Institute, Cary, NC) was used for the statistical analyses.
Results
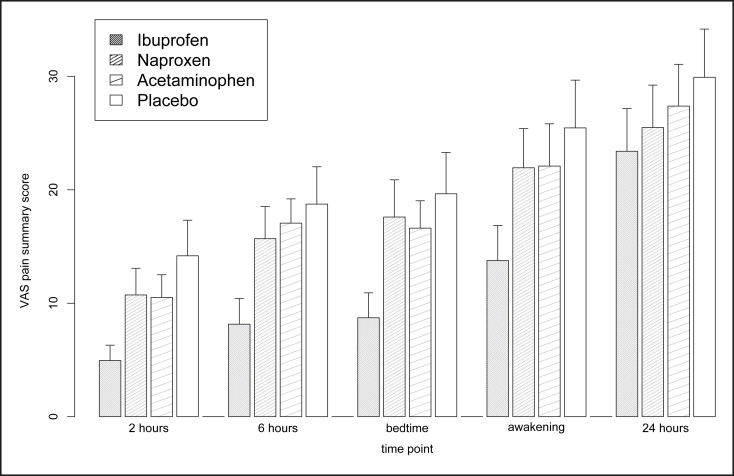
The sample consisted of 11 women (46%) and 13 men (54%); 75% were white, 13% Asian, 8% other, and 4% Hispanic. Their ages ranged from 19 to 30 years, with a mean age of 26.4 years (SD, 2.5). Mean VAS pain summary scores by treatment groups and time points are displayed in the Figure . Our initial mixed model did not indicate significant effects due to period ( P = 0.85), prior treatment ( P = 0.84), order ( P = 0.91), or time point by treatment interaction ( P = 0.68). The reduced model detected significant effects from treatment assignment ( P = 0.0298) and time point ( P <0.0001). Parameter estimates for this model are listed in Table I . Contrasts were used to identify treatments that differed: ibuprofen vs placebo ( P = 0.0034), and a borderline difference was seen between naproxen and the placebo ( P = 0.0563). Contrasts also indicated that all time periods differed from each other ( P <0.0001) except for the T2 and T3 time points ( P = 0.41).
| Parameter | Estimate (SE) | P value |
|---|---|---|
| Intercept | 30.70 (2.70) | <0.0001 |
| Treatment | ||
| Ibuprofen | −7.89 (2.59) | 0.0035 |
| Naproxen sodium | −5.04 (2.50) | 0.0563 |
| Acetaminophen | −3.67 (2.50) | 0.1614 |
| Placebo | (reference) | |
| Time point | ||
| 2 hours | −16,46 (1.42) | <0.0001 |
| 6 hours | −11.64 (1.32) | <0.0001 |
| Bedtime | −10.90 (1.16) | <0.0001 |
| Awakening | − 5.74 (0.89) | <0.0001 |
| 24 hours | (reference) |
The initial model for the VAS pain summary score was evaluated to further identify treatment differences at specific time points. Subjects who took ibuprofen reported significantly less pain than those who took the placebo at 2 and 6 hours after separator placement, as well as at bedtime and awakening. Acetaminophen and naproxen sodium did not show significant differences compared with the placebo at any time point. By 24 hours postplacement, which was 17 hours after the last medication dose, pain levels returned to those of the placebo for all subjects ( P = 0.27).
We next examined the impact of additional covariates: sex and expected pain. No significant effect in the VAS pain summary score due to sex was found ( P = 0.37). However, expected pain had a significant effect on the VAS pain summary score, and its impact varied over time. The coefficient estimates for this model are presented in Table II . Considering both the impact of expected pain and the expected pain by time point interaction, we saw that expected pain had the greatest impact on later pain scores, at T4 and T5. By this time, pain medication would have worn off, and the pain that the subjects felt was consistent with their expectations. For example, from the model, with all other factors equal, we could compare the predicted VAS pain summary score for a subject with an expected pain rating of 1.0 with that of a subject with an expected pain rating of 7. The subject with the higher expected pain rating (7) would have predicted VAS pain summary scores 1.7 points higher at 2 hours and 13.6 points higher at 24 hours, than the subject with the expected pain rating of 1.



