Introduction
In this retrospective cohort study of the effectiveness of interceptive orthodontic treatment, we compared patients receiving interceptive orthodontic treatment with untreated control subjects.
Methods
Models were scored by using the index of complexity, outcome and need (ICON). Control models (n = 113) were archival and were selected based on malocclusion in the early mixed dentition and no orthodontic treatment during the subsequent 2 years. The patients (n = 133) were in the mixed dentition and consecutively treated in the University of Bergen orthodontic clinic. Initial ages were 9.4 years (± 1.4) for the treated group and 9.3 years (± 0.8) for the control group. The treatment took a mean of 27.2 months (± 16.3) for the patients; the control group was observed for a mean of 24.4 months (± 3.6). Subject Groups were matched for age, need, complexity, duration, and all ICON components except spacing ( P <0.006) and crossbite ( P <0.000).
Results
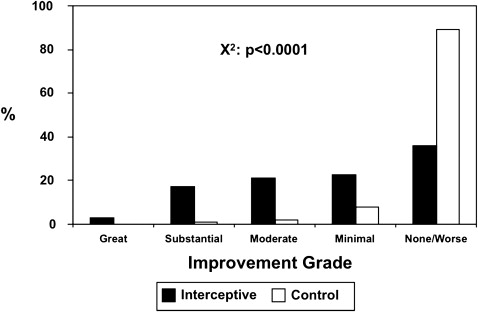
ICON scores decreased after treatment by 38.8% ( P <0.0001) from 54.9 (± 16.6) to 33.6 (± 16.1). The controls were unchanged, with ICON scores of 54.0 (± 14.8) and 54.2 (± 16.9). Improvement grades were different ( P <0.0001), with most controls categorized as “not improved or worse” (89.4%), whereas only 36.1% of the treated group were in that category. However, there were increases in the “minimal,” “moderate,” and “substantial” improvement categories for the treated subjects (22.6%, 21.1%, and 17.3%, respectively). The controls did not change in any ICON component and worsened in crowding ( P <0.007), whereas the patients improved in esthetics, crowding, crossbite, and overbite ( P <0.007).
Conclusions
These results indicate that interceptive orthodontic treatment is effective for improving malocclusion but does not produce finished-quality results.
Interceptive and preventive orthodontic procedures are relatively simple and inexpensive treatment approaches that target developing malocclusions during the mixed dentition. Orthodontists perceive these as useful ways to reduce the severity of malocclusions, improve a patient’s self-image, eliminate destructive habits, facilitate normal tooth eruption, and improve some growth patterns. Because of this, some have advocated their wider use as public health measures aimed at reducing the burden of malocclusion in underserved populations and as a strategy for increasing access to orthodontic treatment when resources are limited.
Available evidence suggests that patients at risk for severe malocclusion can readily be identified in the mixed dentition, and that the burden of these malocclusions in this age group is substantial (about 25%-30%). In 1 study, patients at risk for future orthodontic problems were identified in 28% of those examined, and most of the developing malocclusions were judged to be suitable for interceptive orthodontic treatment. A similar study found that about 27% of the children examined in a large Nigerian sample needed some form of interceptive orthodontic treatment. A third study of children screened in a community dental clinic at ages 9 and 11 years also found that one-third would benefit from interceptive orthodontic treatment.
Although interceptive orthodontic procedures often do not produce finished orthodontic results without a second phase of treatment in the permanent dentition, several studies have suggested that systematically planned interceptive treatment in the mixed dentition might contribute to a significant reduction in treatment need between the ages of 8 and 12 years, often producing results so that further need can be categorized as elective. In a Finnish study, the need was reduced significantly from ages 8 to 12 in a small group receiving interceptive treatment. In a similar study, 94% of the children receiving interceptive treatment in a community health clinic were judged to have completely successful results, with only 2% showing deterioration. Using the peer assessment rating (PAR) and the index of complexity, outcome and need (ICON), the authors of another study reported significant reductions in malocclusion severity after early treatment in both Medicaid and privately financed patients, with comparable results in both groups. In addition, about two thirds of those patients changed from a “medically necessary” category, as judged by the handicapping labiolingual deviation index to “elective” after mixed dentition orthodontic intervention.
Although the available data suggest that interceptive orthodontic treatment can be effective, no randomized clinical trials or large cohort studies have compared interceptive outcomes with no treatment in either the near or long term. This has been primarily due to the lack of suitable cohorts of untreated patients with malocclusions to serve as control subjects. During the 1970s, the orthodontic faculty at the University of Bergen in Norway collected orthodontic study casts biannually from many local school children. A substantial number of these children had orthodontic needs and were not treated during the mixed dentition. Thus, it was possible to collect an archival cohort of study casts of untreated subjects with excellent matching for malocclusion severity to compare with a contemporary sample of patients treated in an interceptive clinic. We hypothesized that interceptive orthodontic treatment would improve malocclusions with reductions in their complexity and need.
Material and methods
This was a retrospective cohort design. Power calculations were based on a similar study with a 40% improvement in ICON scores after interceptive treatment. A sample size of 100 provided a power of 90% and an alpha of 0.05 for this level of difference in ICON scores. For the treated group, 133 patients with pre- and postinterceptive sets of dental casts were selected from consecutively treated patients who met our inclusion criteria and were treated in the orthodontic clinic at the University of Bergen by dental students supervised by orthodontic faculty members. Most of these patients were treated for dental misalignment, crowding or spacing, inversions, anterior open bite, and crossbite with various removable appliances. The control group, consisting of 113 patients with 2 sets of dental casts that also met the inclusion criteria, was randomly selected from departmental archives of biannual records of school children taken during the 1970s. Inclusion and exclusion criteria were initial casts in the early mixed dentition, final casts after interceptive orthodontic treatment but no later than the late mixed dentition (ie, final casts with a fully erupted permanent dentition mesial to the first molars were excluded), final casts for the control group who received no orthodontic treatment were taken 2 years after the first, initial casts showing a malocclusion suitable for funding under the Norwegian Social Security System as judged subjectively by an orthodontist (P.B.) experienced with these criteria, Scandinavian ethnicity, and no exclusion based on sex.
All casts were scored with the ICON by a calibrated examiner (G.J.K.) who was not blinded to group or time point. True blinding was not possible because the casts of the control group were easily recognizable because of their rough trimming, and the time points were obvious based on the stage of tooth development evident on the casts. The ICON scores overall occlusion and an esthetic component of malocclusion on an interval scale, from 0 to 120 for the former and 0 to 10 for the latter. The higher the ICON score, the worse the malocclusion. The ICON has been validated based on the subjective judgments of 97 orthodontists from 9 countries on 240 initial and 98 treated dental casts. Created as a single measure of need, complexity, and outcome simultaneously, the ICON has 2 advantages over the more commonly used PAR as a dental outcome measure. It has an esthetic component that is weighted highly by clinicians and valued by patients, and it has clear and internationally validated cut points for treatment need and outcome with categories for complexity and improvement. Five weighted parameters are scored and comprise the components of the ICON: dental esthetics, crossbite, anterior vertical relationship, maxillary crowding or spacing, and buccal segment anteroposterior relationship. The components were individually scored from dental casts and multiplied by their respective weights to yield a single summary ICON score. This final score was then used to determine initial need (ICON >43) and final outcome acceptability (ICON <31), and difference scores were used to determine improvement. According to the convention recommended by the developers of the ICON, improvement scores were calculated by subtracting 4 × final scores from the initial scores. This permitted us to compare the improvement in our samples with the categories validated for the ICON. Intrarater reliability of the examiner was determined by using Dahlberg’s formula on 10 sets of models remeasured 2 weeks apart and was considered to be acceptable (4.1 ICON points).
Initial equivalence of the groups was assessed by using age, sex, and malocclusion characteristics. The latter consisted of weighted initial ICON scores and unweighted ICON component scores. Equivalence in ICON components was assessed by using multiple unpaired t tests with Bonferroni adjustments for multiple comparisons. Since 7 tests were performed, the level of significance was set at P <0.007 (ie, P <0.05/7). ICON scores were compared between groups and at the 2 time points with 2-way analysis of variance (ANOVA) and post-hoc comparisons with the Kruskal-Wallis test if P <0.05. Initial need was determined by using the weighted ICON score threshold of >43, and end-of-study acceptability was determined with the <31 threshold. The prevalences of subjects in the initial complexity grades and improvement categories were also calculated, and these distributions were compared between groups by using the chi-square statistic. Unweighted ICON component scores were compared between initial and final casts, and differences were assessed with multiple t tests with Bonferroni adjustments and significance set at P <0.007.
Results
Initially, the subjects in the interceptive and control groups had mean chronological ages of 9.4 years (± 1.4) and 9.3 years (± 0.8), respectively ( Table I ). These were not different. However, although the treated group was about equally divided by sex (51.6% female), the control group was predominantly male (31.8% female). These were statistically different ( P = 0.017). As assessed by the unweighted ICON component scores, the malocclusions in the 2 groups were largely well matched, with moderate esthetics scores, minimal maxillary crowding or spacing and openbite or overbite, and moderate buccal anteroposterior occlusal relationships. Statistical differences were found only in maxillary anterior spacing ( P <0.006) and crossbite ( P <0.000).
| lnterceptive | Control | P value | |
|---|---|---|---|
| Age (y) (SD) | 9.4 (1.4) | 9.3(0.8) | 0.590 |
| Female (%) | 51.6 | 31.8 | 0.017 |
| Mean ICON (SD) unweighted components | |||
| Esthetics (1-10) | 5.3(1.8) | 5.2 (1.7) | 0.469 |
| Crowding (0-5) | 0.6 (1.3) | 0.4 (1.6) | 0.414 |
| Spacing (0-5) | 0.2 (0.5) | 0.4 (0.7) | 0.006 |
| Crossbite (0-1) | 0.6 (0.5) | 0.2 (0.4) | 0.000 |
| Open bite (0-4) | 0.3 (1.0) | 0.2 (0.6) | 0.277 |
| Overbite (0-3) | 0.6 (0.8) | 1.0 (0.9) | 0.008 |
| Buccal AP (0-2) | 1.1 (0.8) | 1.2 (0.5) | 0.500 |
Table II shows that both groups had similar ICON scores when the first models were taken (54.9 and 54.0, respectively). Based on the validated ICON assessment of need (>43), both groups of subjects needed treatment. The intervals between the first and second sets of casts averaged 27.2 months (± 16.3) in the treated group and 24.4 months (± 3.6) in the control; these were not different. At the second time point, the mean ICON scores were 33.6 (± 16.1) for the treated group and 54.2 (± 16.9) for the untreated controls. This represented a 38.8% improvement for the former ( P <0.0001) and no change for the latter. Based on the ICON acceptability cut point of <31, both groups would be judged unacceptable, but the treated cohort was borderline.
| lnterceptive (n = 133) |
Control (n = 113) |
ICON cut points (need or acceptability) |
|
|---|---|---|---|
| Initial mean ICON (SD) | 54.9 (16.6) | 54.0 (14.8) | >43 |
| Final mean ICON (SD) | 33.6 (16.1) ∗ | 54.2 (16.9) | <31 |
| lmprovement % | 38.8 | −0.9 |
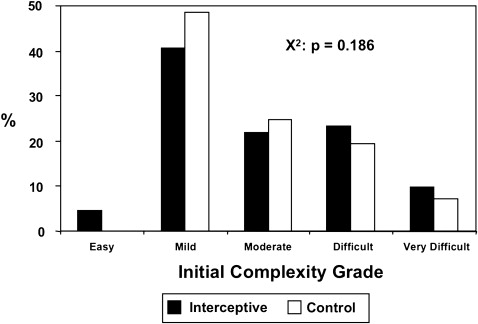
The distributions of the initial complexity grades ( Fig 1 ) were not different between the groups (chi-square: P = 0.186). Figure 2 gives a comparison of the distributions of improvement grades between the 2 groups. The difference between these was highly significant (chi-square, P <0.0001). Whereas most subjects were categorized as “not improved or worse” in the untreated control group (89.4%), the treated group had 36.1% in that category. This reduction was reflected by roughly equivalent increases in the “minimal,” “moderate,” and “substantial” improvement categories for the treated subjects (22.6%, 21.1%, and 17.3%, respectively) compared with the controls (7.9%, 1.8%, and 0.9%, respectively).