Introduction
The purpose of this study was to investigate the effect of piezocision on orthodontically induced inflammatory root resorption.
Methods
Fourteen patients were included in this split-mouth study; 1 side was assigned to piezocision, and the other side served as the control. Vertical corticotomy cuts of 4 to 5 mm in length were performed on either side of each piezocision premolar, and 150-g buccal tipping forces were applied to the premolars. After 4 weeks, the maxillary first premolars were extracted and scanned with microcomputed tomography.
Results
There was a significantly greater total amount of root resorption seen on the piezocision sides when compared with the control sides ( P = 0.029). The piezocision procedure resulted in a 44% average increase in root resorption. In 5 patients, there was noticeable piezocision-related iatrogenic root damage. When that was combined with the orthodontic root resorption found on the piezocision-treated teeth, there was a statistically significant 110% average increase in volumetric root loss when compared with the control side ( P = 0.005).
Conclusions
The piezocision procedure that initiates the regional acceleratory phenomenon may increase the iatrogenic root resorption when used in conjunction with orthodontic forces. Piezocision applied close to the roots may cause iatrogenic damage to the neighboring roots and should be used carefully.
Highlights
- •
Piezocision might cause increased root resorption when used with orthodontic forces.
- •
Piezocision-related iatrogenic root damage occurred in 5 of 14 participants.
- •
Piezocision should not be used in areas of close root proximity.
Orthodontically induced inflammatory root resorption is defined as the loss of dental hard tissues caused by clastic cellular activity. It is an undesirable and often unpredictable side effect of orthodontic tooth movement, with a complex and multifactorial etiology.
Orthodontic tooth movement relies on the complicated changes that occur in the periodontal ligament, supporting alveolar bone, and tissues with differing cell populations and differing remodeling capabilities. During tooth movement, the production of hyalinization regions in the periodontal tissues occurs particularly upon the application of heavy forces. The removal of these hyalinization zones by osteoclasts has been associated with orthodontic root resorption.
Corticotomies have been discussed in the orthodontic literature as a means for accelerating the rate of tooth movement for over 100 years. Initially, it was believed that corticotomies accelerated tooth movement because of segmentation of alveolar bone and the en-masse movement of the teeth and associated block of bone. More recent research has used corticotomies as a means of accelerating the rate of bone turnover. Corticotomy accelerates orthodontic tooth movement via the activation of a regional acceleratory phenomenon (RAP). The RAP effect usually commences within a few days of injury, peaks at 1 to 2 months, and lasts for 2 to 4 months, with up to 6 to 24 months reported in the literature. This normal healing process involves the acceleration of growth, remodeling, metabolism, healing, inflammation, perfusion, cell turnover, and repair of microdamage.
The corticotomy-induced RAP response accelerates tooth movement by producing temporary demineralization/osteopenia in the bone surrounding the roots of activated teeth. These teeth that have been activated by corticotomies experience more rapid and extensive alveolar bone and periodontal ligament turnover. The literature has demonstrated that corticotomies can increase the rate of orthodontic tooth movement by up to 2 to 3 times the normal rate.
There is only limited evidence in the orthodontic literature that demonstrates a statistically significant reduction in the amount of root resorption with the use of corticotomy procedures, when compared with normal tooth movement.
Piezocision is a more conservative and less invasive variation of the traditional corticotomy technique. It involves the use of an ultrasonic cutting instrument to make the corticotomy incisions, without the need for raising a soft tissue flap. It has been claimed that piezocision can produce comparable rates of accelerated tooth movement to more conventional corticotomy procedures.
The aim of this pilot study was to investigate the effect of piezocision on root resorption when 150-g buccal tipping forces were applied to maxillary first premolars for a 4-week period. A qualitative and quantitative assessment of the degree of root resorption was performed by microcomputed tomography scanning of the extracted premolars.
Material and methods
The sample consisted of 28 maxillary first premolars that were extracted bilaterally from 14 patients. There were 6 male and 8 female patients (mean age, 16 years 2 months; range, 13 years 1 month to 19 years 0 month). They required the extraction of maxillary first premolars as part of their orthodontic treatment. Ethics approval was granted by the Sydney Local Health District, RPAH Zone (ethics approval numbers X13-0371 and HREC/13/RPAH/519). The patients were carefully selected according to previously described strict inclusion criteria, and written informed consent was obtained.
After the collection of pretreatment records, the subjects had a baseline periodontal checkup for standardized periodontal measurements and oral hygiene control before the experiment.
Using a split-mouth study design, we allocated the maxillary first premolars to 1 of 2 groups for each participant. One side was chosen to have the piezocision procedure performed, with the other side acting as the control. In some participants, it was apparent that there was limited interradicular space between the maxillary first premolar and canine or second premolar. There was concern that randomization might result in iatrogenic damage to the teeth when performing the piezocision procedure, so the side with the least risk of causing root damage was selected.
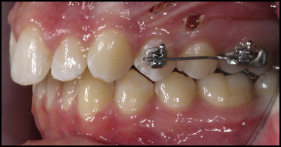
The subjects had partial fixed appliances placed on the maxillary first premolars and first molars bilaterally. Self-ligating 0.022-in SPEED brackets and tubes were used (Strite Industries, Cambridge, Ontario, Canada). Buccal tipping forces (150 g) were applied to the maxillary first premolars by 0.017 × 0.025 Beta III Titanium (3M Unitek, Monrovia, Calif) cantilever springs. The springs were inserted into the maxillary first molar and first premolar brackets and bypassed the maxillary second premolar ( Fig 1 ).
The force produced by the springs was calibrated with a strain gauge (Dentaurum, Ispringen, Germany) and customized to each premolar. Once the springs were fitting well and generating 150 g of force, they were taken out of the brackets to allow unimpeded access to the surgical site. In addition, occlusal stops (Transbond Plus Light Cure Band Adhesive; 3M Unitek) were placed onto the mesiopalatal cusps of the maxillary first molars to prevent occlusal interferences and allow uninhibited tipping of the maxillary first premolars during the experiment.
At the same appointment, the piezocision procedure was performed on 1 maxillary first premolar. A surgical setup was used for all subjects, with a sterile field of operation. Local anesthetic was administered (Lignospan lidocaine hydrochloride 2%, 1:100,000 Adr; Septodont, France), and then a soft tissue laser (Picasso; AMD Lasers, Indianapolis, Ind) was used to produce 2 buccal vertical interproximal incisions into the gingiva/mucosa, one on the mesial side and one on the distal side of the first premolar. The incisions were made apical to the interdental papilla, 5 to 7 mm long. A piezocision blade (VarioSurg Ultrasonic Bone Surgery System; NSK-Nakanishi, Tochigi, Japan) was then inserted into the soft tissue incision, as per the technique of Dibart et al and Dibart and Dibart. The piezocision blade was used to produce a vertical corticotomy cut into the buccal cortical plate, mesial and distal to the buccal root of the maxillary first premolar. Each alveolar bone corticotomy cut was 4 to 5 mm long and made to a depth of 2 to 3 mm. When the maxillary first premolar root was close to the canine or second premolar root, the depth of the corticotomy cut was reduced to prevent iatrogenic root damage. Once the piezocision procedure had been completed, no suturing was required for the vertical soft tissue incisions ( Fig 2 ).

The calibrated beta-titanium alloy springs were replaced into their corresponding brackets and left in place for the 4-week experimental period, with no reactivation.
All surgical procedures were performed by 1 clinician (S.M.) from the periodontology department. All orthodontic procedures were performed by 1 clinician (B.P.) from the orthodontics department, both from the University of Sydney.
Two weeks after the piezocision procedure, standardized periodontal parameters were retaken, and the subjects were checked for any issues regarding the piezocision procedure.
After 4 weeks of buccal tipping force application, the partial fixed appliances and occlusal stops were removed. Final standardized periodontal measurements were taken. The maxillary first premolars were carefully extracted by 1 operator (B.P.) to ensure that minimal damage occurred to the root surfaces. The teeth were not luxated; only forceps were used.
The extracted first premolars were then stored and prepared according to previously established protocols. The teeth were stored in deionized water (Milli Q; Millipore, Bedford, Mass). An ultrasonic bath was used for 10 minutes to allow the removal of soft tissue and periodontal fragments from the root surface. Any residual periodontium was carefully removed with damp gauze. Disinfection was achieved by placing the teeth into 70% isopropyl alcohol for 30 minutes, followed by bench drying at room temperature (23°C ± 2°C) for at least 48 hours.
A desktop x-ray microtomograph machine (SkyScan 1172; Bruker, Aartselaar, Belgium) was used to scan each tooth specimen. This microcomputed tomography unit produces high-resolution 3-dimensional images from multiple 2-dimensional (2D) x-ray shadow transmission images of the specimen at differing angulations.
The teeth were scanned individually, from a position just apical to the cementoenamel junction to the root apex. Specimens were scanned 180° around the vertical axis, with image resolution set at 17.6 μm.
The image data from the SkyScan unit was then reconstructed with its own proprietary software, NRecon (version 1.6.9.18; Bruker). This program relies on a modified Feldkamp cone-beam algorithm to produce slice-by-slice axial reconstruction. The settings for NRecon were standardized for all images. The reconstructed slices were saved in 16-bit tagged image file format (TIFF).
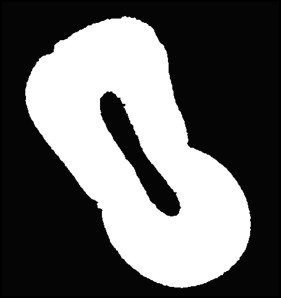
Root resorption crater detection and quantification were performed using the imaging software program Fiji (version 2.0.0-rc-15/1.49k; available at http://imagej.net/Contributors ), along with a custom macro (Enigma; Australian Centre for Microscopy and Microanalysis, University of Sydney). All axial slices of the image stack for each specimen were manually examined for resorption craters. Each image slice needed to be converted to a binary image (black and white) before crater calculation ( Fig 3 ).
Once a crater was detected, it was highlighted with a clipping tool and duplicated into its own image sequence to allow Enigma to calculate the volume of each crater in cubic millimeters. All measurements were carried out by 1 operator (B.P.) to reduce error and bias. Craters were categorized as located on the buccal, palatal, mesial, or distal surface, with the 3 vertical location designated as the cervical, middle, or apical third of the root. Total root resorption volume was also recorded for each tooth.
For 3-dimensional image reconstruction (Avizo Fire version 8.1.0; Konrad-Zuse-Zentrum, Berlin, Germany) was used to create and view selected specimens ( Fig 4 ).
Statistical analysis
The SPSS statistics program (version 21; IBM, Armonk, NY) was used for statistical analysis. Paired t tests were used to determine whether there were any statistically significant differences in the data of the piezocision-related root resorption compared with the nonpiezocision root resorption. This included comparing the total resorption crater volume per tooth for each root surface (buccal, palatal, mesial, and distal) and for each vertical third (cervical, middle, and apical). All analyses were assessed with P <0.05 considered statistically significant.
The root resorption crater volumes of 6 randomly selected teeth were remeasured to determine the overall standard error of the measurements and the coefficient of variation.
Results
All 14 patients completed the study, with all 28 premolars deemed eligible for assessment and inclusion in the study.
Overall, more root resorption was seen on the piezocision teeth than on the control teeth ( Fig 5 ).
For the total volumes of root resorption cratering per tooth, the piezocision teeth averaged 0.435 mm 3 , and the control teeth averaged 0.302 mm 3 . This resulted in the piezocision procedure producing an average of 0.133 mm 3 , or 44%, more root resorption than did the corresponding control teeth. The difference was statistically significant ( P = 0.029). Only 4 participants demonstrated less total root resorption with the piezocision procedure when compared with the contralateral control teeth ( Table I ).
| Subject | Total resorption per tooth (mm 3 ) | Piezocision damage (mm 3 ) | Damage + piezocision side (mm 3 ) | |
|---|---|---|---|---|
| Piezocision side | Nonpiezocision side | |||
| 1 | 0.455 | 0.447 | 0 | 0.455 |
| 2 | 0.122 | 0.176 | 0.725 | 0.847 |
| 3 | 0.263 | 0.170 | 0.212 | 0.475 |
| 4 | 0.395 | 0.180 | 1.116 | 1.511 |
| 5 | 0.340 | 0.381 | 0.547 | 0.886 |
| 6 | 0.315 | 0.267 | 0 | 0.315 |
| 7 | 0.157 | 0.153 | 0.173 | 0.330 |
| 8 | 0.717 | 0.399 | 0 | 0.717 |
| 9 | 0.396 | 0.422 | 0 | 0.396 |
| 10 | 1.109 | 0.710 | 0 | 1.109 |
| 11 | 0.551 | 0.320 | 0 | 0.551 |
| 12 | 0.121 | 0.295 | 0 | 0.121 |
| 13 | 0.445 | 0.127 | 0 | 0.445 |
| 14 | 0.711 | 0.180 | 0 | 0.711 |
| Total | 6.095 | 4.228 | 2.772 | 8.867 |
| Mean | 0.435 | 0.302 | 0.198 | 0.633 |
| SD | 0.271 | 0.161 | 0.350 | 0.365 |
The root resorption data were also assessed in terms of distribution on the buccal, palatal, mesial, and distal surfaces for each tooth. The piezocision teeth demonstrated marginally more root resorption on the buccal, palatal, mesial, and distal surfaces when compared with the control teeth. However, no results had statistical significance ( Table II ).
| Tooth surface | Piezocision | Mean | SD | Nonpiezocision | Mean | SD | t test, P |
|---|---|---|---|---|---|---|---|
| Buccal | 2.052 | 0.147 | 0.099 | 1.318 | 0.094 | 0.075 | 0.072 |
| Palatal | 0.824 | 0.059 | 0.059 | 0.599 | 0.043 | 0.038 | 0.298 |
| Mesial | 1.911 | 0.136 | 0.116 | 1.361 | 0.098 | 0.091 | 0.313 |
| Distal | 1.309 | 0.093 | 0.117 | 0.951 | 0.068 | 0.077 | 0.295 |
| Total | 6.096 | 4.229 | |||||
When we examined the root resorption crater distribution on the cervical, middle, and apical thirds of the teeth, the piezocision-treated teeth exhibited more root resorption in all vertical thirds than did the control teeth, but these results were not statistically significant ( Table III ).
| Tooth third | Piezocision | Mean | SD | Nonpiezocision | Mean | SD | t test, P |
|---|---|---|---|---|---|---|---|
| Cervical | 2.764 | 0.197 | 0.111 | 2.040 | 0.146 | 0.093 | 0.217 |
| Middle | 1.865 | 0.133 | 0.154 | 1.128 | 0.081 | 0.098 | 0.075 |
| Apical | 1.466 | 0.105 | 0.130 | 1.061 | 0.076 | 0.075 | 0.203 |
| Total | 6.095 | 4.229 | |||||
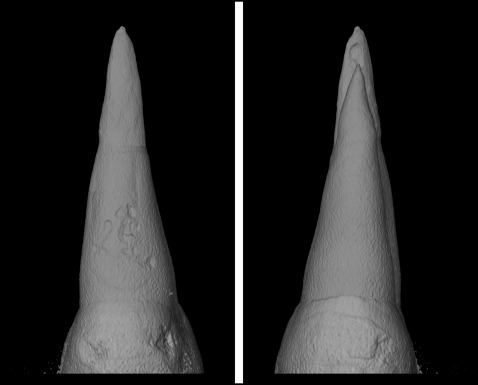
During the assessment of each maxillary first premolar with the microcomputed tomography machine, we noted that 5 participants had considerable iatrogenic root damage from the piezocision surgical procedure. The shape of the piezocision-related damage was clearly differentiated from the orthodontically induced inflammatory root resorption. Iatrogenic piezocision damage appeared as long, narrow, and deep vertical defects, with a sawtooth shape of the floor of the damage crater that corresponded to the piezocision blade configuration, whereas orthodontic root resorption craters had a much shallower and broader form ( Fig 6 ).




