Introduction
Despite the many advances to improve the practice of orthodontics, white spot lesions, or decalcifications, remain a common complication in patients with poor oral hygiene. The purpose of this study was to assess the perceptions and level of awareness of patients, parents, orthodontists, and general dentists toward the development of white spot lesions during orthodontic treatment.
Methods
This was a prospective epidemiologic survey of the perceptions of orthodontic patients (n = 315), parents (n = 279), orthodontists (n = 305), and general dentists (n = 191) regarding the significance, prevention, and treatment of white spot lesions.
Results
All surveyed groups indicated that white spot lesions detracted from the overall appearance of straight teeth, attributed primary responsibility for the prevention of white spot lesions to the patients themselves, and thought that the general dentist should be responsible for treating white spot lesions. Patients regarded themselves as ultimately responsible for the prevention of white spot lesions ( P <0.05).
Conclusions
The patients, parents, orthodontists, and general dentists had similar perceptions regarding the significance, prevention, and treatment of white spot lesions. All groups indicated that patients were the most responsible for the prevention of white spot lesions. Communication among patients, parents, orthodontists, and general dentists needs to improve to decrease the incidence of white spot lesions in the orthodontic population.
Despite the many advances to improve the practice of orthodontics, enamel decalcifications, or white spot lesions, are the most frequent complication with fixed appliance therapy. The debonding appointment is generally an exciting time for the patient, parents, orthodontist, and staff. White spot lesions, however, can detract from the quality of the treatment results and cause disappointment among patients, parents, and dental professionals.
White spot lesions are defined as “subsurface enamel porosities from carious demineralization” with “a milky white opacity . . . when located on smooth surfaces.” Changes in light scattering of the decalcified, porous enamel causes the white appearance. These white spot lesions rarely progress to significant cavitations and are generally not registered as caries requiring restorative treatment in the decayed, missing due to caries, filled teeth (DMFT) index.
White spot lesions can form within 4 weeks, which is typically within the time frame between subsequent orthodontic appointments. Orthodontic attachments in the oral cavity make the mechanical removal of plaque somewhat difficult. In addition, lack of compliance in maintaining adequate oral hygiene can predispose orthodontic patients to white spot lesions. To prevent decalcification and formation of white spot lesions, a good oral-hygiene regimen must be implemented, including proper toothbrushing with a fluoridated dentifrice. Fluoride concentrations below 0.1% should not be recommended for orthodontic patients. For less compliant patients, the use of a fluoridated dentifrice alone is ineffective in preventing the development of carious lesions. Orthodontic patients are therefore requested to use a fluoride mouth rinse (0.05% sodium fluoride) daily in addition to fluoride toothpaste. Fluoride rinses have been shown to significantly reduce white spot lesions during orthodontic therapy.
Unfortunately, these preventive measures depend on patient compliance. Geiger et al reported that less than 15% of orthodontic patients rinsed daily as instructed. Poor patient compliance is a well-documented problem in the dental and medical literature; Wilson et al showed that only 16% of patients who received extensive periodontal therapy complied with the recommended maintenance schedules.
Orthodontic patients develop significantly more white spot lesions than nonorthodontic patients, and these white spot lesions can cause esthetic problems years after treatment. Gorelick et al found that the incidence of at least 1 white spot lesion was 50% in patients who had treatment with fixed orthodontic appliances compared with only 24% in untreated controls. Similarly, Sandvik et al found that about 50% of patients receiving orthodontic treatment developed at least 1 white spot lesion during treatment compared with 11% in untreated controls. In a more recent study, Richter et al reported that an alarming 72.9% of patients developed at least 1 white spot lesion during orthodontic treatment, of which 2.3% showed cavitations.
White spot lesions are difficult to treat and are often permanent, regardless of the treatment approach. Reexamination of 40 subjects who had participated in a randomized controlled clinical study on the effect of a caries-preventive program 6 years after debonding showed that about 75% of the small white spot lesions had regressed during that period. Twenty-five percent of the most severe lesions remained visible on the surfaces.
Patients respond differently to white spot lesions; thus, the recommended course of treatment should be unique to each patient. Ideally, patients and orthodontists should work together to help prevent white spot lesions from developing during treatment. The purpose of this study was to assess the perceptions and levels of awareness of patients, parents, orthodontists, and general dentists toward the development of white spot lesions during orthodontic treatment.
Material and methods
Virginia Commonwealth University in Richmond granted institutional review board approval to conduct this study.
The American Association of Orthodontists and the American Dental Association granted permission to conduct the study. The American Association of Orthodontists provided the names and addresses of all member orthodontists under the age of 60 practicing in Virginia, Maryland, and North Carolina (total, 608 orthodontists). The American Dental Association provided the names and addresses of 500 general dentists under the age of 60 randomly chosen from Virginia, Maryland, and North Carolina. Twenty-one addresses from the American Association of Orthodontists and 5 from the American Dental Association were not recognized by the post office as deliverable addresses. Surveys were therefore mailed successfully to 587 orthodontists and 495 general dentists, and included an addressed postage-paid return envelope. The envelopes were numerically coded to identify nonrespondents. A follow-up survey was sent to those who did not return the questionnaire.
Patient and parent participants were recruited from 7 orthodontic offices that voluntarily participated in this study. Five offices were located in Virginia and 2 in North Carolina. Each office was given 100 surveys, and the receptionist at each office asked patients and parents to participate in the study. Fifty surveys were to be completed by active orthodontic patients in full fixed appliances, and 50 were to be completed by parents of patients receiving active orthodontic treatment. The total number of surveys distributed to the 7 offices was 700 (350 to each group of patients and parents, respectively).
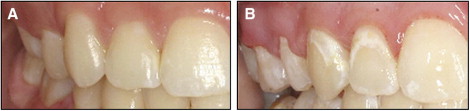
Four analogous surveys were designed to assess the perceptions and levels of awareness of patients, parents, orthodontists, and general dentists toward the development of white spot lesions during orthodontic treatment. The survey distributed to patients is given in the Appendix . The front page of each survey explained the purpose of the study and included 2 color intraoral photographs of the right side of a well-aligned dentition ( Fig ). The teeth in photograph A had no visible white spot lesions, but the teeth in photograph B showed visible white spot lesions.
All questions were multiple choice, and 4 identical questions were asked so that responses could be compared directly. These questions were (1) how much do white spots make straight teeth look worse? (2) who do you think is responsible for the prevention of white spots from braces? (3) who do you think is most responsible for the prevention of white spots from braces? and (4) who should treat white spots on teeth from braces? No identifying information was requested, so the answers were anonymous. The surveys were also pretested before implementation to improve the design and thereby increase the response rate.
Patients and parents were asked several additional multiple-choice questions. Patients were asked how long they had been wearing braces, what they did to take care of their teeth during treatment with braces, and whether they were instructed on how to prevent white spot lesions. Both patients and parents were asked why they thought people get white spot lesions on their teeth from braces. Parents were also asked whether they thought their child needed more instruction on white spot lesions, whether they were worried that their child would have white spot lesions at the end of treatment with braces, and, if their child had white spot lesions, would they recommend treatment with braces to a friend.
Statistical analysis
Chi-square analyses were used to determine differences in responses among the 4 groups. JMP statistical software (version 8.0.2.; SAS Institute, Cary NC) was used for these analyses. Patterns in the differences were identified by large-cell chi-square values. Multi-nomial logistic regression was used to investigate the relationships between perceptions, prevention and treatment of white spot lesions (dependent variables), and patient variables (age, time wearing braces, methods of taking care of teeth, and instruction on preventing white spot lesions). The latter analyses were performed with a statistical package (version 19.0.0 for Windows 2010; IBM SPSS, Somers, NY).
Results
A total of 1090 surveys (61%) were returned. These included responses from 305 orthodontists (52%), 191 general dentists (39%), 315 patients (90%), and 279 parents (80%). Seventy-six percent of orthodontists, 77% of general dentists, 40% of patients, and 41% of parents who completed a survey were male. Unanswered questions and questions requiring 1 response with more than 1 response were omitted. Overall, 269 of 10,585 responses (2.5%) were discarded.
The ages in the patient group ranged from 7 to 69 years, 39% had been wearing braces for less than a year, 41% for more than 1 but less than 2 years, and 19% for more than 2 years. Five patients were not wearing braces and were excluded from the study.
Table I illustrates the responses to question 3, which examined the perceived significance of white spot lesions among the groups. Reference was made to the colored photos in the Figure . A small percentage of respondents from all groups perceived that white spot lesions made the teeth look “no worse.” Similar proportions of patients, parents, and general dentists perceived that white spot lesions would make the teeth look either “a little worse” or “a lot worse” ( P >0.05). However, a greater proportion of orthodontists (60%) indicated that white spot lesions made the teeth look “a lot worse” compared with the other groups ( Table I , P <0.05). Multi-nomial logistic regression was used to determine whether patient factors (independent variables) were predictive of the perceived significance of white spot lesions (dependent variable). The analysis showed that use of a fluoride rinse was the only factor associated with patient perceptions ( P <0.05).
| Group | No worse | A little worse | A lot worse | Total |
|---|---|---|---|---|
| Patients | 25 (8%) | 140 (46%) | 142 (46%) | 307 |
| Parents | 17 (6%) | 122 (45%) | 134 (49%) | 273 |
| Orthodontists | 2 (1%) | 117 (40%) | 175 (60%) ∗ | 294 |
| General dentists | 2 (1%) | 95 (51%) | 90 (48%) | 187 |
| Total | 46 (4%) | 474 (45%) | 541 (51%) | 1061 |
∗ Significant difference between orthodontists and other groups ( P <0.05).
Table II shows the responses to question 4, which examined the perceived responsibility for the prevention of white spot lesions. More than 1 response was acceptable. All groups indicated joint responsibility among patients, parents, orthodontists, and general dentists. Nearly all respondents indicated that patients were responsible for the prevention of white spot lesions, including the patients themselves. Only 17% of the patients thought that prevention of white spot lesions was their parents’ responsibility ( P <0.05). However, 72% of parents held themselves responsible for white spot lesions prevention. Most orthodontists (82%) regarded themselves responsible for prevention of white spot lesions. In addition, most general dentists (82%) perceived that orthodontists were responsible for the prevention of white spot lesions. Patients and parents indicated less often than orthodontists and general dentists that dental professionals were responsible for preventing white spot lesions ( P <0.05, Table II ).
| Group | Responses | Total | |||
|---|---|---|---|---|---|
| Patients | Parents | Orthodontists | Dentists | ||
| Patients | 291 (94%) | 54 (17%) ∗ | 97 (31%) † | 89 (29%) † | 310 |
| Parents | 251 (92%) | 197 (72%) | 150 (55%) † | 106 (39%) † | 274 |
| Orthodontists | 299 (98%) | 275 (90%) | 262 (86%) | 194 (64%) | 304 |
| General dentists | 182 (95%) | 162 (85%) | 157 (82%) | 132 (69%) | 191 |
| Total | 1023 (95%) | 688 (64%) | 666 (62%) | 521 (48%) | 1079 |
∗ Significant difference between patients and other groups ( P <0.05).
† Significant differences between laypeople (patients and parents) and dental professionals ( P <0.05).
Table III illustrates the responses to question 5, which investigated perceptions of who was the most responsible for the prevention of white spot lesions from braces. The majority of subjects in all 4 groups selected patients as most responsible for the prevention of white spot lesions from braces. Patients indicated that they themselves were the most responsible more often than the other groups ( P <0.05). Only 9 respondents (1%) indicated that dentists were the most responsible for the prevention of white spot lesions ( Table III ). Multi-nomial logistic regression showed that age and time wearing braces were associated with patient perceptions of who was the most responsible for preventing white spot lesions ( P <0.05).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


