Abstract
Objectives
Our goal is to review design strategies for the fabrication of calcium phosphate ceramic scaffolds (CPS), in light of their transient role in bone tissue engineering and associated requirements for effective bone regeneration.
Methods
We examine the various design options available to meet mechanical and biological requirements of CPS and later focus on the importance of proper characterization of CPS in terms of architecture, mechanical properties and time-sensitive properties such as biodegradability. Finally, relationships between in vitro versus in vivo testing are addressed, with an attempt to highlight reliable performance predictors.
Results
A combinatory design strategy should be used with CPS, taking into consideration 3D architecture, adequate surface chemistry and topography, all of which are needed to promote bone formation. CPS represent the media of choice for delivery of osteogenic factors and anti-infectives. Non-osteoblast mediated mineral deposition can confound in vitro osteogenesis testing of CPS and therefore the expression of a variety of proteins or genes including collagen type I, bone sialoprotein and osteocalcin should be confirmed in addition to increased mineral content.
Conclusions
CPS are a superior scaffold material for bone regeneration because they actively promote osteogenesis. Biodegradability of CPS via calcium and phosphate release represents a unique asset. Structural control of CPS at the macro, micro and nanoscale and their combination with cells and polymeric materials is likely to lead to significant developments in bone tissue engineering.
1
Introduction
Autologous bone grafts remain the gold standard in bone replacement procedures with the highest success rates for bone regeneration . It is well established, however, that harvest of bone tissue is associated with several clinical drawbacks, including limited availability of healthy bone, secondary surgery cost and burden, harvest site morbidity and long-term pain issues . There is therefore a critical need for synthetic bone graft materials capable of promoting successful bone regeneration. Indeed the past two decades have been associated with sustained interdisciplinary efforts to design and develop synthetic scaffolds encompassing a wide range of materials from ceramics to polymers, including composite scaffolds, cell-bearing, protein-loaded or growth factor-carrying scaffolds mixing both inorganic and organic phases .
Amongst available scaffold materials, calcium phosphate-based ceramics represent a unique avenue based on tunable similarities in both crystalline structure and chemistry between calcium phosphate ceramics and bone apatite, the mineral phase of bone tissue that is similar, albeit distinct, from hydroxyapatite (HA) due to its carbonate content and reduced or absent hydroxyl groups . A literature search associating the terms “calcium” and “phosphate” and “scaffolds” returned a total of more than 7000 articles. This interest appears to have gathered momentum in the past 15 years, although HA, and more generally calcium phosphate-based ceramics have long been the focus of extensive research . Calcium phosphate ceramics have been shown to enhance bone formation depending on crystallinity, crystalline phase and Ca/P ratio, which results in calcium and phosphate ion release needed for bone mineralization . This characteristic uniquely differentiates them from other metal oxide ceramics used in orthopedics, such as alumina or zirconia that are considered chemically inert. The importance of a scaffold-type architecture stems from the fact that interconnected porosity is a condition for osteoconductivity and promotes angiogenesis. Furthermore, there is ample literature showing that calcium phosphate bioceramic scaffolds promote both osteogenesis and osseointegration, which are directly related to surface charge, chemistry and topography. However, it should be noted that the target application for calcium phosphate scaffolds (CPS) is transient bone replacement. Therefore, the degree of mimicry with regard to bone does not extend beyond chemistry, surface topography and architecture. Bone becomes stiffer and stronger as it matures while CPS should biodegrade and become weaker, with the end point of being completely replaced by newly formed bone.
CPS are manufactured using a palette of techniques from polymer foam replication to ceramic foaming, inclusion of porogens, 3D printing and gel casting. This variety of manufacturing techniques illustrates the difficulty of producing ceramic scaffolds with controlled pore size, porosity and mechanical integrity. Regardless of manufacturing technique, the last step is a thermal treatment or sintering step. This high temperature step has traditionally triggered design issues due to the competition between the high temperatures required for sintering and crystalline phase thermal decomposition. Additionally, for bioactive glass-ceramics, competition between sintering and crystallization processes renders sintering to full density difficult to achieve.
Our goal is to review design strategies for the fabrication of CPS, in light of their transient role in bone tissue engineering and associated requirements for effective bone regeneration. We later focus on the importance of proper characterization of CPS in terms of architecture, mechanical properties and time-sensitive properties such as biodegradability. Finally, relationships between in vitro versus in vivo testing are addressed, with an attempt to highlight reliable performance predictors.
1.1
Design requirements for CPS as bone graft substitutes
As mentioned earlier, an ideal scaffold material for synthetic bone grafts should be osteoinductive, osteoconductive, promote osseointegration, be able to deliver osteogenic agents, anti-infectives and stem cells, and degrade at the same rate as new bone forms . Calcium phosphate ceramic scaffolds are therefore excellent candidates, offering a large palette of design options as detailed below.
1.1.1
Osteoinduction and biodegradation
Osteoinduction can be defined as the chemical stimulation of human mesenchymal stem cells into bone-forming osteoblasts, thereby inducing osteogenesis . Osteoinduction is best demonstrated by the ability of a material to form bone in an ectopic site . Calcium phosphate ceramics have been shown to be osteoinductive . It is postulated that osteoinductivity of CPS stems from the combination of micro and macroporosity capable of entrapping and concentrating growth factors that are directly involved in mesenchymal stem cell differentiation into an osteoblastic lineage . The surface and bulk chemistry of the crystalline phases involved is also likely to play a role. The most frequently used phases for CPS are hydroxyapatite (HA), beta tri-calcium phosphate (β-TCP) and combinations of HA and β-TCP. It is well established that the dissolution rate of calcium phosphate phases is directly related to their Ca/P ratio, TCP with a ratio of 1.5, is more soluble than HA, with a ratio of 1.67. The solubility of the final product can be tuned by using biphasic calcium phosphate (BCP), a combination of HA and α or β-TCP. The solubility of calcium phosphate phases is also affected by ionic substitutions. The HA crystalline structure includes several highly exchangeable sites, with both anionic and cationic substitutions possible. The most studied dopants for hydroxyapatite are Mg 2+ , Si 4+ and Sr 2+ . For a detailed list of ionic substitutions and the mechanism of action of metallic trace elements, the reader is referred to the excellent review by Bose et al. . Briefly, Mg 2+ promotes angiogenesis , Sr 2+ enhances osteogenesis and Si 4+ induces angiogenesis and has been shown to play a key role in mineralization processes . Silicon substitution for phosphorous is also possible with tricalcium phosphate and leads to the stabilization of the high temperature alpha polymorph of TCP, which is more soluble at physiological pH, due to a less compact crystallographic structure . Due to the smaller radius of the silicon ion, silicon for phosphorous substitution in the HA unit cell leads to a distortion of PO 4 tetrahedra. These defects in the crystalline structure are responsible for an increase in solubility. Gibson et al. also showed that silicon doping prevented grain growth in HA ceramics and led to an increase in the temperature needed to achieve adequate sintering . Charge imbalance created by the replacement of PO 4 3− with SiO 4 4− leads to a more electronegative surface, which has been linked to increased surface adhesion . Indeed silicon-doped calcium phosphates have generated tremendous interest due to the clinical confirmation of their important role in the formation of bone and cartilage systems. The degree of Si doping is limited to a maximum of about 2 wt.% for HA, in order to prevent the formation of other calcium silicate phases . This small amount has limited effect on the lattice parameters of Si-HA, which are very similar to those of stoichiometric HA (JCPDS 09-432).
Strontium or magnesium-substituted hydroxyapatites also exhibit greater solubility than undoped HA, with a larger unit cell for Sr-HA and a smaller unit cell for Mg-HA , due to respective ionic radii. The optimal amount of magnesium that can be incorporated in the HA structure is about 7–8% , while larger amounts of strontium can be incorporated, up to a full substitution of strontium for calcium . Combinations of dopants have the potential to synergistically enhance the osteoinductive properties of calcium phosphate ceramics. The highly exchangeable nature of both HA and TCP crystalline structures therefore represents a powerful design tool in bone tissue engineering . Lattice parameters of various doped hydroxyapatites are listed in Table 1 .
| Phase | Space group | Lattice parameters (Å) | Celle volume (Å 3 ) | Reference |
|---|---|---|---|---|
| HA | P 6 3 / m | a = b = 9.4238 Å; c = 6.8854 Å | 1588.6 | |
| Si-HA (0.4 wt.% Si) | P 6 3 / m | a = b = 9.4082 Å; c = 6.8828 Å | 1582.8 | |
| Mg-HA (2 mol.% Mg) | P 6 3 / m | a = b = 9.3938 Å; c = 6.8758 Å | 1576.3 | |
| Sr-HA | P 6 3 / m | a = b = 9.745 Å; c = 7.265 Å | 1792.4 |
1.1.2
Osteoconduction given by scaffold architecture
Osteoconductivity is another highly desirable property for a synthetic bone graft substitute and means that new “bone can grow onto a surface” or volume. To this effect, an ideal scaffold should incorporate macropores of 150–500 μm in diameter and exhibit 60–80% interconnected porosity. This description corresponds to that of open cell or cellular ceramics . The difference between cellular and porous ceramics lies in the interconnectivity of the porous network. In addition to porous bone graft substitutes, cellular ceramics have numerous technological applications, such as filters for molten metals, refractory linings, thermal barriers and heat exchangers . Consequently, a wide palette of processing techniques is available for the production of open cell ceramics. One of the most widely used of these techniques is the replication technique , in which a polymer foam is coated with a well dispersed ceramic slurry. The coated foam is then slowly dried and burned out, leading to an open cell ceramic construct. The choice of polymer is critical as it dictates reproducibility through its modulus of elasticity, it must also burnout with minimal residue. Key processing steps are the slurry optimization, the drying process after slurry impregnation and the burnout/sintering heat treatment. The burnout of the polymer foam occurs in the 300–400 °C temperature range, slow heating rates are therefore recommended in order to prevent the collapse of the green ceramic scaffolds. HA as well as bioglasses and combinations of HA and bioglass scaffolds have been successfully processed using this technique. The polymer foam replication technique is frequently used due to its simplicity; however, major drawbacks are inherent fabrication defects with sharp apices at the center of the hollow struts due to polymer burnout. Fig. 1 shows an uncoated polymer strut ( Fig. 1 A) and a typical defect at the center of a sintered scaffold strut from polymer burnout ( Fig. 1 B). This issue can be addressed by performing a second coating with a lighter ceramic slurry, the resulting characteristic strut is shown in Fig. 1 C, displaying a fully dense strut cross section.

Other green fabrication techniques available for producing open cell ceramics include addition of porogens, foaming and gel casting and rapid prototyping, with a large number of variants . HA inks have been successfully developed for production of 3D scaffolds by direct ink writing . A common final step for all ceramic scaffold production techniques is the firing or sintering step, typically associated with shrinkage, potential crystallization and phase transformation. In this regard, bioactive glasses offer tremendous versatility as their chemical composition can be tailored to widen the sintering window, allowing full sintering to occur prior to the onset of crystallization . Fig. 2 shows how mesenchymal stem cells successfully colonized a glass-ceramic scaffold after 5 weeks of culture.

1.1.3
Osseointegration
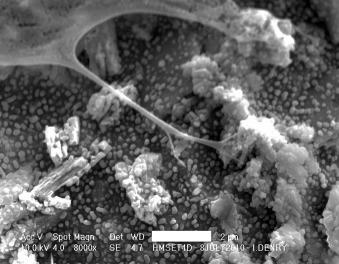
Although CPS are designed to biodegrade over time, they should promote osseointegration, which is defined as the formation of a chemical bond between bone and the surface of an implanted material without formation of fibrous tissue. Osseointegration is promoted by surface charge , wettability, nanotopography , microporosity and hemocompatibility . Seyfert et al. proposed an excellent discussion on in vitro testing of hemocompatibility according to ISO standard 10993-4 and clearly demonstrated the clinical relevance of hemocompatibility testing for implantable devices, while others have shown that every single surface parameter plays a key role in implant/blood interactions . If surface charge and wettability are rather complex to tailor with ceramic materials, nanotopography and microporosity can be easily controlled through thermal treatment by altering heating rate, temperature or duration. Fig. 3 illustrates interaction between a human mesenchymal stem cell (hMSC) and a fluorapatite glass-ceramic at 4 days, facilitated by a microstructure characterized by submicrometer spherical crystals. Fig. 4 illustrates hMSC differentiation into an osteoblastic lineage after 35 days. A fibrillar network is present, together with a spherical nodule consisting of amorphous calcium phosphate.

1.1.4
Delivery of osteogenic factors and anti-infectives by CPS
Strategies to enhance successful bone regeneration by CPS include the addition of growth factors, cytokines, stem cells, and anti-infectives. Given the propensity of CPS to adsorb and concentrate osteoinductive and angiogenic molecules naturally present in the body and thereby enhance bone healing , many of these same factors have been pre-loaded on CPS scaffolds prior to implantation as a means to enhance bone formation. The list of osteogenic factors that have been delivered by CPS for orthopaedic and dental applications is growing and includes bone morphogenetic proteins (e.g. BMP-2, BMP-7) , human growth hormone (hGH) , platelet derived growth factor (PDGF-BB) , transforming growth factor beta-3 (TGF-β3) , fibroblast growth factor-2 (FGF-2) , platelet rich plasma (PRP) and vascular endothelial growth factor (VEGF) . While many CPS-growth factor combinations have been tested in animals, we are only aware of one commercially available CPS-growth factor product used clinically: GEM21S ® (Osteohealth) which delivers PDGF-BB in a controlled manner through the use of a β-TCP delivery vehicle for dental applications.
It is important to use a controlled release delivery vehicle for growth factors because they are proteins that are rapidly denatured if administered systemically. Even more importantly, a delivery system is needed in order to release the growth factor at a low dose locally in a contained manner within the wound site. Growth factors have a broad range of activity on many different cell types throughout the body and uncontrolled non-local administration can lead to tissue malformation associated with painful and life threatening side effects. Complication rates between 10% and 50% have been reported in spine fusion when using BMP-2 delivered from a weakly confining collagen sponge that resulted in ectopic bone formation in and around the spinal canal, post-operative radiculitis, vertebral osteolysis, allergic/hyperinflammatory response, and new malignancies . Growth factor activity is normally tightly regulated in the body through the production of inhibitors, such as growth factor receptor antagonists, e.g. noggin for BMP-2. The artificial delivery of high doses of growth factors instigates the counter productive expression of antagonists, providing further rationale for efficient low dose delivery from biomaterial scaffolds such as CPS.
The final thermal treatment or sintering step during CPS manufacture requires that the addition of osteogenic molecules occur after the structural CPS component is manufactured to avoid destroying their biological activity by the heat. Application of a growth factor as a surface coating is thus the only technique available for combining growth factors with CPS. Simple adsorption of the active biomolecule to the CPS surface was the initial approach used, but that technique is associated with an undesirable burst release . The release kinetics critically affects the biological effects of growth factors and a slow and consistent release is beneficial. To fine tune the release of BMP-2, the surface area and porosity of a commercial sintered biphasic calcium phosphate ceramic was enhanced by applying a biomimetic nanocrystalline apatite coating to increase BMP-2 binding and to slow the release . Another approach to reduce burst release and to enhance growth factor biological effects is to co-precipitate the growth factor within a CaP coating on the CPS by dissolving the growth factor in a simulated body fluid solution and allowing for direct co-precipitation on the CPS. This was demonstrated for BMP-2 and VEGF delivery from CPS by Liu et al. , and Wernike et al. , respectively . Choy et al. increased the degradation of β-TCP ceramics through the incorporation of receptor activator of nuclear factor κ-B ligand (RANKL) using the co-precipitation technique. Superficially adsorbed RANKL did not induce the formation of osteoclasts on β-TCP ceramics in their studies. Overcoat of an additional polymer layer above the adsorbed growth factor, or encapsulation of the growth factor within a polymer that is then applied as a coating to the CPS are other strategies to optimize growth factor delivery from CPS. Polak et al . incorporated BMP-2 within gelatin microspheres and then infiltrated them into micropores on the surface of a porous HA CPS. Fig. 5 demonstrates successful BMP-2 delivery and osseointegration from a biphasic 60% HA/40% β-TCP particulate bone graft substitute combined with a polyethylene glycol hydrogel (HA/TCP/PEG) (Institut Straumann, Basel, Switzerland). The scanning electron micrograph of Fig. 5 A shows the micro and macro-porosity of this product that encouraged new bone tissue growth. The histology image of Fig. 5 B shows new bone tissue growth into the HA/TCP/PEG around a dental implant that was retrieved after 6 weeks from a rabbit mandible as described in Wen et al. . The use of a small amount of polymer as an outer layer, particularly a polymer that does not destroy the biological activity of the growth factors, can enhance the ability of CPS to serve the dual purpose of an osteogenic drug delivery vehicle and scaffold.

Antibiotic delivery from CPS continues to be investigated since infection remains a significant problem associated with orthopaedic and dental surgeries. Silver has antibacterial properties and because of its non-organic nature can be doped into CPS by mixing Ag 2 O with TCP powder and then sintering . Alternatively, AgNO 3 can be dissolved in a calcification solution and then coprecipitated to form a silver containing hydroxyapatite coating on titanium implants . The biomimetic precipitation method has also been used for incorporation and release of cephalothin, carbenicillin, amoxicillin, cefamandol, tobramycin, gentamicin and vancomycin in carbonated HA coatings on titanium alloy plates . The chemical nature and concentration of the antibiotic being incorporated had a significant influence on the carbonated HA coating thickness and thus their release, in addition to their chemical nature. Antibiotics containing carboxylate groups like cephalothin were slower released than others. Kim et al. mixed an antibiotic drug, tetracycline hydrochloride, within a polycaprolactone (PCL)-HA powder combination in a solvent and applied it through dip coating onto a porous HA scaffold. The burst release of antibiotic was reduced and the poor mechanical properties of the highly porous HA scaffold (87%) with pore size of 150–200 μm were enhanced by the PCL-HA coating which blunted or covered the flaws in the CPS. Increased percentage of HA in the coating mixture enhanced release, but decreased the mechanical strength. In a different study, polycaprolactone and polyethylene glycol were mixed and then combined with morselized granules of a corraline calcium carbonate/calcium phosphate CPS and tobramycin sulfate antibiotic and compacted in a mold to form a highly porous biodegradable CPS . This fabrication technique led to a moldable, carvable product with favorable mechanical properties and drug release kinetics providing bactericidal activity to 10 weeks in vitro when polycaprolactone exceeded 98% (w/w) of the total polymer fraction. Drug release in both cases was considerably affected by coating resorption: more degradation leading to more release. A slow degrading polymer coating like polycaprolactone was fine-tuned by the addition of more resorbable CaP powder. One major downside to these coating techniques, as pointed out in the recent and thorough review of the various types of CaP coating techniques with and without growth factors, is that while bioactive hybrid composite CaP-based coatings is an exciting area of research, the adhesion between coating and substrate and high costs related to industrial upscaling are the most influential factors restricting wide spread application of these techniques on a commercial scale .
1.1.5
Cell delivery applications of CPS
Bone regeneration induced by the delivery of mesenchymal stem cells (MSCs) and other progenitor cells currently suffers from a lack of reproducibility for many reasons including donor variability, heterogeneity within the cell source, and loss of multipotency with expansion . Interestingly, animal and human studies have shown that a CPS implantation vehicle can increase the probability of successful bone regeneration outcomes from stem cell-based therapies . In fact, the very first study demonstrating the osteogenic capability of marrow derived MSCs in an ectopic subcutaneous implantation assay used biphasic CPS made of 60% HA and 40% β-TCP . It was concluded that the ceramic graft technique was a sensitive assay for identifying the osteogenic potential of marrow derived stem cells as compared to diffusion chambers in which the cells were not implanted on a CPS. Martin et al. assessed osteogenicity of bone marrow stromal cells treated with FGF-2 prior to seeding on 100% HA scaffolds with 70–80% porosity and the majority of pores greater than 150 μm in an ectopic bone formation assay. They only found consistent new bone formation when cells were implanted on the HA scaffold, bone was never observed if the cells were implanted on a type I collagen sponge. They postulated that the positive results occurred because the mineralized surface of the ceramic served as a primer for the initiation of bone matrix deposition.
As to which CPS is the best to guide the osteogenic differentiation of MSCs, it seems to depend on whether MSCs are seeded on the scaffolds or if the scaffolds are being implanted without cells and endogenous MSCs self-seed the scaffold. For example, Matsushima et al. compared the subcutaneous bone formation in rats from MSCs implanted on HA or β-TCP ceramics and found more bone in the HA ceramic than that in the β-TCP ceramic in 6 of 7 cases. In a comparison study of the scaffolds alone without cells in dogs, rabbits and rats, ectopic bone was most pronounced in the biphasic calcium phosphate ceramics (60 wt% HA and 40 wt% TCP) . Ectopic bone formation without cells reproducibly occurred in dogs, while in rabbits and rats the new tissue formation was mainly limited to osteoid. The mechanism behind the biomaterial-driven osteogenic differentiation of seeded progenitor stem cells was studied by Barradas et al . . They completed in vitro studies with MSCs seeded on both types of materials and reported increased attachment and cell spreading on β-TCP as compared to HA, and induced expression of G-protein coupled receptor 5A associated with protein kinase A signaling pathway, is the earliest evidence of an osteogenic signal from β-TCP. It should be noted that attempts to precondition stem cells in vitro by culturing them in the presence of Ca 2 + and P i supplements resulted in partial or complete abrogation of in vivo ectopic bone formation on CPS indicating that the ions alone are not the predominant mechanism . Wang et al . found that a biphasic CPS (30% hydroxyapatite HA and 70% tricalcium phosphate (β-TCP)) promoted the highest expression of BMP-2 after intramuscular implantation in mice. Tang et al. also found that BMP Smad signaling is active in MSCs affected by osteoinductive CPS. A likely reason for the difference between results from cell seeding studies on CPS versus implantation of naked CPS is due to poor cell viability of cells seeded directly on dry CPS . To enhance survival of MSCs seeded directly on dry CPS, CPS surfaces have been coated with fibronectin and arginine-glycine-aspartic acid (RGD) . The live cell density of scaffolds made with an 0.1% RGD coating was 4× that of the CPS control. Therefore, uncoated HA scaffolds may be better for direct cell seeding than β-TCP since they are less resorbable. During implantation of CPS without cells, the initial contact with blood primes the surface and prepares it for viable in situ cell seeding.
1.2
Scaffold characterization
1.2.1
Scaffold architecture
The unique architecture of open cell ceramics has such a significant impact on their mechanical properties that it becomes critical to fully characterize all structural parameters if any modeling of structure versus properties relationships is to be attempted . Some important parameters include relative density, cell (pore) size and distribution, cell window opening, strut thickness and distribution, strut shape and infrastructure, and degree of anisotropy . The relative density is defined by the ratio of the density of the cellular solid to that of the strut material. True cellular solids have a relative density of less than 0.3.
As indicated earlier, pore size is a critical parameter for CPS. For polymeric foam products, the pore size is often determined by measuring the number of pores per inch on digital micrographs of a sectioned foam, using the well-established linear intercept method. However, this technique is not applicable to CPS for the following reasons: (1) there is no distinction made between pore and window, (2) the pore size will depend on the location of the section, (3) there is likely to be a significant scattering of the data.
Other techniques for determining pore size involve digital image analysis routines. Either optical or scanning electron micrographs can be analyzed and both pore diameter and pore size distribution are derived automatically. However, as for the linear intercept technique, great care should be taken to account for the fact that these images are a 2D projection of a 3D pore structure. Assuming that the pores are spherical, a correction factor of 1.62 can be derived .
Micro computed tomography (micro-CT) permits a more precise representation of pore size, shape and distribution , by providing a complete slice by slice 3D scaffold representation ( Fig. 6 ). The morphometric structure model index (SMI), originally developed to analyze human bone can be used to characterize the 3D architecture of ceramic scaffolds. Mean pore size, surface to volume ratio and strut thickness are obtained via a distance transformation method . In summary, due to the complexity of CPS architecture, micro-CT appears to be the technique of choice for characterization, algorithms developed for human bone morphometric analysis already exist and can be conveniently adapted for CPS analysis.





