Introduction
This study was designed to investigate dentoalveolar compensation in untreated skeletal Class III patients with either positive or negative overjet.
Methods
The positive overjet groups consisted of 104 adults, divided into group 1 (angle between sella-nasion to mandibular plane (SN-MP) > 38°, n = 30), group 2 (30° < SN-MP < 38°, n = 43), and group 3 (SN-MP <30°, n = 31). The negative overjet groups (groups 4-6) consisted of 90 adults who were closely matched to the positive overjet groups with regard to the ANB and SN-MP angles. Twenty-two cephalometric measurements were compared between the matched groups. In the positive overjet groups, correlation analysis was performed between the skeletal and dental measurements, and regression analysis was performed to determine the incisor-mandibular plane angle.
Results
The maxillary incisors were more proclined and the occlusal plane was more flattened in the positive overjet groups than in the negative overjet groups; however, there was no statistically significant difference between them with regard to mandibular incisor inclination. The inclinations of the maxillary and mandibular incisors were correlated with both the sagittal and vertical skeletal measurements. Eight regression equations for the incisor-mandibular plane angle were calculated with the highest coefficient of determination of 0.547.
Conclusions
Proclination of the maxillary incisors and flattening of the occlusal plane contributed to a positive overjet. Mandibular incisor inclination was more closely associated with sagittal and vertical skeletal discrepancies and was not affected by the incisal relationship.
Dentoalveolar compensation refers to a system that attempts to achieve normal interarch relationships with varying skeletal discrepancies. During facial development, full compensatory occlusal development enables normal occlusion despite some variations in skeletal relationships, whereas, in contrast, insufficient compensatory guidance of tooth eruption can lead to malocclusion. Adult patients with a skeletal discrepancy can be treated with orthodontic camouflage or orthognathic surgery, in which proper dentoalveolar compensation or decompensation is required for a successful treatment outcome. Therefore, it would be helpful to understand the physiologic aspects of dentoalveolar compensation in untreated patients with a skeletal discrepancy.
Dentoalveolar compensation varies depending on the sagittal and vertical skeletal discrepancies. Skeletal Class III patients generally show proclination of maxillary incisors and retroclination of mandibular incisors, the degrees of which increase with more severe skeletal discrepancies. With regard to the compensatory inclination of the incisors, some skeletal Class III patients show normal incisor relationships, but others can have a negative overjet, even those with a similar skeletal discrepancy. Ishikawa et al investigated the determinants of positive and negative overjet in skeletal Class I and Class III patients and reported that less compensation of both maxillary and mandibular incisors contributed to a negative overjet. However, the positive and negative overjet groups in that study were not matched in terms of sagittal and vertical skeletal discrepancies, which can significantly affect dentoalveolar compensation.
Traditionally, correct positioning of the mandibular incisors has been considered an important treatment objective, and several cephalometric measurements were developed to this end. However, the population mean cannot be used in patients with skeletal discrepancy because it is derived from a group of ideal occlusions without a skeletal discrepancy. From this perspective, a “floating norm” for the comprehensive analysis of individual craniofacial patterns was proposed and constructed for different facial types. With regard to incisor inclination, Hasund and Ulstein and Segner suggested that dentoalveolar compensation of untreated patients with normal incisor relationships can be used as a guideline for the correction of incisor inclination.
The purposes of this study were 3-fold: (1) to compare the dentoalveolar compensation between positive and negative overjet groups in closely matched skeletal Class III patients, (2) to investigate dentoalveolar compensation in the positive overjet groups according to sagittal and vertical skeletal discrepancies, and (3) to derive floating norms for inclination of the mandibular incisors in patients with specific sagittal and vertical skeletal discrepancies.
Material and methods
This study was performed with the pretreatment lateral cephalograms of selected patients who visited Yonsei University Dental Hospital, Seoul, South Korea, between 2005 and 2013, on the basis of the following criteria: (1) adult skeletal Class III patients (ANB, <0°; age, >18 years for men, and >16 years for women), (2) no previous history of orthodontic treatment, (3) no missing permanent teeth, (4) no systemic or degenerative disease of the temporomandibular joint, and (5) overbite from 0 to 4 mm and overjet from 1 to 4 mm. The 104 patients who met the criteria were all included in the positive overjet group, which was divided into 3 subgroups according to the angle between sella-nasion and the mandibular plane (SN-MP). Group 1 was the hyperdivergent group (SN-MP >38°; n = 30), group 2 was the normodivergent group (30° < SN-MP < 38°; n = 43), and group 3 was the hypodivergent group (SN-MP <30°; n = 31).
As the control group, in which the patients had a negative overjet of less than 0 mm, 90 patients were selected from the same pool of untreated patients based on the same inclusion criteria except the criterion relating to overjet. The control group was divided into groups 4 through 6 (n = 30 per group) according to SN-MP angle and matched as closely as possible to groups 1 through 3, respectively, with regard to ANB for sagittal skeletal discrepancy and SN-MP for vertical skeletal discrepancy. The characteristics of the patients in the positive and negative overjet groups are shown in Table I .
| Hyperdivergent group | Normodivergent group | Hypodivergent group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | Range | Mean | SD | Range | Mean | SD | Range |
| Group 1 (n = 30) | Group 2 (n = 43) | Group 3 (n = 31) | |||||||
| Positive overjet groups | |||||||||
| Age (y) | 20.20 | 4.09 | 16 to 34 | 23.28 | 4.78 | 17 to 35 | 24.56 | 9.41 | 17 to 52 |
| ANB (°) | −1.20 | 1.35 | −5.25 to –0.01 | −1.43 | 1.05 | −4.8 to –0.05 | −2.31 | 1.61 | −6.85 to –0.18 |
| SN-MP (°) | 40.56 | 2.36 | 38.03 to 46.16 | 34.43 | 1.87 | 31.03 to 37.22 | 27.08 | 2.52 | 21.01 to 29.88 |
| Group 4 (n = 30) | Group 5 (n = 30) | Group 6 (n = 30) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Negative overjet groups | |||||||||
| Age (y) | 20.73 | 3.5 | 16 to 29 | 22.47 | 5.18 | 16 to 35 | 22.07 | 4.59 | 17 to 41 |
| ANB (°) | −0.94 | 0.66 | −2.37 to –0.08 | −1.39 | 0.95 | −2.96 to –0.01 | −2.19 | 1.41 | −4.78 to 0.03 |
| SN-MP (°) | 40.66 | 2.18 | 38.08 to 47.09 | 34.33 | 2.07 | 30.31 to 37.12 | 27.27 | 2.51 | 19.14 to 29.97 |
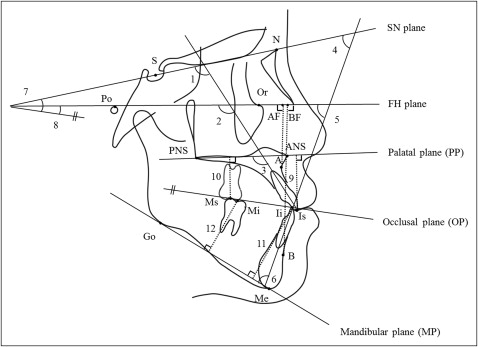
Pretreatment lateral cephalograms were acquired using a Cranex3+ Ceph (Soredex, Milwaukee, Wis) machine with 10% magnification and traced using V-ceph software (version 5.5; OSSTEM, Seoul, South Korea), all by the same examiner (S.-J.K.). Double images were traced using midpoints between 2 images. The cephalometric measurements are illustrated in the Figure .
Statistical analysis
All measurements were performed twice, 2 weeks apart, by the same examiner. A paired t test was conducted on the paired measurements to quantify the reproducibility of the measurements. Method errors were calculated using Dahlberg’s formula, Se = √(d 2 /2n), where d is the difference between measurements, and n is the number of pairs of measurements.
The 2-sample t test was used to compare the measurements of the positive overjet groups (1-3) with those of the negative overjet groups (4-6). The Pearson correlational analysis was used to investigate correlations between skeletal measurements and dental measurements within the positive overjet groups. Multiple linear regression analysis was used to determine floating norms for mandibular incisor inclination in the positive overjet groups using the incisor-mandibular plane angle (IMPA) as the dependent variable and 2 skeletal measurements, one from the sagittal and the other from the vertical skeletal measurements, as the independent variables. Statistical evaluations were performed at the 5% level of significance with SPSS software for Windows (version 18.0; SPSS, Chicago, Ill).
Results
The paired t test showed no statistically significant difference between the measurements made 2 weeks apart. The method errors were 0.47 to 0.87 mm for linear measurements and 0.59° to 0.95° for angular measurements.
There was no statistically significant difference in ANB, SN-AB, AF-BF, SN-MP, FMA, or AB-MP between the positive overjet groups and the corresponding negative overjet groups, indicating that they were closely matched in terms of sagittal and vertical skeletal discrepancies. The Wits appraisal and anteroposterior dysplasia indicator (APDI) differed significantly between the 2 groups because they depend on the occlusal plane angle and the palatal plane angle, respectively ( Table II ).
| Measurement | Hyperdivergent groups | Normodivergent groups | Hypodivergent groups | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Positive overjet (group 1) | Negative overjet (group 4) | P value | Positive overjet (group 2) | Negative overjet (group 5) | P value | Positive overjet (group 3) | Negative overjet (group 6) | P value | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Skeletal measurements | |||||||||
| Anteroposterior | |||||||||
| ANB (°) | −1.20 (1.35) | −0.94 (0.66) | 0.352 | −1.43 (1.05) | −1.39 (0.95) | 0.879 | −2.32 (1.61) | −2.19 (1.41) | 0.789 |
| SN-AB (°) | 80.50 (3.33) | 80.71 (2.48) | 0.363 | 83.18 (3.02) | 84.01 (2.03) | 0.216 | 87.60 (3.64) | 87.70 (3.58) | 0.824 |
| AF-BF (mm) | −0.67 (2.61) | −1.61 (2.41) | 0.153 | −1.63 (2.40) | −2.45 (2.01) | 0.132 | −4.07 (2.96) | −5.23 (2.51) | 0.107 |
| Wits (mm) | −8.36 (2.72) | −10.65 (2.54) | 0.001 † | −6.88 (2.03) | −10.04 (2.46) | <0.001 ‡ | −7.21 (2.21) | −9.53 (2.12) | <0.001 ‡ |
| APDI (°) | 90.07 (3.32) | 93.60 (2.77) | <0.001 ‡ | 92.08 (3.34) | 94.45 (3.61) | 0.005 † | 94.46 (3.51) | 96.51 (3.61) | 0.028 ∗ |
| Vertical | |||||||||
| SN-MP (°) | 40.56 (2.36) | 40.66 (2.18) | 0.866 | 34.43 (1.87) | 34.33 (2.07) | 0.833 | 27.08 (2.52) | 27.27 (2.51) | 0.875 |
| FMA (°) | 30.35 (3.30) | 30.10 (3.17) | 0.762 | 25.65 (3.16) | 25.46 (2.69) | 0.791 | 19.53 (2.81) | 18.33 (3.12) | 0.092 |
| PP-MP (°) | 30.99 (4.29) | 28.28 (3.79) | 0.012 ∗ | 25.35 (3.10) | 23.92 (3.74) | 0.078 | 20.24 (4.42) | 18.43 (2.87) | 0.065 |
| SN-PP (°) | 9.57 (3.60) | 12.37 (2.81) | 0.001 † | 9.08 (3.19) | 10.41 (2.81) | 0.069 | 6.83 (3.55) | 8.84 (2.78) | 0.023 ∗ |
| AB-MP (°) | 58.94 (3.69) | 58.12 (3.32) | 0.370 | 62.39 (2.94) | 61.66 (2.56) | 0.276 | 65.34 (3.88) | 65.03 (3.37) | 0.742 |
| Dental measurements | |||||||||
| Inclination | |||||||||
| U1-SN (°) | 110.54 (5.87) | 105.83 (3.97) | 0.001 † | 113.76 (5.78) | 106.83 (4.63) | <0.001 ‡ | 117.08 (6.26) | 109.22 (5.52) | <0.001 ‡ |
| U1-FH (°) | 120.78 (6.37) | 116.05 (4.25) | 0.003 † | 122.53 (4.77) | 115.69 (5.30) | <0.001 ‡ | 124.63 (5.64) | 118.15 (5.91) | <0.001 ‡ |
| U1-PP (°) | 120.11 (6.53) | 118.28 (3.47) | 0.156 | 122.88 (5.38) | 117.24 (4.76) | <0.001 ‡ | 123.91 (6.84) | 118.05 (5.05) | <0.001 ‡ |
| IMPA (°) | 82.76 (7.20) | 83.72 (3.98) | 0.524 | 86.38 (5.60) | 86.50 (5.12) | 0.928 | 90.30 (6.85) | 91.68 (6.38) | 0.498 |
| FMIA (°) | 66.89 (6.40) | 66.12 (4.37) | 0.587 | 67.97 (6.05) | 68.04 (4.53) | 0.955 | 70.17 (6.95) | 70.01 (6.43) | 0.923 |
| L1-SN (°) | 56.68 (6.79) | 54.57 (3.27) | 0.443 | 59.19 (5.91) | 59.17 (4.83) | 0.990 | 62.62 (6.65) | 61.08 (6.71) | 0.466 |
| SN-OP (°) | 19.42 (3.28) | 21.11 (2.47) | 0.029 ∗ | 15.17 (3.43) | 17.92 (2.59) | <0.001 ‡ | 11.58 (2.79) | 14.37 (3.05) | 0.001 † |
| FH-OP (°) | 9.22 (3.04) | 10.91 (3.06) | 0.116 | 6.39 (2.85) | 9.01 (2.75) | <0.001 ‡ | 4.03 (2.36) | 5.43 (3.47) | 0.079 |
| Height | |||||||||
| U1-PP (mm) | 32.74 (2.61) | 32.31 (3.25) | 0.573 | 32.00 (2.46) | 31.61 (2.73) | 0.525 | 30.54 (3.53) | 30.59 (2.98) | 0.962 |
| U6-PP (mm) | 26.03 (2.26) | 26.19 (2.66) | 0.808 | 27.38 (2.49) | 26.42 (2.54) | 0.110 | 26.42 (2.54) | 25.97 (2.55) | 0.481 |
| L1-MP (mm) | 45.06 (3.25) | 46.47 (4.59) | 0.174 | 45.55 (3.71) | 45.93 (3.96) | 0.679 | 44.98 (4.21) | 44.93 (3.41) | 0.936 |
| L6-MP (mm) | 32.94 (2.58) | 35.51 (4.08) | 0.005 † | 34.63 (2.95) | 36.29 (3.43) | 0.030 ∗ | 35.10 (3.78) | 36.76 (3.33) | 0.087 |
In terms of dental compensation, U1-SN, U1-FH, and U1-PP were significantly higher in the positive overjet groups than in the negative overjet groups; the maxillary incisors were more proclined in the positive overjet groups. In contrast, IMPA, FMIA, and L1-SN did not differ significantly between the positive and negative overjet groups ( Table II ).
The occlusal plane angle, assessed with SN-OP and FH-OP, was significantly lower in the positive overjet groups than in the negative overjet groups. Among the heights of the incisors and molars, the only measurement that differed significantly was the height of the mandibular first molar, which was significantly less in the positive overjet groups. Although the height of the maxillary first molar did not differ significantly between the positive and negative overjet groups, the palatal plane angle, SN-PP, was significantly smaller in the positive overjet groups ( Table II ).
Correlational analyses showed that the inclinations of the maxillary and mandibular incisors were significantly correlated with the sagittal and vertical skeletal discrepancies, with varying correlational coefficients. With regard to the inclination of maxillary incisors, U1-SN, U1-FH, and U1-PP were negatively correlated with ANB, AF-BF, SN-MP, FMA, and PP-MP, and positively correlated with SN-AB, the Wits appraisal, and APDI, showing that the maxillary incisors were more proclined with a more severe sagittal skeletal discrepancy and a more hypodivergent facial profile. The inclination of the mandibular incisors was measured in relation to the mandibular inferior border, IMPA, and horizontal reference line, FMIA, and L1-SN. With regard to the sagittal skeletal discrepancy, analysis of IMPA, FMIA, and L1-SN showed that the mandibular incisors were more retroclined with a more severe sagittal skeletal discrepancy. With regard to the vertical skeletal discrepancy, the mandibular IMPA was associated with a more hyperdivergent facial profile. However, FMIA was not significantly correlated with any vertical skeletal measurements except FMA, and L1-SN was only significantly correlated with SN-MP. Flattening of the occlusal plane was associated with a more severe sagittal skeletal discrepancy and a more hypodivergent facial profile ( Table III ).
| Correlation coefficient | ANB (°) | SN-AB (°) | AF-BF (mm) | Wits (mm) | APDI (°) | SN-MP (°) | FMA (°) | SN-PP (°) | PP-MP (°) | AB-MP (°) |
|---|---|---|---|---|---|---|---|---|---|---|
| U1-SN (°) | −0.243 ∗ | 0.591 ‡ | −0.302 † | 0.130 | 0.385 ‡ | −0.441 ‡ | −0.196 ∗ | −0.303 † | −0.246 ∗ | −0.011 |
| U1-FH (°) | −0.199 ∗ | 0.356 ‡ | −0.446 ‡ | 0.103 | 0.369 ‡ | −0.267 † | −0.302 † | −0.025 | −0.249 ∗ | −0.004 |
| U1-PP (°) | −0.116 | 0.285 † | −0.194 ∗ | 0.205 ∗ | 0.553 ‡ | −0.276 † | −0.210 ∗ | 0.256 † | −0.434 ‡ | 0.079 |
| IMPA (°) | 0.312 † | −0.110 | 0.177 | 0.549 ‡ | −0.018 | −0.468 ‡ | −0.482 ‡ | 0.116 | −0.537 ‡ | 0.733 ‡ |
| FMIA (°) | −0.546 ‡ | 0.425 ‡ | −0.638 ‡ | −0.436 ‡ | 0.373 ‡ | −0.155 | −0.271 † | −0.112 | −0.083 | −0.223 ∗ |
| L1-SN (°) | −0.591 ‡ | 0.677 ‡ | −0.528 ‡ | −0.384 ‡ | 0.416 ‡ | −0.346 ‡ | −0.192 | −0.379 ‡ | −0.103 | −0.224 ∗ |
| SN-OP (°) | 0.360 ‡ | −0.775 ‡ | 0.368 ‡ | −0.350 ‡ | −0.389 ‡ | 0.736 ‡ | 0.414 ‡ | 0.528 ‡ | 0.397 ‡ | −0.197 ∗ |
| FH-OP (°) | 0.341 ‡ | −0.476 ‡ | 0.654 ‡ | −0.380 ‡ | −0.392 ‡ | 0.566 ‡ | 0.675 ‡ | 0.146 | 0.469 ‡ | −0.272 † |
Regression analysis with IMPA as a dependent variable showed that all regression models and independent variables attained statistical significance with variance inflation factors less than 2, indicating that there was no multicollinearity problem. The regression model with ANB, AB-MP, and the Wits appraisal as independent variables showed the highest adjusted coefficient of determination, 0.547, indicating that approximately 54.7% of the variation in IMPA could be explained by these independent variables ( Table IV ). The correlational coefficients between skeletal measurements are shown in Table V .



