Figure 2.27 Male, 44 years old. Born in Bosnia, immigrated to Sweden 24 years ago. Referred to orofacial pain specialist from general practitioner due to TMJ pain and sounds.
B. Symptom History
- Today, pain from right TMJ at rest, movement, and chewing.
- Chewing and mouth opening worsens the pain. Rest, diclofenac and ibuprofen may decrease the pain.
- Pain intensity varies between 1 (at rest) and 5 (on chewing hard food) on a 0–10 NRS.
- Characteristic pain intensity 10 (NRS 0–100), current pain intensity 1 (NRS 0–10), pain-related disability 23 (NRS 0–100; GCPS).
- JFLS reveals limitation in mouth opening and chewing. No apparent daytime parafunctions according OBCL.
- No headache. No neck pain.
- Grating sounds from the right TMJ.
- Debut with grating sounds in the right TMJ 7 years ago. Since 2 years ago, intermittent pain as described earlier from the right TMJ and increasing grating sounds.
- Trauma to the left side of the face at a soccer game 12 years ago. Initially pain in the right TMJ and mouth opening difficulties that subsided during 2 weeks.
- Six months ago the patient noticed occlusal changes with a gradual loss of occlusal contacts, especially in the front. Today, no contacts in the front.
C. Medical History
- Hypothyreosis.
- Diffuse and undiagnosed knee joint pains.
- Medication: diclofenac a few times a week against the knee and TMJ pain.
D. Psychosocial History
- Married, three children (21, 15, and 12 years of age).
- Works as a chef in a high school; enjoys his work but finds it very stressful. Few sick-leave days in general.
- In his spare time: house renovation, gym, family, and friends.
- Describes himself as person that easily gets stressed and with inadequate stress management. Mild scores for depression (PHQ-9) and anxiety (GAD-7). Some physical symptoms (PHQ-15; 7 p) but moderate level of stress (PSS-10). Normal catastrophizing (Patient Catastrophizing Scale (PCS)). Good sleep quality (PSQI).
- GCPS grade I; that is, low pain intensity and low disability.
- No smoking, moderate alcohol consumption.
E. Previous Consultations and Treatments
- Several visits to this general dental practitioner. Tried splint but with limited success.
F. Extraoral Status
Asymmetries
- No apparent swelling or other facial asymmetries. No redness. No increased skin temperature over either TMJ.
Somatosensory abnormalities
- Normal findings bilaterally for the trigeminal nerve regarding touch, cold. and pinprick.
Temporomandibular joint
- Familiar palpation pain on the right side. Normal translatory movement on both sides. Familiar pain from the right TMJ on mouth opening; laterotrusion to both sides and on protrusion.
- Palpable crepitus from the right TMJ.
Masticatory muscles
- Familiar palpation pain in right masseter and temporalis muscle. No referred pain.
Jaw movement capacity
- Maximum mouth opening without pain is 29 mm, maximum unassisted opening is 45 mm with familiar pain in right TMJ, and maximum assisted mouth opening is 50 mm with familiar pain in the right TMJ. Right laterotrusion 14 mm (no familiar pain), left laterotrusion 10 mm with familiar pain in the right TMJ and masseter muscle, and protrusion 9 mm with familiar pain in the right TMJ.
Neck examination
- Normal range of motion; no familiar neck pain on movement or palpation.
G. Intraoral Status
Soft tissues
- Normal findings.
Hard tissues and dentition
- Complete dentition (except for 46) with some fillings.
Occlusion
- Dentition: 17–27, 37–45, 47. Hard occlusion shows contacts on the following teeth in the upper jaw: 17, 24–27 (Figure 2.28).
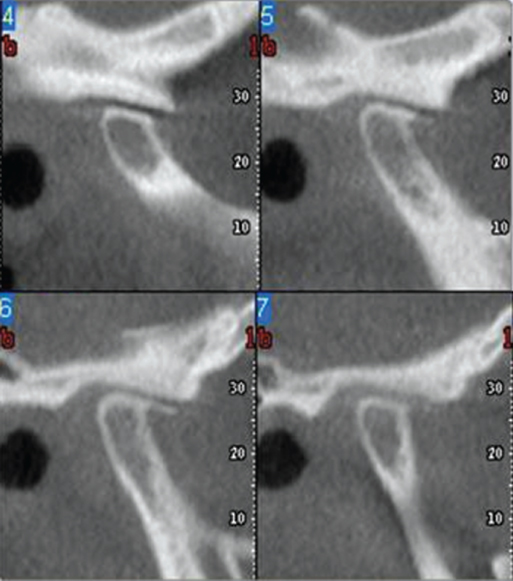
Figure 2.28 Dentition: 17–27, 37–45, 47. Hard occlusion shows contacts on the following teeth in the upper jaw: 17, 24–27.
H. Additional Examinations and Findings
- CBCT of the right TMJ shows condyle and temporal eminence flattening, v-shaped temporal eminence, condylar bone loss, and condylar osteophytes (Figure 2.29). Normal findings on the left side.
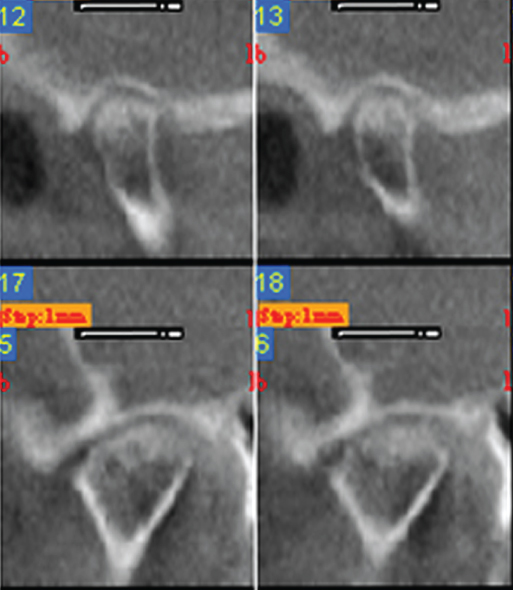
Figure 2.29 CBCT of the right TMJ shows condyle and temporal eminence flattening, v-shaped temporal eminence, condylar bone loss, and condylar osteophyte. Normal findings on the left side.
I. Diagnosis/Diagnoses
DC/TMD
- Right TMJ degenerative joint disease.
- Arthralgia in the right TMJ.
- Myalgia of the masticatory muscles.
Expanded DC/TMD
- Arthritis, right TMJ.
J. Case Assessment
- Degenerative joint disease in the right TMJ with a probable secondary arthritis due to the finding of arthralgia, including TMJ pain on mandibular movements (see Case 2.2).
- Radiographic examination shows typical signs of degenerative joint disease in the right TMJ: condyle and temporal eminence flattening, v-shaped temporal eminence, condylar bone loss, and condylar osteophytes, supporting the diagnosis of degenerative joint disease.
- Minor masticatory muscle myalgia that was not part of the main complaint. However, it may point to a muscle tension situation that in turn may have contributed to the degenerative joint disease by excessive TMJ loading.
- Bone tissue changes in combination with the ongoing inflammatory activity in the right TMJ are a likely cause of the changes in occlusion.
K. Evidence-based Treatment Plan including Aims
- After information and counselling, the first priority is to stop the inflammatory activity in the right TMJ. The aim would be to eliminate the pain and the ongoing cartilage and bone tissue destruction in the joint. See Case 2.2 for detail. In overview, anti-inflammatory treatment (intraarticular corticosteroids or NSAIDs) supplemented with a treatment modality that has the possibility to reduce the risk of a relapse of the arthritis. For example, jaw exercise.
- When the inflammatory activity is substantially reduced and under control, the occlusal changes should be addressed. The aim for this part should be adequate chewing ability and stable, comfortable occlusion. Treatment options range from no treatment and natural normalization of the occlusion, via occlusal adjustment, prosthodontic therapy, orthodontic therapy, surgery, or combinations of these. The goal here must be increased or normalized chewing capacity. Also, the treatment should be minimal since there is an increased risk of future arthritic episodes that may have the possibility to further change the occlusion.
L. Prognosis and Discussion
- The prognosis is very much dependent on how well it will be possible to stop the inflammatory activity. The supposedly long duration of arthritis, including pain and later occlusal changes due to the bone tissue destruction, is a negative prognostic factor. The short-term prognosis for treatment of arthritis must be considered as good, especially if intraarticular corticosteroids are used. However, the long-term prognosis is unclear and depends on how well the inflammation will be controlled, also over time.
Background Information
- Degenerative joint disease is primarily a noninflammatory progressive and degenerative cartilage disease resulting in degradation of load-bearing cartilage tissue and remodeling of underlying bone tissue. However, the etiology of the majority of TMJ degenerative joint disease is complex and multifactorial or unknown.
- The terms degenerative joint disease, osteoarthritis, osteoarthrosis, and arthrosis are often used interchangeably. In DC/TMD, these terms have all been replaced with the umbrella term “degenerative joint disease.” Future research will hopefully clarify this matter.
- Degenerative joint disease is frequently associated with arthritis. This association is bidirectional; that is, degenerative joint disease can cause arthritis and arthritis can cause degenerative joint changes.
- Degenerative joint disease can initiate and maintain a secondary arthritis due to an intraarticular discharge of short cartilage collagen fragments from the damaged cartilage surface. These fragments may be discharged as part of the degenerative process or by joint movement and loading, especially if the cartilage surface is damaged. Short collagen fragments cause inflammation by an unspecific immune system reaction. Indeed, one commonly used animal model of rheumatoid arthritis uses intraarticular injections of short collagen fragments to cause chronic arthritis.
- Degenerative joint disease is the most common joint disease with a prevalence in the TMJ of 8–16% in the general population. The prevalence increases with age but is also related to genetic factors, disc displacement, loss of molar support, trauma, and loading, where loading can both prevent and contribute to degenerative joint disease.
- Given the limited understanding of its pathogenesis and the low healing potential of avascular cartilage, no effective therapy is available for restoring the structures of TMJ with progressive osteoarthritis.
(De Souza et al., 2012; Wang et al., 2015; Ahmad and Schiffman, 2016)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


