A 19-year-old woman with skeletal Class III malocclusion, paranasal depression, and a low mandibular plane angle was treated with orthodontics and orthognathic surgery. Dental decompensation and protraction of maxillary right third molar to replace maxillary right second molar were performed before surgery. Clockwise rotation of maxillo-mandibular complex was applied by Le Fort I osteotomy and bilateral sagittal split osteotomies to achieve facial balance. The active treatment period was 12 months. The stable occlusion and skeletal relationship were observed after a 10-month follow-up period.
Treatment for an adult patient with skeletal Class III malocclusion requires dentoalveolar compensation or combined orthodontic and surgical procedures, with the aim to achieve normal occlusion and improve facial esthetics. In conventional treatment planning for orthognathic surgery, the anteroposterior discrepancies are corrected by advancement or setback of the jaws along the existing occlusal plane. When vertical change of the maxilla is required, the mandible will autorotate; as a consequence of this rotation, the occlusal plane angle will be altered. This principle does not always produce optimal esthetic results. When change of the occlusal plane is required for esthetic considerations, the maxilla and the mandible will rotate together according to the new defined occlusal plane. Reyneke et al stated that when a patient needs an occlusal plane change of more than +2°, the situation is significant enough to be considered a deliberate clockwise rotation case. This treatment design, also known as alteration of the occlusal plane or the rotation of the maxillomandibular complex, is often indicated in patients who have excessively high or low mandibular plane angles. The objective of this article was to present the treatment of a skeletal Class III malocclusion in a patient with paranasal depression and a low mandibular plane angle. The clockwise rotation of maxillo-mandibular complex provided good maxillary incisor exposure and excellent smile arc, and improved the patient’s facial balance.
Diagnosis and etiology
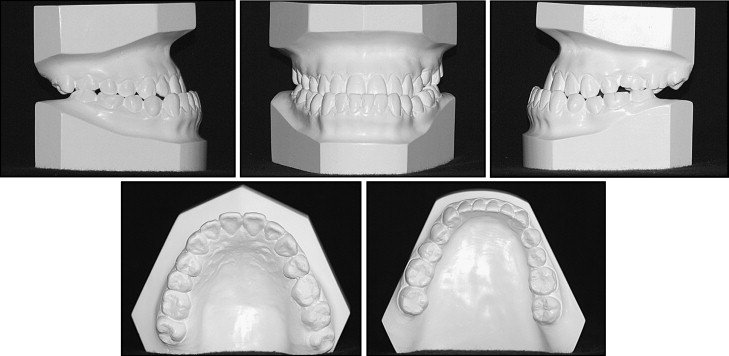
A Taiwanese woman (age, 19 years 6 months) came for treatment with no history of trauma or serious illness. She reported her inability to incise food and had esthetic concerns with her long and dished-in face ( Figs 1-3 ). She had received orthodontic treatment and interproximal enamel reduction of her mandibular incisors during her childhood. The maxillary left second premolar was extracted at an early age, and the maxillary left first molar had drifted mesially. The prognathic mandible was responsible for the dished-in face and the Class III malocclusion.

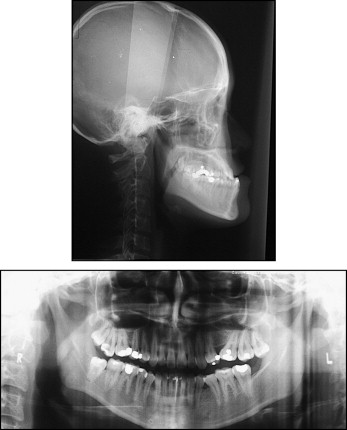
The patient had a Class III skeletal malocclusion with severe mandibular prognathism, a low mandibular plane angle, and excessive lower facial height (especially from stomion to soft-tissue menton). The lips were incompetent, and the incisor-stomion distance was 2 mm. The lower lip was strained to compensate for the vertical discrepancy, and this stretch eliminated the labiomental sulcus. Infraorbital rim positions appeared to be in good relationship to the globe. Also noted were a paranasal depression and an acute nasolabial angle ( Figs 1 and 3 , Table ).
| Measurement | Pretreatment | Posttreatment | Norm |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 86 | 85.5 | 84.2 ± 3.2 |
| SNB (°) | 92 | 85 | 81.2 ± 3.0 |
| ANB (°) | −6 | 0.5 | 2.9 ± 1.9 |
| NAPg (°) | −12 | 2 | 5.4 ± 4.9 |
| A-Nv (mm) | 1 | 2 | 0 ± 3.0 |
| Pg-Nv (mm) | 16 | 4 | −5.8 ± 5.6 |
| Wits (mm) | −15 | −7 | −1 ± 1 |
| SN-OP (°) | 6 | 18 | 16 ± 2 |
| SN-MP (°) | 22 | 26 | 27.8 ± 6.2 |
| UFH/LFH (%) | 43.5/56.5 | 44/56 | 45/55 |
| Dental factor | |||
| U1-SN (°) | 120 | 106 | 110 ± 5.6 |
| U1-NA (°/mm) | 6/34 | 4.5/23 | 24/5 |
| U1-L1 (°) | 157 | 128 | 121.9 ± 10.5 |
| L1-NB (°/mm) | 1.5/14 | 7/29 | 27/6 |
| L1-MP (°) | 74 | 95 | 99.2 ± 6.8 |
| Soft tissue | |||
| NLA (°) | 84 | 102 | 92.9 ± 7.4 |
| E-line (mm) | −6 | 1 | −0.67 ± 1.8 |
| Upper lip/lower lip | 0 | 1.5 | 0.93 ± 2.16 |
| Sn-ST/ST-Me | 20:48 | 22:46 | 1:2 |
| Chin throat length (mm) | 58 | 48 | 57 ± 6 |
She had a dental Class III malocclusion with an overbite of 3.5 mm and a negative overjet of 5 mm. Her maxillary incisors were tipped labially of their bony base, and the mandibular incisors were tipped lingually. Bilateral posterior and anterior crossbites were present. The absence of the maxillary left second premolar aggravated the deviation of her maxillary dental midline. The mandibular midline was coincident with the facial midline. The maxillary right second molar had a large temporary restoration with subgingival caries. The periodontal tissues were healthy ( Figs 1-3 , Table ).
Treatment objectives
- 1.
Maxilla. Rotate the maxillomandibular complex clockwise, correct the insufficient dentogingival display and the paranasal depression, eliminate the acute nasolabial angle, and assist the sagittal coordination with mandible.
- 2.
Mandible. Rotate the maxillomandibular complex clockwise, reduce the lower facial height, correct the prognathism and the dental malocclusion, and shape the bilateral gonial angle because of the bony ledge after clockwise rotation of maxillomandibular complex.
- 3.
Maxillary dentition. Substitute the maxillary right third molar for the largely decayed maxillary right second molar, coordinate the facial and maxillary dental midlines, resolve the proclined incisor position, and achieve ideal overbite and overjet relationships.
- 4.
Mandibular dentition. Remove dental compensation by placing the mandibular incisors more upright over the basal bone. Level, align, and coordinate with the maxillary arch.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


