This report describes a novel concept of 3-dimensional tooth movement by using biocreative therapy to provide unrestricted distal movement of the full mandibular dentition. The patient was a 26-year-old Korean woman with multiple problems, including a collapsed occlusion, a full-step Class III relationship with posterior open bite, a crossbite, temporomandibular joint pain, and a tendency for root resorption. Two orthodontic miniplates with tubes were initially placed on both retromolar pads for distalization; 1 miniplate was relocated to the anterior region for angulation and vertical control of the anterior teeth. The total treatment period was 13 months. The occlusion was finished in Class I molar and canine relationships with optimal overjet and overbite. Posttreatment records 2.5 years later showed a stable treatment outcome. The results suggest that an orthodontic miniplate is an efficient tool for the treatment of a collapsed occlusion by changing the affected arch only.
Patients with collapsed arches tend to have altered tooth positions; typical signs can include migration of adjacent teeth into the spaces, midline deviation, loss of vertical dimension, flaring of anterior teeth, and a multi-occlusal plane. An efficient treatment strategy essentially aims to resolve the vertical and anteroposterior problems of each segment separately while simultaneously shortening the treatment duration.
Within the last decade, the use of mini-implants as temporary skeletal anchorage devices has greatly expanded the boundaries of orthodontic tooth movement, especially for adult patients who do not want to wear extraoral appliances or undergo surgery. However, mini-implants have been associated with fairly high failure rates, including fracture during placement, loosening under loading, and root injury. Liou et al reported that mini-implants do not remain stationary under orthodontic forces and suggested that a safety zone for root or nerve proximity might be required. This could further restrict possible placement sites or limit the amount of tooth movement. In contrast, miniplates have an advantage because their fixation screws are generally placed apically to the roots and so do not interfere with tooth movement. They might provide more secure anchorage when higher forces, such as orthopedic forces, are needed. Placement of miniplates is more complex than mini-implants because flap elevation should be required by a surgeon. However, miniplates might be preferred for patients who are planned to have en-masse movement of an entire arch by more than 2 mm or extensive orthopedic corrections, or the force vectors need to be varied.
Biocreative therapy (C-therapy) was developed to target the patient’s chief complaint by using a variety of temporary skeletal anchorage devices without the unwanted side effects of conventional orthodontic biomechanics. This treatment concept was developed by partially osseointegrated mini-implants or plates that can easily endure multi-directional heavy forces even when they support orthodontic archwires.
This case report describes the use of biocreative therapy to correct a collapsed occlusion in a patient with degenerative joint disease focused on the mandibular arch. One miniplate was relocated during treatment. This technique provided maximum treatment efficiency by reducing the cost of multiple mini-implants and the overall orthodontic treatment duration.
Diagnosis and etiology
A 26-year-old Korean woman was referred from a local clinic with a chief complaining of chewing difficulty because of her collapsed occlusion ( Figs 1 and 2 ). She had worn an occlusal splint on the mandibular arch for 13 months, and orthodontic fixed appliances (MBT, 3M Unitek, Monrovia, Calif) were placed in the maxillary arch with 4 anterior mini-implants. Three were installed on the buccal side and 1 on the left palatal side for intrusion of the anterior teeth. The mini-implant on the right buccal side was bent because of poor placement. Initial and previous treatment records were not available. Temporomandibular joint symptoms had subsided, and no centric relation-centric occlusion discrepancy was seen at retreatment.

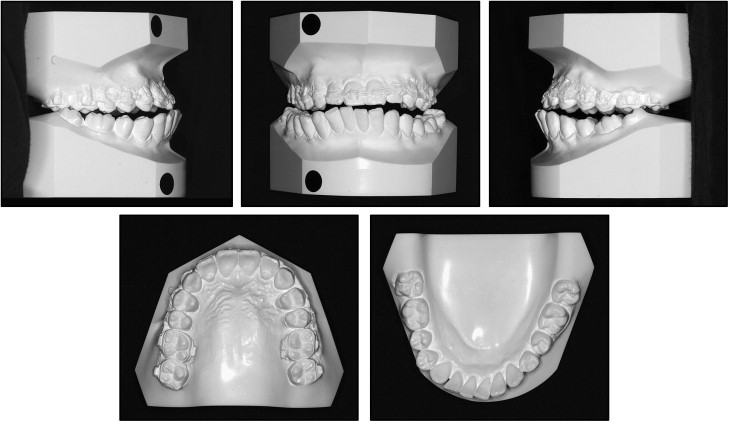
The patient had a straight profile and good facial proportions, but with asymmetry to the left side. The intraoral examination showed a full-step Class III malocclusion with a posterior open bite, anterior and posterior crossbites, occlusal canting, and a deep curve of Spee. The mandibular molars were significantly inclined mesially, especially on the left side. The mandibular anterior teeth were also inclined toward the right, and the midline of the mandibular arch was shifted 4.5 mm to the right. There was occlusal contact only at the right distal end ( Fig 2 ).
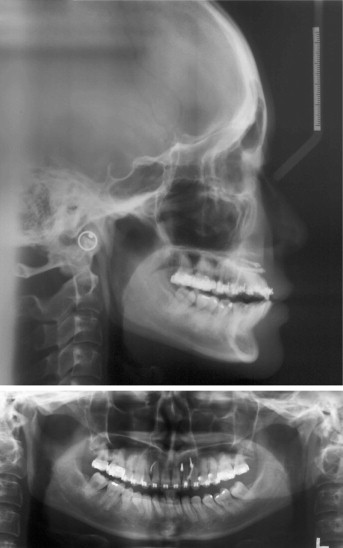
A panoramic radiograph showed root resorption of the maxillary anterior teeth and short roots in the premolar and mandibular anterior regions. A degenerative bony change of the left condyle was found ( Fig 3 ). Cephalometric analysis showed a skeletal Class I relationship (ANB, 0.6°) and a hypodivergent vertical pattern (FMA, 20.0°). Although the maxillary incisors had a normal labiolingual inclination (U1-FH, 116.3°), the mandibular incisors showed an excessive proclination (IMPA, 115.8°) ( Fig 3 , Table ).
| Average (female) | Pretreatment | Posttreatment | 2.5 years retention | |
|---|---|---|---|---|
| SNA (°) | 81.6 | 78.6 | 79.2 | 79.4 |
| SNB (°) | 79.2 | 78.0 | 77.3 | 77.4 |
| ANB (°) | 2.4 | 0.6 | 1.9 | 2.0 |
| PFH/AFH (%) | 66.8 | 68.6 | 68.5 | 68.5 |
| Sum (°) | 395.7 | 387.7 | 387.4 | 387.3 |
| FMA (°) | 24.3 | 20.0 | 20.2 | 20.4 |
| SN-MxOP (°) | 17.9 | 17.0 | 17.1 | 17.0 |
| SN-PP (°) | 10.2 | 13.2 | 13.0 | 13.1 |
| FH-UI (°) | 116.0 | 116.3 | 112.0 | 111.9 |
| IMPA (°) | 95.9 | 115.8 | 99.3 | 99.8 |
| FMIA (°) | 59.8 | 44.8 | 59.5 | 59.3 |
| Interincisal angle (°) | 123.8 | 104.5 | 121.2 | 121.0 |
| UL-E plane (mm) | −0.9 | −2.2 | −1.8 | −1.6 |
| LL-E plane (mm) | 0.6 | −1.8 | −6.0 | −6.1 |
| Nasolabial angle (°) | 98.0 | 97.0 | 100.0 | 100.2 |
Treatment objectives
The patient was diagnosed with skeletal Class I, dental Class III with facial asymmetry, crossbite, posterior open bite, and temporomandibular disorder. The treatment objectives were to (1) correct the molar and canine relationships to a Class I relationship, (2) achieve optimal overjet and overbite, (3) achieve a functional Class I occlusion, and (4) maintain the facial balance.
Treatment alternatives
Based on those objectives, 2 treatment options were proposed. The ideal treatment option involved surgery to correct the skeletal asymmetry. However, the patient adamantly refused orthognathic surgery. She planned to marry in 1 year and did not want the treatment to interfere. Therefore, she accepted the second treatment option, which required the use of temporary skeletal anchorage devices (C-tube plates) to distalize the entire mandibular arch to correct the molar relationship, overjet, and overbite without involving extractions. The patient was informed that this process would include several stages: (1) upright and distalize the mandibular posterior teeth, (2) upright and retract the mandibular anterior teeth, (3) intrude the mandibular anterior teeth for vertical control, and (4) coordinate the maxillary and mandibular arches to achieve ideal overbite and overjet for the final detailing.
Treatment objectives
The patient was diagnosed with skeletal Class I, dental Class III with facial asymmetry, crossbite, posterior open bite, and temporomandibular disorder. The treatment objectives were to (1) correct the molar and canine relationships to a Class I relationship, (2) achieve optimal overjet and overbite, (3) achieve a functional Class I occlusion, and (4) maintain the facial balance.
Treatment alternatives
Based on those objectives, 2 treatment options were proposed. The ideal treatment option involved surgery to correct the skeletal asymmetry. However, the patient adamantly refused orthognathic surgery. She planned to marry in 1 year and did not want the treatment to interfere. Therefore, she accepted the second treatment option, which required the use of temporary skeletal anchorage devices (C-tube plates) to distalize the entire mandibular arch to correct the molar relationship, overjet, and overbite without involving extractions. The patient was informed that this process would include several stages: (1) upright and distalize the mandibular posterior teeth, (2) upright and retract the mandibular anterior teeth, (3) intrude the mandibular anterior teeth for vertical control, and (4) coordinate the maxillary and mandibular arches to achieve ideal overbite and overjet for the final detailing.
Treatment progress
The patient stopped wearing the splint, and 4 mini-implants in the anterior region were removed. Fixed appliances were placed in the mandibular arch with segmental approaches. The anterior (incisors and canines) and 2 posterior (premolars and molars) regions were leveled separately. Two I-type C-tube plates (Jin Biomed, Bucheon, Korea) were placed bilaterally in the retromolar area ( Fig 4 ). Each was fixed with 2 drill-free miniscrews (diameter, 1.5 mm; length, 5 mm). The placement procedures were described in a previous article. Molar uprighting generated a significant interdental space between the canine and first premolar, which was to be used for retraction of the anterior dentition. After 5 months, positive overjet and overbite were achieved, and the mandibular right molars are fully distalized into a Class I molar relationship. Then the temporary skeletal anchorage device in the right retromolar area was relocated to the left anterior region to solve the occlusal plane canting caused by the overerupted mandibular left incisors ( Fig 5 , A-C ). Relocation is a unique characteristic of C-therapy for maximum efficiency and minimum use of temporary skeletal anchorage devices. First, the miniscrews were unscrewed, and the C-tube plate on the right retromolar pad was removed. The surface of the removed C-tube plate was gently but copiously irrigated with saline solution, and it was bent along the bone contour of anterior region. The C-tube plate was reused, but the miniscrew was replaced with a new, shorter one (diameter, 1.5 mm; length, 4 mm) to prevent fatigue fracture during reimplantation into the cortical bone and adjacent root damage, although that possibility was remote.




