Coronal Approach
|
|
The coronal or bitemporal incision is a versatile surgical approach to the upper and middle regions of the facial skeleton, including the zygomatic arch. It provides excellent access to these areas with minimal complications (1). A major advantage of this approach is that most of the surgical scar is hidden within the hairline. When the incision is extended into the preauricular area, the surgical scar is inconspicuous.
SURGICAL ANATOMY
Layers of the Scalp
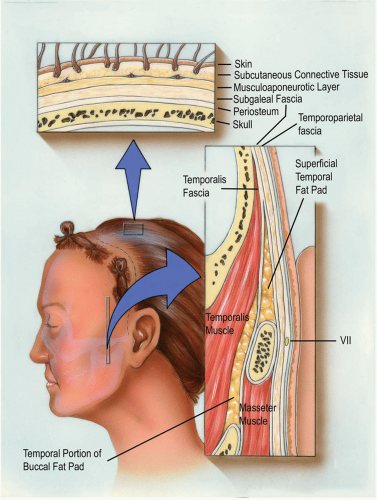
The basic mnemonic for the layers of the scalp (see Fig. 6.1) is “SCALP”: S, skin; C, subcutaneous tissue; A, aponeurosis and muscle; L, loose areolar tissue; P, pericranium (periosteum).
The skin and subcutaneous tissue of the scalp are surgically inseparable, unlike these same structures elsewhere in the body. Many hair follicles and sweat glands are found in the subcutaneous fat just beneath the dermis. In addition, no easy plane of cleavage exists between the subcutaneous fat and the musculoaponeurotic layer.
The musculoaponeurotic layer, also inappropriately called the galea (which refers to aponeurosis only), consists of the paired frontalis (epicranius) and occipitalis muscles, the auricular muscles, and a broad aponeurosis. The aponeurosis is the true galea and has two portions, an extensive intermediate aponeurosis between the frontalis and occipitalis muscles and a lateral extension into the temporoparietal region, which is known as the temporoparietal fascia. Farther inferiorly, the temporoparietal fascia is continuous with the superficial musculoaponeurotic system (SMAS) of the face. The paired frontalis muscles originate from the galeal aponeurosis and insert into the dermis at the level of the eyebrows. An extension of the galea separates the two quadrilateral frontalis muscles in the midline of the forehead.
The galea is a dense, glistening sheet of fibrous tissue, approximately 0.5 mm thick, stretching between the occipitalis and frontalis muscles. When the galea moves, the skin and fat move with it because they are closely attached. Laterally, the galea (or temporoparietal fascia, as it is usually called) becomes less dense but is still readily dissectible. The superficial temporal artery lies on or in this layer.
The subgaleal fascia is the layer usually referred to as the loose areolar layer or the subaponeurotic plane. This layer cleaves readily, allowing the skin, subcutaneous tissue, and musculoaponeurotic layers to be stripped from the pericranium. It is in this fascial plane that cleavage occurs during traumatic avulsion of the scalp. The loose tissue of the subgaleal fascia allows for free movement of the skin over the periosteum when the frontalis muscle is contracted. Anatomic dissections have also revealed that the subgaleal fascia can be mobilized as an independent fascial layer. For the routine coronal approach to the facial skeleton, however, this fascial layer is used only for its ease of cleavage.
Anteriorly, the subgaleal fascia is continuous with the loose areolar layer deep to the orbicularis oculi muscles. Laterally, it is attached to the frontal process of the zygoma. This attachment continues along the superior surface of the zygomatic arch, above the external auditory meatus, and over the mastoid process. It terminates by fusing with the periosteum along the superior nuchal line.
The pericranium is the periosteum of the skull. It can be elevated from the skull, although it is more firmly attached along cranial sutures. When released by subperiosteal dissection, the pericranium retracts owing to its elasticity.
Layers of the Temporoparietal Region
The temporoparietal fascia is the most superficial fascial layer beneath the subcutaneous fat (Fig. 6.1). Frequently called the superficial temporal fascia or the suprazygomatic SMAS, this fascial layer is the lateral extension of the galea and is continuous with the SMAS of the face (see Fig. 6.2). Because the fascia is just beneath the skin, it may go unrecognized after incision. The blood vessels of the scalp, such as the superficial temporal vessels, run along the outer aspect of the fascia, adjacent to the subcutaneous fat. The motor nerves, such as the temporal branch of the facial nerve, run on its deep surface.
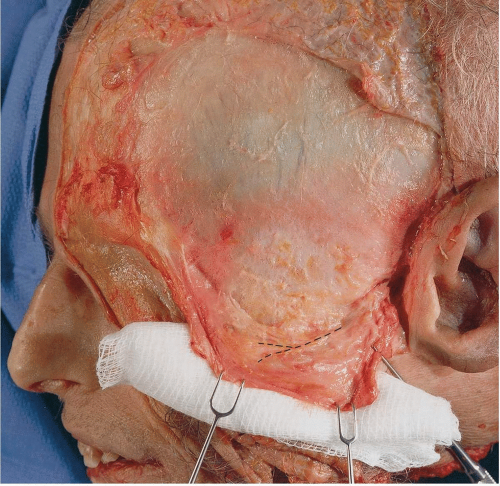
The subgaleal fascia in the temporoparietal region is well developed and can be dissected as a discrete fascial layer, although it is used only as a cleavage plane in the standard coronal approach (Fig. 6.2).
The temporalis fascia is the fascia of the temporalis muscle. This thick layer arises from the superior temporal line, where it fuses with the pericranium (Fig. 6.1). The temporalis muscle arises from the deep surface of the temporalis fascia and the whole of the temporal fossa. At the level of the superior orbital rim, the temporalis fascia splits, with the superficial layer attaching to the lateral border and the deep layer attaching to the medial border of the zygomatic arch. A small quantity of fat, sometimes called the superficial temporal fat pad, separates the two layers. Dissection through the medial layer
of the temporalis fascia reveals another layer of fat, the temporal portion of the buccal fat pad, which is continuous with the other portions of the buccal fat pad of the cheek below the zygomatic arch. This fat pad separates the temporalis muscle from the zygomatic arch and from the other muscles of mastication, allowing a smooth gliding motion while functioning.
of the temporalis fascia reveals another layer of fat, the temporal portion of the buccal fat pad, which is continuous with the other portions of the buccal fat pad of the cheek below the zygomatic arch. This fat pad separates the temporalis muscle from the zygomatic arch and from the other muscles of mastication, allowing a smooth gliding motion while functioning.
Temporal Branch of Facial Nerve
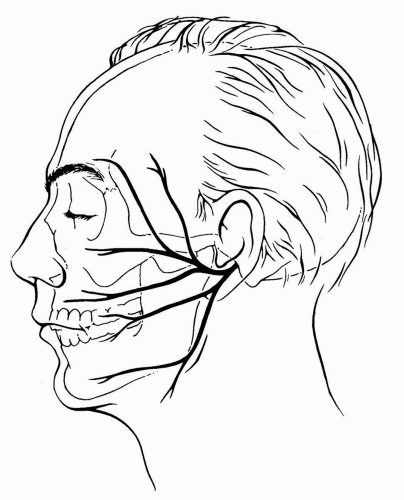
The temporal branches of the facial nerve are often called the frontal branches when they reach the supraciliary region. The nerves provide motor innervation to the frontalis, to the corrugator, to the procerus, and occasionally, to a portion of the orbicularis oculi muscles. Nerve injury is revealed by the inability to raise the eyebrow or wrinkle the forehead.
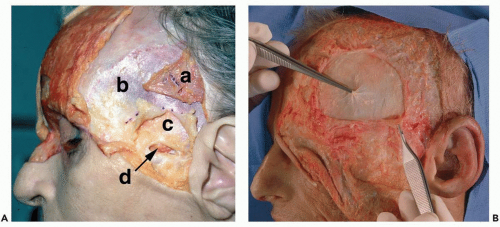
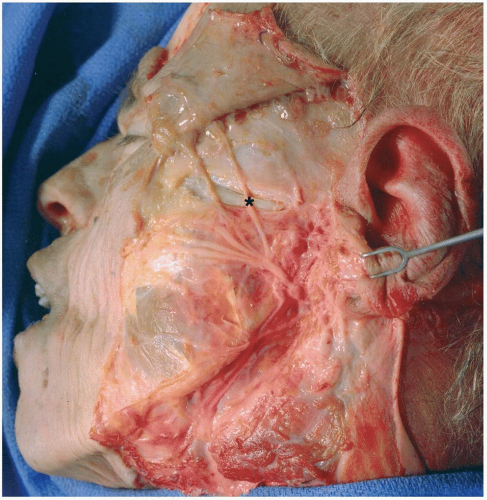
The temporal branch or branches of the facial nerve leave the parotid gland immediately inferior to the zygomatic arch (see Fig. 6.3). The general course is from a point 0.5 cm below the tragus to a point 1.5 cm above the lateral eyebrow (2). It crosses superficial to the zygomatic arch at an average distance of 2 cm anterior to the anterior concavity of the external auditory canal, but in some cases it is as near as 0.8 cm or as far as 3.5 cm anterior to the external auditory canal (see Fig. 6.4) (3). As the temporal branch crosses the lateral surface of the arch, it courses along the undersurface of the temporoparietal fascia, between it and the fusion of periosteum of the zygomatic arch, the superficial layer of temporalis
fascia, and the subgaleal fascia (Fig. 6.1). As the nerve courses anterosuperiorly toward the frontalis muscle, it lies on the undersurface of the temporoparietal fascia (see Fig. 6.5) and enters the frontalis muscle no more than 2 cm above the level of the superior orbital rim. It usually branches into three or four rami along its course. The anterior branches supply the superior portion of the orbicularis oculi muscle and the frontalis muscle. The posterior branch innervates the anterior auricular muscles.
fascia, and the subgaleal fascia (Fig. 6.1). As the nerve courses anterosuperiorly toward the frontalis muscle, it lies on the undersurface of the temporoparietal fascia (see Fig. 6.5) and enters the frontalis muscle no more than 2 cm above the level of the superior orbital rim. It usually branches into three or four rami along its course. The anterior branches supply the superior portion of the orbicularis oculi muscle and the frontalis muscle. The posterior branch innervates the anterior auricular muscles.
The Medial Orbit
The medial orbital wall is composed of several bones: the frontal process of the maxilla, the lacrimal bone, the lamina papyracea of the ethmoid, and part of the lesser wing of the sphenoid. In terms of function, the medial orbit can be divided into anterior, middle, and posterior thirds.
Anterior One Third of the Medial Orbital Wall
The medial orbital rim and the anterior one third of the medial orbit comprise the frontal process of the maxilla, the maxillary process of the frontal bone, and the lacrimal bone. The lacrimal fossa for the lacrimal sac lies between the anterior and posterior lacrimal crests. The anterior crest is a continuation of the frontal process of the maxilla. The posterior lacrimal crest is an extension of the lacrimal bone. The bone of the lateral nasal wall contains the nasolacrimal
duct, which enters the nasal cavity through the inferior meatus located beneath the inferior turbinate.
duct, which enters the nasal cavity through the inferior meatus located beneath the inferior turbinate.
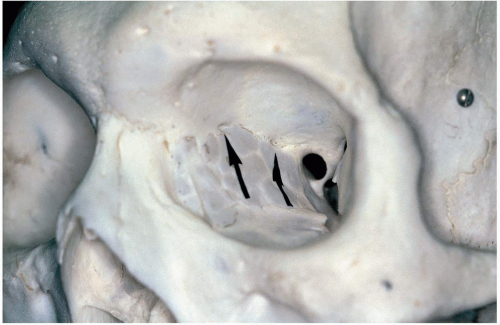
Middle One Third of the Medial Orbital Wall
The middle one third of the medial orbital wall, largely made of the lamina papyracea of the ethmoid bone, is thin, but it is reinforced by the buttress effect of the ethmoid air cells. The only vascular structures of any significance are the anterior and posterior ethmoidal arteries. The foramina for the anterior and posterior ethmoid arteries and nerves are found in, or just above, the frontoethmoid suture line at the level of the cribriform plate. The anterior ethmoid foramen is located approximately 24 mm posterior to the anterior lacrimal crest (4) (see Fig. 6.6). The posterior ethmoid foramen or foramina (25% are multiple) are located approximately 36 mm posterior to the anterior lacrimal crest (4). The optic canal is located approximately 42 mm posterior to the anterior lacrimal crest. The distance between the posterior ethmoidal artery and the optic nerve is variable, but it is never less than 3 mm (4).
Posterior One Third of the Medial Orbital Wall
The posterior part of the orbit is made of thick bone surrounding the optic foramen and superior orbital fissure.
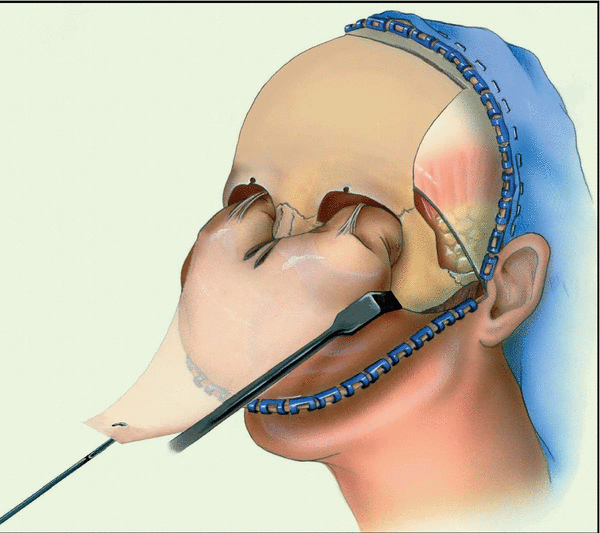
TECHNIQUE
The coronal approach can be used to expose different areas of the upper and middle face. The layer of dissection and the extent of exposure depend on the particular surgical procedure for which the coronal approach is used. In some instances, it may be prudent to perform a subperiosteal elevation of the coronal flap from the point of incision. The periosteum is freed with a scalpel along the superior temporal lines as one proceeds anteriorly with the dissection, leaving the temporalis muscles attached to the skull. In most cases, however, dissection and elevation of the coronal flap are in the easily cleavable subgaleal plane. The deeper pericranium may be used as a separate vascularized coronal flap for defect coverage. For illustrative purposes, the following description of the complete exposure of the upper and middle face, including the zygomatic arch, using a subgaleal dissection for most of the flap elevation is given.
▶ Step 1. Locating the Incision Line and Preparation
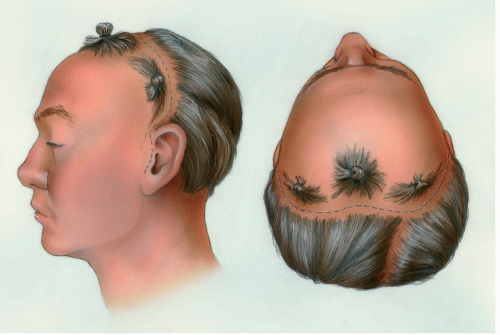
Two factors are considered when designing the line of incision. The first is the hairline of the patient. In men, hairline recession at the widow’s peak and the lateral temporal valleys should be considered. For balding men, the incision might be placed along a line extending from one preauricular area to the other, several centimeters behind the hairline (see Fig. 6.7), or even more posteriorly. Incisions made further posteriorly need not reduce access to the operative field because the extent of skeletal exposure depends on the inferior extent of the incisions and not on the anteroposterior position. In men who are not balding and in most women, the incision may be curved anteriorly at the vertex, paralleling but remaining 4 to 5 cm within the hairline (see Fig. 6.8). In children, the incision is preferably placed well behind the hairline to allow for migration of the scar with growth. In black patients with short hair, keloid formation is also a concern. Zigzag incisions may be used to make the scars less noticeable. If a hemicoronal incision is planned, the incision curves forward at the midline, ending just posterior to the hairline. Curving the hemicoronal incision anteriorly provides the relaxation necessary for the retraction of the flap.
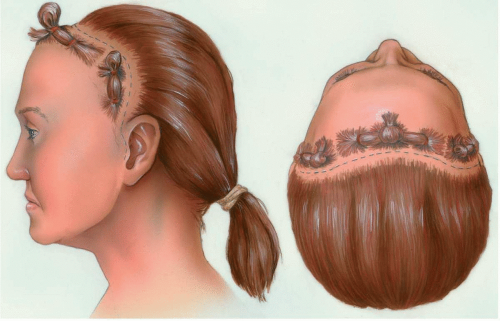
Figure 6.8 Incision placement for most female patients and for those male patients with no signs or family history of baldness. The incision is kept approximately 4 cm behind the hairline.
|
The second factor considered while designing the location of the incision is the extent of inferior access required for the procedure. When exposure of the zygomatic arch is unnecessary, extending the coronal incision inferiorly to the level of the helix may be all that is necessary. However, the coronal incision can be extended inferiorly to the level of the earlobe as a preauricular incision. This maneuver allows exposure of the zygomatic arch, temporomandibular joint (TMJ), and/or infraorbital rims.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses